SYNOPSIS
Objectives.
This study was conducted to estimate the burden of non-canine-related bite and sting injuries in the U.S.; describe the affected population, injury severity, and bite or sting source; and provide considerations for prevention strategies.
Methods.
Data were from the 2001 through 2004 National Electronic Injury Surveillance System-All Injury Program (NEISS-AIP) (a stratified probability sample of U.S. hospitals). Records included information about age, body part affected, cause, diagnosis, disposition, and gender. Narrative descriptions were coded for the source of the bite or sting.
Results.
Between 2001 and 2004, an estimated 3.6 million people were treated in emergency departments for injuries related to non-canine bites and stings. Results detail the reported sources of the bite or sting, and examine sources by gender and age group. Common sources included bees (162,000 cases annually), spiders (123,000 cases annually), and cats (66,000 cases annually). Female adults were more likely than male adults to be treated for cat bites. Although rare, of the known venomous snakebites, more than half (58.4%) of the patients were hospitalized.
Conclusions.
Our results demonstrate the public health burden of non-canine-related bite and sting injuries. More than 900,000 people were treated in emergency departments annually for non-canine bite or sting injuries, or roughly 1.7 injuries per minute. Treatment consumes substantial health-care resources. While preventing these injuries should be the first line of defense, resources could be conserved by educating the public about immediate first aid and when warning signs and symptoms indicate the need for professional or emergency care.
Bite and sting injuries from insects, spiders, and cats may initially appear to be benign, yet they can lead to wound infection, pain, disfigurement, allergic reactions, tissue damage, disease, and even death. Zoonotic diseases that can be transmitted from animals to humans through bites include cat scratch disease, rat bite fever, and rabies. Mosquitoes and ticks are associated with potentially debilitating or life-threatening vector-borne diseases including West Nile virus and Lyme disease, respectively.1
The literature on bites and stings predominately reports regional estimates of exposure,2–6 management of specific injuries,7–9 and case reports of infectious diseases and injuries resulting from exposure to wild or domesticated animals.10–12 Detailed nationally based estimates of the burden of non-canine-related bite and sting injuries treated in emergency departments (EDs) have not been previously reported. We present these estimates along with descriptive data regarding the affected population, the severity of the injury, the source responsible for the bite or sting, and considerations for prevention strategies. This information should be useful in guiding public health and health-care practitioners' knowledge base regarding the prevention and control of bite and sting injuries.
METHODS
Study design and setting
The National Electronic Injury Surveillance System (NEISS) is an ongoing surveillance system used to monitor consumer product-related injuries treated in U.S. hospital EDs. The system is maintained and operated by the U.S. Consumer Product Safety Commission (CPSC). There are currently 100 NEISS hospital EDs that represent a stratified probability sample of all U.S. and U.S. territory hospitals that have at least six beds and provide 24-hour emergency services. NEISS is particularly sensitive to detect emerging injury problems. The NEISS is also adaptable: as a new mechanism of injury is detected, a new code is created, which then allows the injury type to be tracked.
The National Electronic Injury Surveillance System-All Injury Program (NEISS-AIP) is a subsample of NEISS consisting of 66 hospitals. NEISS-AIP tracks all injuries seen in EDs whether or not they are associated with consumer products, and as such is a source of nationally representative data on injuries. For this project, NEISS-AIP data were analyzed for a four-year period from 2001 through 2004.
NEISS-AIP is a collaborative effort of the Centers for Disease Control and Prevention's (CDC's) National Center for Injury Prevention and Control (Injury Center) and the CPSC, and has been described in more detail in previously published reports.13,14 It has been widely used in reports of intentional15,16 and unintentional injuries.17–20
For each case, NEISS coders collected the following information from the ED medical record: age, gender, injury diagnosis, body part injured, ED discharge disposition, location where the injury occurred (e.g., home, street/highway), work-relatedness, and intentionality (i.e., unintentional, assault, suicide attempt, or unknown intent) of the injury event. In addition, a two-line narrative describing circumstance and treatment of injuries was recorded.
Cases were defined as people treated at an NEISS-AIP hospital for a bite or sting injury and were included if intent was coded as unintentional or undetermined. Those who were dead on arrival or who died in the ED were excluded because mortality data are not fully captured by NEISS-AIP. Dog and human bites, and bites or stings incurred at work or during active military duty were excluded from these analyses. CDC's Injury Center researchers have addressed the issue of dog bites in recent reports.21 Human bites were excluded because they are considered intentional injuries. Work-related bites and stings were excluded because risk, exposure, and prevention are different from that of the general population and would most likely involve on-the-job safety precautions. The total unweighted sample size across the four years was substantial (n=62,098).
Methods of measurement
The narrative descriptions were coded for the source of the bite or sting using text string queries. Fifty percent of the source coding was then rechecked to further verify the accuracy of the coding. Inaccuracies, typically due to spelling errors in the narratives, were corrected manually.
Anaphylactic signs and symptoms were abstracted in a similar fashion to the source of bite or sting variable by using a text string query and examining the comment line for verification. The anaphylaxis abstraction was limited to cases in which a person was bitten by an insect, ant, bee, wasp, hornet, and/or yellow jacket. A subject was coded as having anaphylaxis signs and symptoms if one of the following was recorded in the narrative description: anaphylaxis, use of epi-pen, or ED treatment of epinephrine. Additionally, subjects were coded as having anaphylaxis signs and symptoms if two or more of the following were listed in the narrative description: gastrointestinal symptoms (e.g., nausea, vomiting, or diarrhea), respiratory symptoms (e.g., wheezing, difficulty breathing, shortness of breath, or chest tightness), cardiovascular symptoms (e.g., drop in blood pressure, increased heart rate, or shock), generalized dermatologic symptoms (e.g., generalized hives, generalized swelling, or swelling of the throat, lips, or tongue), or other symptoms (e.g., sudden weakness or loss of consciousness). Approximately 15% of the records coded as having anaphylactic signs or symptoms stated anaphylaxis explicitly in the comment narrative and 3% noted use of an epi-pen/epinephrine. The remaining 82% of cases coded as having anaphylactic signs or symptoms were based upon having two or more of the noted symptoms.
