Interferon induced HBeAg loss is persistent in up to 90% of patients with chronic hepatitis B (HBV).1,2,3 Older age and vertical transmission have been shown previously to be independent predictors of relapse after conventional IFN.4 Shorter duration of HBV DNA below 0.7 log10 IU/ml was found to predict relapse after lamivudine.5 Predictors of relapse after PEG‐IFN treatment are, however, still unknown. Our aim in this study was to investigate the frequency and predictors of relapse after treatment with PEG‐IFN α‐2b alone or in combination with lamivudine.
Data for this study were extracted from a multicentre randomised controlled trial comparing 52 weeks of PEG‐IFN α‐2b monotherapy (100 μg/week) with combined PEG‐IFN and lamivudine (100 mg/day) in 266 patients with HBeAg positive chronic hepatitis B. The inclusion and exclusion criteria for the study were reported previously.6 Relapse was defined as HBeAg negativity at the end of treatment (week 52) and recurrence of HBeAg at the end of follow up (week 78).
Treatment groups were comparable regarding baseline characteristics. At the end of treatment, 57 of 130 patients (44%) in the combination therapy group and 40 of 136 (29%) in the monotherapy group lost HBeAg (p = 0.01). HBeAg relapse occurred more often in patients treated with PEG‐IFN α‐2b and lamivudine combination therapy compared with PEG‐IFN α‐2b alone (22 of 57 patients (39%) vs five of 40 (13%), p = 0.005). Patients with HBeAg relapse were more likely to have relapse of HBV DNA >200 000 copies/ml than sustained HBeAg responders (76% vs 20%, p<0.001), as well as relapse of alanine aminotransferase (69% vs 24%, p = 0.007).
Among patients treated with combination therapy, seven of 33 (21%) with detectable anti‐HBe at week 52 relapsed compared with 15 of 24 (63%) without detectable anti‐HBe (p = 0.002). A similar trend was observed in patients treated with PEG‐IFN α‐2b alone: two of 30 patients (7%) with detectable anti‐HBe and three of seven without (30%) relapsed (p = 0.09). The HBV genotype tended to influence HBeAg relapse rates: 29% of patients harbouring genotype A relapsed compared with 56% of those with genotype D (p = 0.09). Three of four patients (75%) with lamivudine resistance showed HBeAg relapse compared with 19 of 53 (36%) without antiviral resistance (p = 0.29).
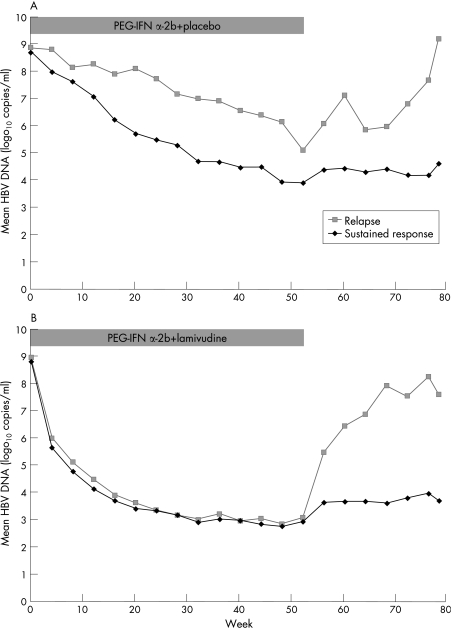
Mean HBV DNA levels in patients with HBeAg relapse and in sustained responders are shown in fig 1 for both treatment groups. In patients treated with PEG‐IFN α‐2b alone, the combination of HBeAg loss and HBV DNA <10 000 copies/ml at week 52 was associated with a significantly lower rate of relapse compared with partial response of HBeAg loss but HBV DNA ⩾10 000 copies/ml (p = 0.01). At the end of follow up, 56% of patients with sustained HBeAg response had HBV DNA <10 000 copies/ml compared with 4% of patients with relapse (p<0.001). Factors independently associated with HBeAg relapse in time dependent multivariate logistic regression analysis are shown in table 1.
