Autoimmune pancreatitis is characterised by raised serum levels of IgG4 and IgG4‐bearing plasma cells in the inflammatory tissue.1 Similar pathology can also occur in the larger bile ducts, resembling sclerosing cholangitis.2 We report a patient with hepatitis and chronic cholecystitis, raised IgG4 level, and IgG4‐bearing plasma cells in the liver and gall bladder wall, but no evident pancreatic disease.
In January 2003, a cholecystectomy was undertaken on a 54 year old woman for chronic cholecystitis. The extracted gall bladder showed lymphoplasmacytic infiltration and subserosal fibrosis. A liver biopsy was done because of abnormal liver function tests and showed severe lobular hepatitis with mild portal inflammation. Plasma cell infiltration was observed in the portal tracts and parenchyma, though fibrosis was not significant. IgG4 bearing plasma cell infiltration was found both in the liver and the gall bladder wall. After six months, liver function was still abnormal: aspartate aminotransferase, 234 IU/l (reference range, 12 to 37); alanine aminotransferase, 487 IU/l (7 to 45); alkaline phosphatase, 478 IU/l (124 to 367); γ‐glutamyl transpeptidase, 581 IU/l (6 to 30); total bilirubin, 46.2 μmol/l (5 to 20); IgG, 2403 mg/dl (870 to 1700). The antinuclear antibody titre (1:80 on rodent tissue) was abnormal, and tests for autoantibodies to smooth muscle, double stranded DNA, and mitochondria were negative. Infection with hepatitis viruses A, B, and C, cytomegalovirus, and Epstein‐Barr virus was excluded. HLA DRB1 alleles were *1302 and *1501.
She denied taking medicines or herbal remedies.
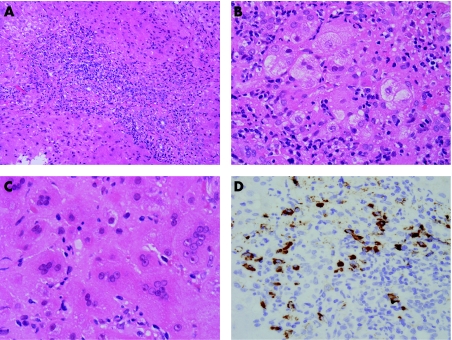
Ultrasonography, abdominal computed tomography, endoscopic retrograde cholangiography, and magnetic resonance cholangiopancreatography showed no abnormalities in the extrahepatic bile ducts or pancreas. A second liver biopsy, which was done six months after the first, showed changes associated with autoimmune hepatitis, interface hepatitis, lobular hepatitis, rosette formation, syncytial multinucleated giant cell change, and marked plasma cell infiltration (fig 1, panels A to C). Biliary features, such as cholangitis and periductal fibrosis, were not evident. Immunostaining of liver tissue showed abundance of plasma cells with strong immunohistochemical reactivity to IgG4 (fig 1D). The International Autoimmune Hepatitis Group (IAIHG) disease score was 18, identifying definite autoimmune hepatitis3 (table 1). Treatment was successful with prednisolone 40 mg daily for four weeks, tapered by 5 mg weekly to 5 mg daily. Serum IgG4 concentrations were 557 mg/dl pretreatment (reference range <135 mg/dl), 226 mg/dl after one month, and 44 mg/dl after one year. Serum aspartate aminotransferase and alanine aminotransferase were 94 and 278 IU/l after one month, 31 and 73 IU/l after two months, and 22 and 25 IU/l after one year, respectively.
Figure 1 Pathological findings of the second liver biopsy. (A) Portal tracts are enlarged with severe inflammatory cell infiltration. Interface hepatitis is also observed (H&E, ×200). (B) Hepatocytes show rosette formation (H&E, ×400). (C) Syncytial multinucleated giant cell change of hepatocytes is observed (H&E, ×400). (D) Immunostaining for IgG4 reveals abundant IgG4 bearing plasma cells in a portal tract (IgG4 immunostaining, ×400).
Table 1 Autoimmune hepatitis score using IAIHG scoring system.
| Variable/feature | Score |
|---|---|
| Female sex: female | +2 |
| ALP:AST ratio: 0.2 (<1.5) | +2 |
| Serum IgG above normal: 1.4 g/dl (1.0 to 1.5) | +1 |
| ANA: 1:80 | +2 |
| AMA positive: negative | 0 |
| Hepatitis viral markers: negative | +3 |
| Drug history: negative | +1 |
| Average alcohol intake: <25 g/day | +2 |
| Liver histology: | |
| Interface hepatitis | +3 |
| Predominantly lymphoplasmacytic infiltrate | +1 |
| Rosetting of liver cells | +1 |
| Total | +18 |
ALP, alkaline phosphatase; AMA, anti‐mitochondrial antibodies; ANA, antinuclear antibody; AST, aspartate aminotransferase; IAIHG, International Autoimmune Hepatitis Group.
Raised serum IgG4 concentration and IgG4‐bearing plasma cell infiltrates have a high sensitivity and specificity for the diagnosis of autoimmune pancreatitis1 and associated diseases, including sclerosing cholangitis.2 In the present case, the clinical and histological criteria for definite autoimmune hepatitis were met and, additionally, both biopsies showed hepatitis with abundant IgG4‐bearing plasma cells in the liver and gallbladder.
We previously studied 17 patients with classic autoimmune hepatitis. Both serum IgG4 and IgG4‐bearing plasma cells were completely absent in the liver of 13, and a minor increase in only one index was seen in four.4 Thus we can identify a new disease entity—IgG4 associated autoimmune hepatitis—which can be differentiated from other recognised types. Our present case implies that IgG4 related inflammatory processes can occur in the hepatic parenchyma in the same way as in the pancreatobiliary system, and such cases may resemble autoimmune hepatitis both clinically and pathologically. As such, detection of IgG4 and assessment of liver histology using IgG4 immunostaining may be useful for differentiating IgG4 related diseases from definite autoimmune hepatitis. Further studies are needed on this possible new disease entity and its impact on the diagnostic guidelines for autoimmune hepatitis.
Acknowledgements
This work was supported in part by a research on Measures for Intractable Diseases of the Pancreas, Health and Labour Sciences Research Grants, Japanese Ministry of Health, Labour and Welfare. We are indebted to Taeko Yamamoto for her technical assistance and to Dr Eishi Hara of Iida Hospital, Japan, for his clinical assistance.
Footnotes
Conflict of interest: None declared
References
- 1.Hamano H, Kawa S, Horiuchi A.et al High serum IgG4 concentrations in patients with sclerosing pancreatitis. N Engl J Med 2001344732–738. [DOI] [PubMed] [Google Scholar]
- 2.Zen Y, Harada K, Sasaki M.et al IgG4‐related sclerosing cholangitis with and without hepatic inflammatory pseudotumor, and sclerosing pancreatitis‐associated sclerosing cholangitis: do they belong to a spectrum of sclerosing pancreatitis? Am J Surg Pathol 2004281193–1203. [DOI] [PubMed] [Google Scholar]
- 3.Alvarez F, Berg P A, Bianchi F B.et al International Autoimmune Hepatitis Group report: review of criteria for diagnosis of autoimmune hepatitis. J Hepatol 199931929–938. [DOI] [PubMed] [Google Scholar]
- 4.Umemura T, Zen Y, Hamano H.et al IgG4‐hepatopathy: association of IgG4‐bearing plasma cells in liver with autoimmune pancreatitis. Hepatology. (in press). [DOI] [PubMed]