There are six possible categories for case disposition: treated and released, transferred to another facility (e.g., trauma center), hospitalized, observed (i.e., held for observation), left without being seen, or unknown. Given the small number of cases in the latter three categories, they were combined in the analyses. Cases that were transferred were combined with cases that were hospitalized in NEISS-AIP and are referred to in the text as hospitalized.
Data analysis
National annual estimates and percentages were based on weighted data. A sample weight was calculated by the CPSC for each injured person treated at an NEISS hospital on the basis of the inverse of the probability of selection of that hospital in each stratum. In addition, sample weights were poststratified by the annual number of ED visits over time. The adjustment applied to the basic NEISS-AIP weight was the ratio of the known total number of ED visits in the population (from the most recent hospital database) over the estimate of the total ED visits based on the sample of NEISS-AIP hospitals.22 Rates were calculated using U.S. Census Bureau 2001 through 2004 bridged race population estimates available on the Web-based Injury Statistics Query and Reporting System (WISQARS).23
Injury estimates were identified as unstable if the national estimate was <1,200, the number of sample cases used was <20, or coefficient of variation (CV) was >30%, where CV = (standard error [SE] / national estimate) × 100.14 Analyses were conducted with SPSS Complex Samples. Comparisons are presented by gender and age group (<18 and ≥18) as well as by body part with 95% confidence intervals (CIs).
RESULTS
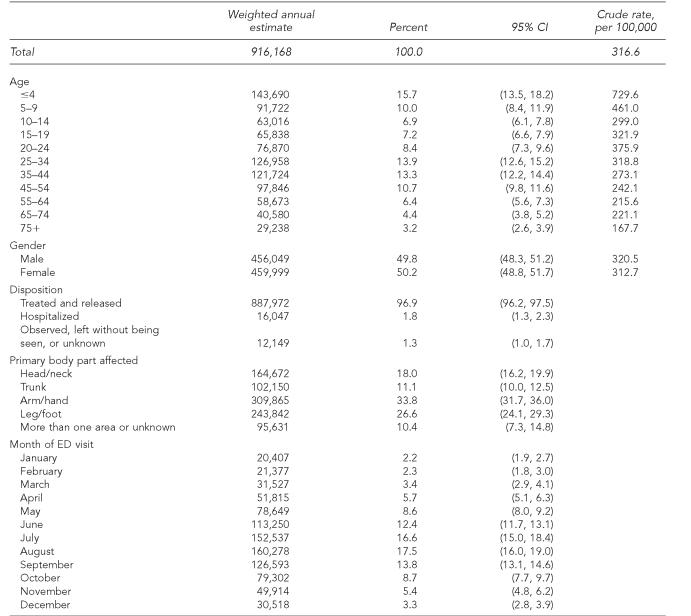
Between 2001 and 2004, an estimated 916,168 people were treated in U.S. EDs annually for non-canine bite or sting injuries, including more than 140,000 bites or stings sustained by children ages 0–4 years (Table 1). This number totals more than an estimated 3.6 million people treated in U.S. EDs for injuries related to non-canine bites and stings over the course of four years. The crude rate of bite or sting injuries was 316.6 per 100,000 population per year. The bite or sting rates were highest among the younger age groups (crude rate = 729.6 per 100,000 for children aged 0–4 years per year; crude rate = 167.7 per 100,000 for adults aged ≥75 years per year). Overall, there were no differences by gender.
Table 1.
Annual estimates of nonfatal unintentional bite and sting injuries treated in emergency departments, by age, gender, disposition, primary body part affected, and month of visit, U.S., 2001–2004 (weighted n=3,664,671)a
Excludes canine, human, and work-related bite or sting injuries
ED = emergency department
CI = confidence interval
Nearly all cases were treated and released (96.9%; 95% CI 96.2, 97.5) and few cases (1.8%; 95% CI 1.3, 2.3) were hospitalized. Bites and sting injuries were most likely to occur to the extremities of the body (hand or arm 33.8%; 95% CI 31.7, 36.0; foot or leg 26.6%; 95% CI 24.1, 29.3). Bites and stings occurred most frequently during the summer months, with approximately two-thirds (60.3%) of the injuries occurring between June and September.