Figure 1 Mean hepatitis B virus (HBV) DNA in patients with HBeAg relapse and sustained response after PEG‐IFN α‐2b alone or in combination with lamivudine. Among patients treated with PEG‐IFN α‐2b monotherapy, the decline in HBV DNA was more pronounced in sustained responders than in relapsers (A). This difference was, however, not observed in patients treated with PEG‐IFN α‐2b and lamivudine combination therapy (B). Mean HBV DNA was comparable in sustained responders and relapsers at baseline in both treatment groups. In patients treated with PEG‐IFN α‐2b alone, decline in HBV DNA was 4.8 log10 copies/ml for sustained responders compared with 3.8 log10 copies/ml for patients with relapse at the end of treatment (p = 0.30). The decline in HBV DNA was 5.8 log10 copies/ml for all patients in the combination therapy group at the end of treatment. In both treatment groups mean HBV DNA was significantly higher in relapsers than in sustained responders at week 78 (9.2 log10 vs 4.6 log10 for monotherapy, and 7.7 log10vs 3.7 log10 for combination therapy, p<0.001).
Table 1 Factors significantly associated with HBeAg relapse in multivariate analysis.
| Variable | OR (95% CI, lower–upper) | p Value |
|---|---|---|
| Combination therapy | 3.9 (1.1 to 13.2) | 0.03 |
| HBsAg positivity at week 52 | 10.3 (1.09 to 97.89) | 0.04 |
| Absence of anti‐HBe at week 52 | 9.8 (3.2 to 30.3) | <0.001 |
CI, confidence interval; OR, odds ratio.
In HBeAg positive chronic hepatitis B, it is assumed that relapse occurs frequently after discontinuation of nucleoside or nucleotide analogue therapy, while response appears more durable after interferon based treatment because of its immunomodulatory effects. The observed relapse rates in our study are consistent with findings of previous studies, which showed HBeAg relapse in 22–40% of lamivudine treated patients,3,7 in 10% of IFN treated patients,1,3 and in 18–22% of patients treated with PEG‐IFN α‐2a.8 The higher relapse rates after cessation of combination therapy compared with PEG‐IFN α‐2b monotherapy in our study can most probably be explained by lamivudine induced HBeAg loss.
Treatment with PEG‐IFN and lamivudine combination therapy, absence of anti‐HBe, and HBsAg positivity at week 52 were independently associated with HBeAg recurrence. In addition to these predictors, a profound decline in HBV DNA (below 10 000 copies/ml) also seems important for maintaining PEG‐IFN induced response and may be associated with immune control of the virus. Patients with a partial response, as defined by HBeAg loss but insufficient decline of HBV DNA (not below 10 000 copies/ml) at the end of therapy, might benefit from prolonged treatment, as this has previously been shown to increase response to standard IFN.9
In conclusion, HBeAg relapse occurs more commonly after PEG‐IFN α‐2b and lamivudine combination therapy than after PEG‐IFN α‐2b monotherapy. Absence of anti‐HBe at the end of treatment was found to be the strongest predictor of relapse. Full HBeAg seroconversion with the appearance of anti‐HBe, rather than HBeAg loss, thus seems the best end point of PEG‐IFN based treatment in HBeAg positive chronic HBV.