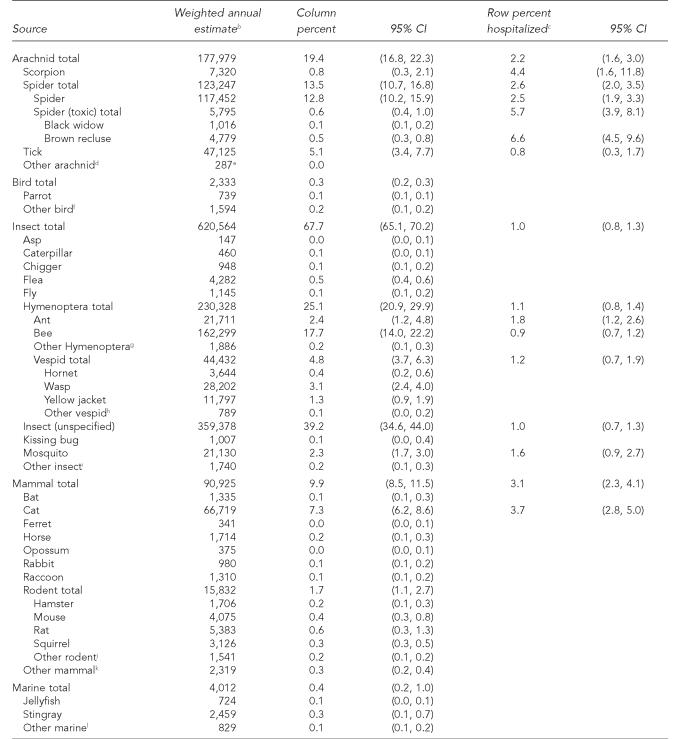
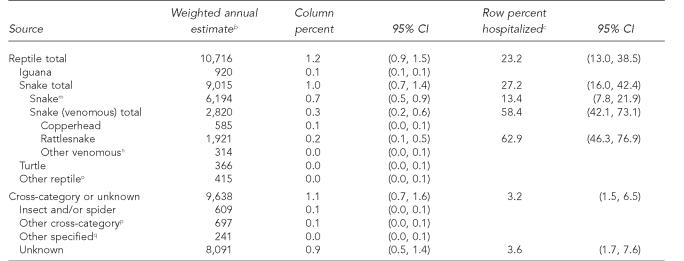
The source of the bite or sting reported most frequently was unspecified insect (39.2%; 95% CI 34.6, 44.0) (Table 2). Other common sources included bees (17.7%; 95% CI 14.0, 22.2), spiders (12.8%; 95% CI 10.2, 15.9), and cats (7.3%; 95% CI 6.2, 8.6). Less than 1% of the bee sting, 2.5% of the spider bite, and 3.7% of the cat bite patients were hospitalized. More than 15,000 people were treated for rodent bites annually. Although rare, of the 2,820 known venomous snakebites, more than half (58.4%; 95% CI 42.1, 73.1) of the patients were hospitalized.
Table 2.
Source of nonfatal unintentional bite and sting injuries treated in emergency departments, U.S., 2001–2004 (weighted n=3,664,671)a
Excludes canine, human, and work-related bite and sting injuries
Column values for groupings may not sum due to rounding.
Percent hospitalized for each source is only reported for cases when the estimate is considered statistically stable.
Other arachnid includes more than one arachnid source.
Estimates might be unstable because the number of sample cases was <20.
Other bird includes: chicken, cockatiel, cockatoo, duck, goose, macaw, parakeet, rooster, seagull, and unspecified bird.
Other Hymenoptera includes more than one Hymenoptera source.
Other vespid includes more than one vespid source.
Other insect includes: centipede, cockroach, gnat, lice, mite, no-see-um, pinworms, scabies, sand flea, and more than one insect source.
Other rodent includes: chipmunk, gerbil, gopher, groundhog, guinea pig, muskrat, porcupine, prairie dog, river rat, woodchuck, more than one rodent source, and unspecified rodent.
Other mammal includes: badger, bear, bobcat, burro, coati mundi, cow, coyote, donkey, fox, goat, hedgehog, hog, javelina, mink, mole, monkey, mountain lion, mule, otter, pig, sea lion, seal, shrew, skunk, wolf, and unspecified animal.
Other marine animal includes: crab, fish, lobster, piranha, sea anemone, sea urchin, shellfish, shark, and unspecified marine organism.
Snake includes all nonvenomous or unidentified snakes.
Other venomous snake includes cottonmouth, water moccasin, and unspecified venomous.
Other reptile includes: alligator, gecko, and lizard.
Other cross-category includes more than one source that was cross-species (e.g., flea and cat).
Other specified includes: asp (when it could not be determined if snake or insect), leech, worm, and slug.
CI = confidence interval
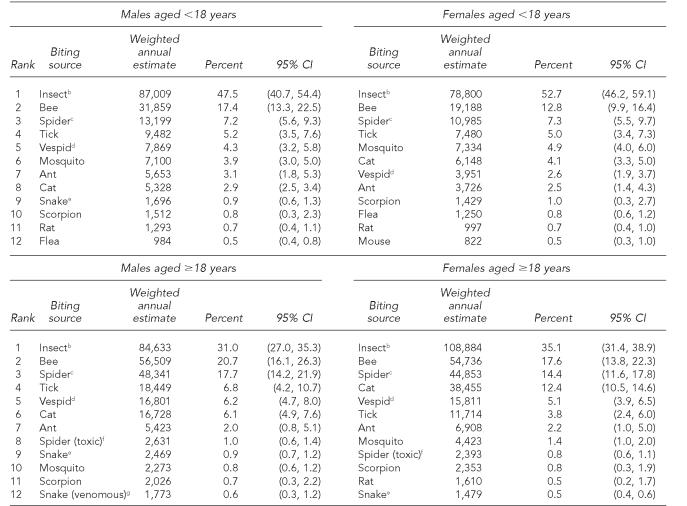
The 12 leading sources of bite or sting injury by gender and by age group are shown in Table 3. The top three reported bite or sting sources among male and female children (<18 years) and adults (≥18 years) were the same: insect, bee, and spider. Children were significantly more likely than adults to be treated for an insect sting (female children 52.7%; 95% CI 46.2, 59.1; female adults 35.1%; 95% CI 31.4, 38.9; male children 47.5%; 95% CI 40.7, 54.4; male adults 31%; 95% CI 27, 35.3). Female adults were more likely than male adults to be treated for cat bites (female adults 12.4%; 95% CI 10.5. 14.6; male adults 6.1%; 95% CI 4.9, 7.6).
Table 3.
Most frequent sources of nonfatal unintentional bite and sting injuries treated in emergency departments, by gender and age group, U.S., 2001–2004 (weighted n=3,664,671)a
Excludes canine, human, and work-related bite and sting injuries
Insect includes unspecified insects.
Spider does not include the toxic spider subcategory.
Vespid includes hornets, wasps, and yellow jackets.
Snake does not include the venomous snake subcategory.
Spider (toxic) includes black widow and brown recluse.
Snake (venomous) includes copperhead, rattlesnake, cottonmouth, water moccasin, and unspecified venomous.
CI = confidence interval
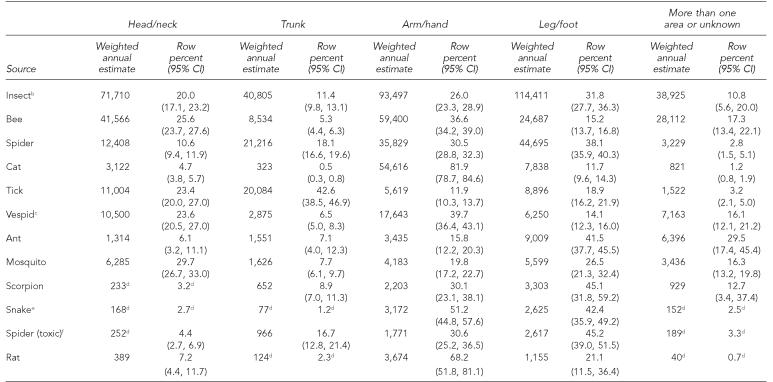
Table 4 shows the distribution of the 12 leading sources of bites and stings by body part affected. For bee stings, the arm and hand, and head and neck regions of the body were more frequently treated (arm or hand 36.6%; 95% CI 34.2, 39; head or neck 25.6%; 95% CI 23.7, 27.6) than the leg and foot (15.2%; 95% CI 13.7, 16.8) or trunk (5.3%; 95% CI 4.4, 6.3) regions. Tick bites mostly occurred on the trunk of the body (42.6%; 95% CI 38.5, 46.9), while cat and rat bites were most often on the arms and hands (cat 81.9%; 95% CI 78.7, 84.6; rat 68.2%; 95% CI 51.8, 81.1). Ant and scorpion bites predominately affected the legs and feet (ant 41.5%; 95% CI 37.7, 45.5; scorpion 45.1%; 95% CI 31.8, 59.2).
Table 4.
Affected body part for the most frequent sources of nonfatal unintentional bite and sting injuries treated in emergency departments, U.S., 2001–2004 (weighted n=3,664,671)a
Excludes canine, human, and work-related bite and sting injuries
Insect includes unspecified insects.
Vespid includes hornets, wasps, and yellow jackets.
Estimates might be unstable because the number of sample cases was <20.
Snake does not include copperhead, rattlesnake, cottonmouth, water moccasin, or unspecified venomous.
Spider (toxic) includes black widow and brown recluse.
CI = confidence interval
The demographic characteristics and disposition of patients reported to have anaphylactic signs or symptoms were also assessed. Annually, 25,360 patients were treated in U.S. EDs for anaphylactic signs or symptoms after a Hymenoptera bite or sting; most were treated and released (95.1%; 95% CI 93.3, 96.4); 3.4% (95% CI 2.3, 5.1) were hospitalized. Patients with anaphylactic signs and symptoms were more likely to be male than female (male 56.4%; 95% CI 53.6, 59.1; female 43.6%; 95% CI 40.9, 46.4). The mean age of patients with anaphylactic symptoms was 34.3 years (95% CI 32.2, 36.5). The predominant source of severe allergic reactions was a bee sting (49.6%; 95% CI 35.5, 63.8).
Limitations
The NEISS-AIP is designed to provide national estimates and does not include state or local estimates; therefore, regional differences in bite or sting injuries cannot be elucidated through this dataset. This limitation is particularly evident among certain species, such as venomous snakes, whose distribution and prevalence vary throughout the U.S.24–27 For example, a tertiary referral poison treatment center in central Arizona documented 236 rattlesnake bites in a seven-year period,28 and a national review of death certificates found that 97 deaths between 1978 and 1997 were due to snakebites, with Texas, Florida, and Georgia having the greatest incidence of deaths.29 Regional differences are mitigated somewhat, however, by travel and exotic pet ownership. Some of the narrative descriptions indicated that the injured person waited to seek care until returning home from travel or indicated that the encounter was with an exotic pet.
The spider bite literature is unique among that of other sources of bites and stings because of robust disputes regarding identification of spiders and the validity of spider bite reporting. People who present in the health-care setting with signs and symptoms of a spider bite wound may not have witnessed the bite event, may not have seen a spider in the area, or if they had seen the spider, may not have been able to identify the species.30 Poisonous spider bites may be diagnosed and reported in parts of the country where the species of spiders are not known to have a natural habitat;31 however, narratives in the case records indicate that individuals do occasionally seek care in a different place than the injury event.
Fatal injuries, injuries treated in health-care facilities outside of an ED (e.g., a physician's office or an urgent care center), or those injuries for which no professional medical care was received were not included. Therefore, our estimates may have undercounted the total burden of bite or sting injuries in the U.S. In addition, details of serious outcomes such as severe allergic reactions, wound infection, and zoonotic and vector-borne diseases (e.g., rabies, West Nile virus, and Lyme disease) were limited in this surveillance system.
Another limitation was that the level of detail in the narratives varied. Therefore, systematically reported data were not available on factors potentially associated with the injury incident, such as known insect allergy, a risk factor associated with an increased risk for an anaphylactic episode,32 or asthma—a condition that can influence the course of treatment. As previous work has pointed out, methicillin-resistant Staphylococcus aureus may be misdiagnosed and attributed to a spider bite,33 or they may coincide.34 We were unable to determine the misdiagnosed cases, and this bias may have led to an overcount of bite injuries.