Acknowledgements
Other members of the HBV 99‐01 Study Group: Netherlands – KJ van Erpecum, BCM Vroom (University Medical Centre, Utrecht); CMJ van Nieuwkerk (VU University Medical Centre, Amsterdam); J Jansen, J Drenth, SJ van den Hazel (University Medical Centre Radboud, Nijmegen); JW den Ouden‐Muller (St Franciscus Hospital, Rotterdam); AC Tan (Canisius Wilhelmina Hospital, Nijmegen). Belgium – DM Adler (Hopital Erasme, Brussels); P Michielsen (University Hospital, Antwerp); H van Vlierberghe (University Hospital, Gent); J Delwaide (Centre Hospitalier Universitaire, Liège); J Henrion (Hopital de Jolimont, Hainet Paul). Germany – S Bein, U Treichel (University Hospital, Essen); MP Manns, J Hadem (Medizinische Hochschule, Hannover); C Niederau (St Jozef Hospital, Oberhausen). Denmark – MR Buhl, IM Hansen (Skejby Hospital, Arhus); K Krogsgaard (Copenhagen University Hospital, Hvidovre). Poland – J Jablonska, J Kozlowska (Medical Academy of Warsaw, Warsaw); D Prokopowicz, R Flisiak (Medical Academy of Bialystok, Bialystok). Spain – M Buti, A Valdes, R Esteban (Hospital Valle Hebron, Barcelona); M Rodriguez, M Garcia Espiga (Hospital Central de Asturias, Oviedo). Italy – A Andriulli, G Stornaiulo, GB Gaeta (Ospedale Gesù e Maria, Napoli); G Montalto, F D'Antona (Università di Palermo, Palermo). Greece – P Xiarchos Panagiotis (George Papanikolaou General Regional Hospital,Thessaloniki); NC Tassopoulos (West Attica Hospital, Athens). Turkey – G Ersöz (Ege University Faculty of Medicine, Izmir); C Yurdayin, H Bozkaya (Medical School Cebeci Kampusu, Ankara); Y Balaban (Hacettepe University Faculty of Medicine, Ankara), F Tabak (Istanbul University Cerrahpasa Medical School, Istanbul). Israel – Y Lurie (Sauraski Medical Center, Tel‐Aviv). Canada – S Greenbloom (General Hospital, Etobicoke). Indonesia – DA Sulaiman (Ciptomangunkusomo Hospital, Jakarta). Singapore – R Guan (Mount Elizabeth Medical Center Singapore).
The study was organised and sponsored by the foundation for liver research (SLO), Rotterdam, Netherlands. Financial support and study medication was provided by Schering‐Plough International, Kenilworth, NJ, USA and GlaxoSmithKline, Research and Development, Greenford, UK.
Footnotes
Conflict of interest: None declared.
References
- 1.van Zonneveld M, Honkoop P, Hansen B E.et al Long‐term follow‐up of alpha‐interferon treatment of patients with chronic hepatitis B. Hepatology 200439804–810. [DOI] [PubMed] [Google Scholar]
- 2.Korenman J, Baker B, Waggoner J.et al Long‐term remission of chronic hepatitis B after alpha‐interferon therapy. Ann Intern Med 1991114629–634. [DOI] [PubMed] [Google Scholar]
- 3.van Nunen A B, Hansen B E, Suh D J.et al Durability of HBeAg seroconversion following antiviral therapy for chronic hepatitis B: relation to type of therapy and pretreatment serum hepatitis B virus DNA and alanine aminotransferase. Gut 200352420–424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Song B C, Suh D J, Lee H C.et al Which patients with chronic hepatitis B are more likely to relapse after interferon alpha‐induced hepatitis B e antigen loss in Korea? J Clin Gastroenterol 200438124–129. [DOI] [PubMed] [Google Scholar]
- 5.Ito K, Tanaka Y, Orito E.et al Predicting relapse after cessation of lamivudine monotherapy for chronic hepatitis B virus infection. Clin Infect Dis 200438490–495. [DOI] [PubMed] [Google Scholar]
- 6.Janssen H L, van Zonneveld M, Senturk H.et al Pegylated interferon alfa‐2b alone or in combination with lamivudine for HBeAg‐positive chronic hepatitis B: a randomised trial. Lancet 2005365123–129. [DOI] [PubMed] [Google Scholar]
- 7.Yoon S K, Jang J W, Kim C W.et al Long‐term results of lamivudine monotherapy in Korean patients with HBeAg‐positive chronic hepatitis B: response and relapse rates, and factors related to durability of HBeAg seroconversion. Intervirology 200548341–349. [DOI] [PubMed] [Google Scholar]
- 8.Lau G K, Piratvisuth T, Luo K X.et al Peginterferon Alfa‐2a, lamivudine, and the combination for HBeAg‐positive chronic hepatitis B. N Engl J Med 20053522682–2695. [DOI] [PubMed] [Google Scholar]
- 9.Janssen H L, Berk L, Schalm S W.et al Antiviral effect of prolonged intermittent lymphoblastoid alpha interferon treatment in chronic hepatitis B. Gut 1992331094–1098. [DOI] [PMC free article] [PubMed] [Google Scholar]