Information on the circumstances of the event, such as intentionality of the interaction with the animal, was often limited. Furthermore, the description of the bite or sting source was sometimes vague (e.g., DX: insect bite). This was a limitation of medical record data. Another limitation for this study was that underlying conditions were not part of the standard data collection, although mentions of various conditions were occasionally found in narratives. While missing data were less than 0.1% for main variables such as diagnosis, age, gender, body part, or disposition, the data were not presented by race and ethnicity because of the high percentage of cases where race/ethnicity was not specified in the medical record.
Location of the bite or sting event was unknown in 50% of the cases, and thus this variable was also excluded in analyses. Of the cases where location was determined, 88% of the injuries occurred in or around the home.
DISCUSSION
Most previous reports of non-canine bite or sting injuries described a specific population, geographic region, or source animal or insect. This article describes the diversity of exposures resulting in non-canine bite or sting injuries treated in EDs at the national level. Results showed that over the course of four years, more than 3.6 million people were treated in U.S. EDs for injuries related to non-canine bites and stings. This equates to 1.7 bite or sting injuries treated in U.S. EDs per minute. This number does not include deaths from non-canine bites, which average 158 annually,35 or the multitude of bite and sting injuries that are treated outside the ED by other health-care providers.36 Non-canine bites and stings were the seventh-leading cause of nonfatal injuries seen in U.S. EDs in 2003.23 More than 92,000 non-canine bite or sting injuries were reported to the American Association of Poison Control Centers in 2003.37
While the majority of our cases involved unspecified insects as the source of the bite or sting, the 10 leading identified sources were bees, spiders, cats, ticks, vespids, ants, mosquitoes, scorpions, snakes, and harmful spiders. While some organisms, such as fire ants and scorpions, can be found only in certain regions of the U.S., others including yellow jackets, mosquitoes, and cats are more ubiquitous. According to the American Veterinary Medical Association, there were nearly 71 million pet cats, 10 million birds, 5 million rabbits, 1 million hamsters, and 700,000 snakes in U.S. households in 2001.38 As the practice of exotic pet trade activity increases, the possibility of public health practitioners treating an injury from these species may also increase. Bites or stings can occur in many settings, interactions with animals can be either intentional or unintentional, and interactions are influenced by curiosity, encroachment on habitats, seasonal activities, or intoxication.
In this study, the percentage of women treated in the ED for bites and stings was similar to men. For most other nonfatal injury mechanisms, such as nonfatal drowning and poisonings, men generally have a significantly higher injury rate than women.23 The leading sources of animal bites and stings were similar among the sexes, although the distribution was different. We did not find gender differences in reports of spider bites overall, or for black widow or brown recluse spider bites. Previous work with poison center data did find a difference between men and women with a higher proportion of reported black widow spider bites among men and more brown recluse spider bites among women.39
Results support previous research suggesting that risk is greatest in the summer months2,5 and that injuries mostly occur to extremities of the body.2,3,6,32 Children <18 years of age had a higher rate of ED visits for bites or stings than adults. Unspecified insect bites were a higher proportion among children than among adults, which may be due to the fact that parents may not have witnessed the bite or sting to their child, and children may be too young to properly identify the source.
The severity of the injury was ascertained through the disposition of the patient, specifically, whether discharged or hospitalized. Few patients were hospitalized (1.8%), compared with the average for all unintentional injuries during the 2001 through 2004 period of the study (5.4%). Although most were treated and released, bite and sting injuries can lead to serious outcomes. The percent hospitalized was substantially higher in some groups (e.g., 3.2% of the patients seen with anaphylactic symptoms were hospitalized; 58.4% of the known venomous snakebite patients were hospitalized).
Bites and stings from Hymenoptera, an order of insects that includes bees, vespids (wasps, yellow jackets, and hornets), and ants are of particular concern due to the risk of systemic allergic reaction (anaphylaxis). Anaphylactic signs and symptoms include cardiovascular reactions (e.g., hypotension and arrhythmias), respiratory reactions (e.g., bronchospasm), cutaneous reactions (e.g., hives), and gastrointestinal distress.40 In severe cases, anaphylaxis may lead to death. The percent of the U.S. population at risk for Hymenoptera sting anaphylaxis is up to 5%, or 13.6 million, and the number of deaths attributable to insect-related anaphylaxis is between 40 and 100 annually.41,42 In our study, the mean age of a patient bitten or stung by a Hymenoptera and exhibiting signs or symptoms of anaphylaxis was 34 years; 56% of these patients were male. This is similar to other reports.32 Because a history of anaphylaxis reaction is a predictor of future occurrence, guidelines recommend that patients with anaphylactic reactions to Hymenoptera be educated on techniques of self-administered epinephrine and be referred to an allergist.32
Our study found that more than 900,000 people sought treatment at an ED for non-canine mammal bites annually. A large proportion of those cases (66,000 annually) were people treated in EDs for cat bites. Dog bites were more common, with an estimated 368,245 people treated in EDs in 2001.23 Cat bites, however, were more likely than dog bites to result in an infected wound.3,43,44 Similar to dog bites, overall bite and sting injuries were more frequent in the summer months and rates were higher among children.
Mammalian bites are of particular concern for the public's health because they can lead to rabies exposure, rat-bite fever, and other zoonotic infectious diseases. Rabies surveillance of animal cases reported to the CDC during 2003 indicated that it was most commonly identified in wild animals, although 8.6% of the cases were from domesticated species. The U.S. animal species that carry rabies include raccoons, skunks, bats, foxes, cats, dogs, and cattle.45 Previous surveillance of animal bites found that the ownership of the biting animal was largely known.2,3,43,44 Pet owners, therefore, can be targeted for education regarding the potential for wound infections and zoonotic transmissions from both domesticated and wild animal bites. More information is available at: http://www.cdc.gov/healthypets. Distribution of hamsters and other pet rodents from centralized breeding facilities to pet stores located in various states46 and the distribution of imported, exotic pets47 have resulted in the diffusion of potential infectious exposures that may be infrequently seen by local physicians (e.g., monkeypox).
Some snake species including rattlesnakes, cottonmouths, copperheads, and coral snakes can poison their victims, though the effects are generally only severe to those with impaired health, such as the very young or old or people with chronic diseases.48 In severe cases, envenomations can cause coagulopathy, renal failure, shock, and even death.49 Our study indicated that more than half of venomous snakebite patients were hospitalized. This number was substantially higher than the overall frequency of hospitalized patients for our study population.
Animal-related morbidity and mortality events cited in the popular press have included alligator and shark bites and jellyfish stings, though these interactions occurred relatively infrequently compared with other sources of bites and stings. Burgess et al. report that during a 66-year period (1928 through 1993), there were 154 alligator bites in Florida, which amounts to two reported bites per year.50 The authors also reported that between 1990 and 1996, there were 106 unprovoked shark attacks in Florida, amounting to approximately 15 attacks per year or a crude rate of 1.1 per 1 million people per six years.50 In a more recent report, Langley investigated injuries and deaths due to alligator attacks and found that 15 deaths and 376 injuries occurred during a 57-year period (1948 through 2004) in the U.S.51 Our estimates also indicate that alligator and shark bites are rare events. Langley notes, however, that alligator nuisance complaints have been increasing and this may be due to the increasing alligator population and human encroachment into alligator habitats.51 There are case reports of jellyfish stings resulting in fatal envenomations in the Gulf Coast and Portuguese man-of-war fatalities in Florida and North Carolina.52 Our study found that an estimated 650 jellyfish stings were treated in U.S. EDs annually. Marine interactions with stingrays, jellyfish, barracudas, and moray eels generally result in lacerations and skin irritation injuries.53
CONCLUSION
This article summarizes the characteristics and volume of bite and sting injury cases treated in U.S. EDs. It highlights that treating bite and sting injuries consumes substantial health-care resources. Estimates of the lifetime costs for all ED treated bites and stings in 2000 topped $900 million; costs for cases that required hospitalization added another $179 million in lifetime costs.54 Preventing injuries can be accomplished by avoiding exposure to unfamiliar and wild animals, using repellents, and wearing appropriate clothing. Additional caution should be used when attempting to handle animals that are sick or injured, especially stray and wild animals that may expose people to zoonotic diseases such as rabies and catch-scratch disease.55
Previous examinations suggest that there is a lack of knowledge among the public regarding important guidelines for treating bite and sting injuries, such as proper wound care and the need to rapidly remove bee stingers.56 While preventing these injuries would be the first line of defense, considerable cost saving also might be achieved through public education on immediate first aid, and what warning signs and symptoms indicate a need for professional emergency care. The appropriate use of first aid may reduce the rates of secondary infection, allergic reaction, and transmission of zoonotic and vector-borne diseases. By improving the delivery of first aid at home in less serious cases, we would anticipate an overall reduction of the burden of ED treatment.
Footnotes
The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the Centers for Disease Control and Prevention.
REFERENCES
- 1.Glaser C, Lewis P, Wong S. Pet-, animal-, and vector-borne infections. Pediatr Rev. 2000;21:219–32. doi: 10.1542/pir.21-7-219. [DOI] [PubMed] [Google Scholar]
- 2.Hanna TL, Selby LA. Characteristics of the human and pet populations in animal bite incidents recorded at two Air Force bases. Public Health Rep. 1981;96:580–4. [PMC free article] [PubMed] [Google Scholar]
- 3.Kizer KW. Epidemiologic and clinical aspects of animal bite injuries. JACEP. 1979;8:134–41. doi: 10.1016/s0361-1124(79)80339-1. [DOI] [PubMed] [Google Scholar]
- 4.Langley RL. Fatal animal attacks in North Carolina over an 18-year period. Am J Forensic Med Pathol. 1994;15:160–7. doi: 10.1097/00000433-199406000-00014. [DOI] [PubMed] [Google Scholar]
- 5.Sinclair CL, Zhou C. Descriptive epidemiology of animal bites in Indiana, 1990–92—a rationale for intervention. Public Health Rep. 1995;110:64–7. [PMC free article] [PubMed] [Google Scholar]
- 6.Spence G. A review of animal bites in Delaware—1989 to 1990. Del Med J. 1990;62:1425–33. [PubMed] [Google Scholar]
- 7.Elston DM. Systemic manifestations and treatment of brown recluse spider bites. Cutis. 2004;74 336,38,40. [PubMed] [Google Scholar]
- 8.Hughes A. Observation of snakebite victims: is twelve hours still necessary? Emerg Med (Fremantle) 2003;15:511–7. doi: 10.1046/j.1442-2026.2003.00510.x. [DOI] [PubMed] [Google Scholar]
- 9.Stefanopoulos P, Karabouta Z, Bisbinas I, Georgiannos D, Karabouta I. Animal and human bites: evaluation and management. Acta Orthop Belg. 2004;70:1–10. [PubMed] [Google Scholar]
- 10.Applegate JA, Walhout MF. Childhood risks from the ferret. J Emerg Med. 1998;16:425–7. doi: 10.1016/s0736-4679(98)00008-0. [DOI] [PubMed] [Google Scholar]
- 11.Fatal rat-bite fever—Florida and Washington, 2003. MMWR Morb Mortal Wkly Rep. 2005;53(51):1198–202. [PubMed] [Google Scholar]
- 12.Riordan C, Hussain M, McCann J. Moray eel attack in the tropics: a case report and review of the literature. Wilderness Environ Med. 2004;15:194–7. doi: 10.1580/1080-6032(2004)15[194:meaitt]2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 13.Quinlan KP, Thompson MP, Annest JL, Peddicord J, Ryan G, Kessler EP, et al. Expanding the National Electronic Injury Surveillance System to monitor all nonfatal injuries treated in US hospital emergency departments. Ann Emerg Med. 1999;34:637–45. doi: 10.1016/s0196-0644(99)70166-6. [DOI] [PubMed] [Google Scholar]
- 14.Vyrostek SB, Annest JL, Ryan GW. Surveillance for fatal and nonfatal injuries—United States, 2001. MMWR Surveill Summ. 2004;53(7):1–57. [PubMed] [Google Scholar]
- 15.Claassen CA, Trivedi MH, Shimizu I, Stewart S, Larkin GL, Litovitz T. Epidemiology of nonfatal deliberate self-harm in the United States as described in three medical databases. Suicide Life Threat Behav. 2006;36:192–212. doi: 10.1521/suli.2006.36.2.192. [DOI] [PubMed] [Google Scholar]
- 16.Nonfatal self-inflicted injuries treated in hospital emergency departments—United States, 2000. MMWR Morb Mortal Wkly Rep. 2002;51(20):436–8. [PubMed] [Google Scholar]
- 17.Adams AL, Schiff MA. Childhood soccer injuries treated in U.S. emergency departments. Acad Emerg Med. 2006;13:571–4. doi: 10.1197/j.aem.2005.12.015. [DOI] [PubMed] [Google Scholar]
- 18.Linakis JG, Amanullah S, Mello MJ. Emergency department visits for injury in school-aged children in the United States: a comparison of nonfatal injuries occurring within and outside of the school environment. Acad Emerg Med. 2006;13:567–70. doi: 10.1197/j.aem.2005.11.073. [DOI] [PubMed] [Google Scholar]
- 19.Qazi K, Gerson LW, Christopher NC, Kessler E, Ida N. Curling iron-related injuries presenting to U.S. emergency departments. Acad Emerg Med. 2001;8:395–7. doi: 10.1111/j.1553-2712.2001.tb02121.x. [DOI] [PubMed] [Google Scholar]
- 20.Skarbek-Borowska S, Amanullah S, Mello MJ, Linakis JG. Emergency department visits for sledding injuries in children in the United States in 2001/2002. Acad Emerg Med. 2006;13:181–5. doi: 10.1197/j.aem.2005.09.009. [DOI] [PubMed] [Google Scholar]
- 21.Nonfatal dog bite-related injuries treated in hospital emergency departments—United States, 2001. MMWR Morb Mortal Wkly Rep. 2003;52(26):605–10. [PubMed] [Google Scholar]
- 22.Schroeder T, Ault K, Commission UCPS, editors. NEISS All Injury Program: sample design and implementation. Washington: U.S. Consumer Product Safety Commission; 2001. [Google Scholar]
- 23.Centers for Disease Control and Prevention (US); National Center for Injury Prevention and Control, Centers for Disease Control and Prevention (producer) Web-based Injury Statistics Query and Reporting System (WISQARS) [online] [cited 2005 Oct 15]. Available from: URL: www.cdc.gov/ncipc/wisqars wisqars.
- 24.Downey DJ, Omer GE, Moneim MS. New Mexico rattlesnake bites: demographic review and guidelines for treatment. J Trauma. 1991;31:1380–6. [PubMed] [Google Scholar]
- 25.Farstad D, Thomas T, Chow T, Bush S, Stiegler P. Mojave rattlesnake envenomation in southern California: a review of suspected cases. Wilderness Environ Med. 1997;8:89–93. doi: 10.1580/1080-6032(1997)008[0089:MREISC]2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 26.Morandi N, Williams J. Snakebite injuries: contributing factors and intentionality of exposure. Wilderness Environ Med. 1997;8:152–5. doi: 10.1580/1080-6032(1997)008[0152:sicfai]2.3.co;2. [DOI] [PubMed] [Google Scholar]
- 27.Plowman DM, Reynolds TL, Joyce SM. Poisonous snakebite in Utah. West J Med. 1995;163:547–51. [PMC free article] [PubMed] [Google Scholar]
- 28.Tanen D, Ruha A, Graeme K, Curry S. Epidemiology and hospital course of rattlesnake envenomations cared for at a tertiary referral center in Central Arizona. Acad Emerg Med. 2001;8:177–82. doi: 10.1111/j.1553-2712.2001.tb01284.x. [DOI] [PubMed] [Google Scholar]
- 29.Morgan BW, Lee C, Damiano L, Whitlow K, Geller R. Reptile envenomation: 20-year mortality as reported by US medical examiners. South Med J. 2004;97:642–4. doi: 10.1097/00007611-200407000-00006. [DOI] [PubMed] [Google Scholar]
- 30.Isbister GK, White J. Clinical consequences of spider bites: recent advances in our understanding. Toxicon. 2004;43:477–92. doi: 10.1016/j.toxicon.2004.02.002. [DOI] [PubMed] [Google Scholar]
- 31.Wendell RP. Brown recluse spiders: a review to help guide physicians in nonendemic areas. South Med J. 2003;96:486–90. doi: 10.1097/01.SMJ.0000066761.59212.22. [DOI] [PubMed] [Google Scholar]
- 32.Clark S, Long AA, Gaeta TJ, Camargo CA. Multicenter study of emergency department visits for insect sting allergies. J Allergy Clin Immunol. 2005;116:643–9. doi: 10.1016/j.jaci.2005.06.026. [DOI] [PubMed] [Google Scholar]
- 33.Dominguez TJ. It's not a spider bite, it's community-acquired methicillin-resistant Staphylococcus aureus. J Am Board Fam Pract. 2004;17:220–6. doi: 10.3122/jabfm.17.3.220. [DOI] [PubMed] [Google Scholar]
- 34.Fagan SP, Berger DH, Rahwan K, Awad SS. Spider bites presenting with methicillin-resistant staphylococcus aureus soft tissue infection require early aggressive treatment. Surg Infect (Larchmt) 2003;4:311–5. doi: 10.1089/109629603322761364. [DOI] [PubMed] [Google Scholar]
- 35.Langley RL. Animal-related fatalities in the United States—an update. Wilderness Environ Med. 2005;16:67–74. doi: 10.1580/1080-6032(2005)16[67:afitus]2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 36.Schappert SM, Burt CW. Ambulatory care visits to physician offices, hospital outpatient departments, and emergency departments: United States, 2001–02. Vital Health Stat. 2006;13(159) [PubMed] [Google Scholar]
- 37.Watson WA, Litovitz TL, Klein-Schwartz W, Rodgers GC, Jr, Youniss J, Reid N, et al. 2003 annual report of the American Association of Poison Control Centers Toxic Exposure Surveillance System. Am J Emerg Med. 2004;22:335–404. doi: 10.1016/j.ajem.2004.06.001. [DOI] [PubMed] [Google Scholar]
- 38.American Veterinary Medical Association. U.S. Pet Ownership & Demographic Sourcebook. Schaumburg (IL): American Veterinary Medical Association; 2002. [Google Scholar]
- 39.Forrester MB, Stanley SK. Black widow spider and brown recluse spider bites in Texas from 1998 through 2002. Vet Hum Toxicol. 2003;45:270–3. [PubMed] [Google Scholar]
- 40.Valentine MD. Anaphylaxis and stinging insect hypersensitivity. JAMA. 1992;268:2830–3. [PubMed] [Google Scholar]
- 41.Matasar MJ, Neugut AI. Epidemiology of anaphylaxis in the United States. Curr Allergy Asthma Rep. 2003;3:30–5. doi: 10.1007/s11882-003-0007-8. [DOI] [PubMed] [Google Scholar]
- 42.Neugut AI, Ghatak AT, Miller RL. Anaphylaxis in the United States: an investigation into its epidemiology. Arch Intern Med. 2001;161:15–21. doi: 10.1001/archinte.161.1.15. [DOI] [PubMed] [Google Scholar]
- 43.Aghababian RV, Conte JE. Mammalian bite wounds. Ann Emerg Med. 1980;9:79–83. doi: 10.1016/s0196-0644(80)80335-0. [DOI] [PubMed] [Google Scholar]
- 44.Moore DA, Sischo WM, Hunter A, Miles T. Animal bite epidemiology and surveillance for rabies postexposure prophylaxis. J Am Vet Med Assoc. 2000;217:190–4. doi: 10.2460/javma.2000.217.190. [DOI] [PubMed] [Google Scholar]
- 45.Krebs JW, Mandel EJ, Swerdlow DL, Rupprecht CE. Rabies surveillance in the United States during 2003. J Am Vet Med Assoc. 2004;225:1837–49. doi: 10.2460/javma.2004.225.1837. [DOI] [PubMed] [Google Scholar]
- 46.Outbreak of multidrug-resistant Salmonella typhimurium associated with rodents purchased at retail pet stores—United States, December 2003-October 2004. MMWR Morb Mortal Wkly Rep. 2005;54(17):429–33. [PubMed] [Google Scholar]
- 47.Update: Multistate outbreak of monkeypox—Illinois, Indiana, Kansas, Missouri, Ohio, and Wisconsin, 2003. MMWR Morb Mortal Wkly Rep. 2003;52(27):642–6. [PubMed] [Google Scholar]
- 48.Otten EJ, Blomkalns A. Rosen's Emergency Medicine. 5th ed. Vol 1. St. Louis: Mosby; 2002. Venomous animal injuries. [Google Scholar]
- 49.Juckett G, Hancox JG. Venomous snakebites in the United States: management review and update. Am Fam Physician. 2002;65:1367–78. [PubMed] [Google Scholar]
- 50.Burgess GH, Callahan MT, Howard RJ. Sharks, alligators, barracudas, and other biting animals in Florida waters. J Fla Med Assoc. 1997;84:428–32. [PubMed] [Google Scholar]
- 51.Langley RL. Alligator attacks on humans in the United States. Wilderness Environ Med. 2005;16:119–24. doi: 10.1580/1080-6032(2005)16[119:AAOHIT]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 52.Fenner PJ, Williamson JA. Worldwide deaths and severe envenomation from jellyfish stings. Med J Aust. 1996;165:658–61. doi: 10.5694/j.1326-5377.1996.tb138679.x. [DOI] [PubMed] [Google Scholar]
- 53.Auerbach PS. Hazardous marine animals. Emerg Med Clin North Am. 1984;2:531–44. [PubMed] [Google Scholar]
- 54.Finkelstein EA, Corso PS, Miller TR. The incidence and economic burden of injuries in the United States. New York: Oxford University Press; 2006. [Google Scholar]
- 55.Freer L. North American wild mammalian injuries. Emerg Med Clin North Am. 2004;22:445–73. ix. doi: 10.1016/j.emc.2004.01.008. [DOI] [PubMed] [Google Scholar]
- 56.Singer AJ, Gulla J, Thode HC, Jr, Cronin KA. Pediatric first aid knowledge among parents. Pediatr Emerg Care. 2004;20:808–11. doi: 10.1097/01.pec.0000148028.53598.5c. [DOI] [PubMed] [Google Scholar]