Abstract
PURPOSE We undertook a study to compare 3 ways of administering brief domestic violence screening questionnaires: self-administered questionnaire, medical staff interview, and physician interview.
METHODS We conducted a randomized trial of 3 screening protocols for domestic violence in 4 urban family medicine practices with mostly minority patients. We randomly assigned 523 female patients, aged 18 years or older and currently involved with a partner, to 1 of 3 screening protocols. Each included 2 brief screening tools: HITS and WAST-Short. Outcome measures were domestic violence disclosure, patient and clinician comfort with the screening, and time spent screening.
RESULTS Overall prevalence of domestic violence was 14%. Most patients (93.4%) and clinicians (84.5%) were comfortable with the screening questions and method of administering them. Average time spent screening was 4.4 minutes. Disclosure rates, patient and clinician comfort with screening, and time spent screening were similar among the 3 protocols. In addition, WAST-Short was validated in this sample of minority women by comparison with HITS and with the 8-item WAST.
CONCLUSIONS Domestic violence is common, and we found that most patients and clinicians are comfortable with domestic violence screening in urban family medicine settings. Patient self-administered domestic violence screening is as effective as clinician interview in terms of disclosure, comfort, and time spent screening.
Keywords: Domestic violence/diagnosis, screening
INTRODUCTION
The prevalence of current victims of domestic violence among patients in primary care settings ranges from 7% to 50%,1 even though studies show that only 1% to 15% of women in primary care settings were asked about domestic violence by their clinician.2–4 Lack of office protocols and limited time are perceived as common barriers by medical clinicians.5–8 In one study, battered women perceived clinician reluctance to ask about abuse as a major barrier to their domestic violence disclosure.9
Although studies have found that brief screening questionnaires increase identification of domestic violence,10,11 research findings are inconsistent on the optimum method of administering screening tests. In a recent randomized study, MacMillan et al found no significant difference in the proportion of patients who disclosed domestic violence using a self-administered questionnaire compared with patients who were interviewed by a clinician; the patients, however, preferred self-administered screening.12 McFarlane and colleagues found that a medical staff interview identified more abused women than a written history form,13 whereas another study reported opposite findings.14 With few notable exceptions,10,12–17 previous studies have not examined clinician and patient comfort with different screening protocols. One study of a brief screening tool indicated that 91% of women felt comfortable when screened by their clinicians.10
The purpose of this study was to identify an optimal screening protocol to help overcome barriers to domestic violence screening. We compared the rate of domestic violence disclosure, comfort level with screening, and time spent screening for self-administered, medical staff interview, and physician interview screening protocols.
METHODS
Participants
This randomized trial of 3 domestic violence screening protocols was conducted in 4 urban family medicine practices. The 4 practices have a total of 18 physicians and 27 residents who see approximately 3,500 patients per month total, of which 86% are African-American or Hispanic. The target population was women aged 18 years or older who were currently with a partner.
Procedure
Figure 1 ▶ is a flowchart of the study design. At the start of the study, 7 research assistants, all medical staff, and all physicians received 3 hours of training by the investigators in lecture format on screening techniques, the use of the screening questionnaires, assessment of domestic violence victims, interventions, and referral to support agencies.
Figure 1.
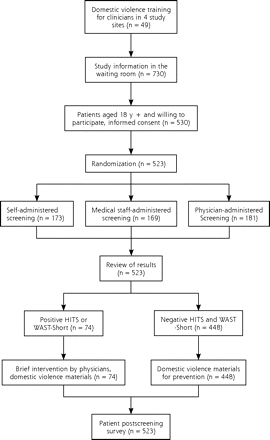
Flowchart of study design.
During June 2004 through March 2005, the research assistants approached and recruited consecutive patients and confirmed their eligibility in private. Screening at each practice site ranged from 2 to 5 months, because some practice sites see more adult female patients and took fewer months to accrue the sample. The research assistants completed the study in one practice before moving on to the next. Randomization of the 3 protocols was conducted before recruitment with research assistants blinded to the method assigned to patients. A block design was not used. If the protocol was to be self-administered, the patient completed the questionnaire herself. When necessary, the research assistant explained the questions to the participant. Patients assigned to be interviewed by medical staff were directed to one of the medical staff, who administered the screening tool, reviewed the results, and intervened if necessary. For patients assigned to be interviewed by a physician, a similar procedure was performed. In all 3 protocols, participants were provided with domestic violence materials by research assistants. The physicians were informed of the written results of screening. Those patients whose screening test was positive for domestic violence received an intervention by the physicians. The time taken to provide materials on domestic violence was included in the estimate of time for screening, whereas the time taken to intervene with those who disclosed domestic violence was not included.
After the health care visit, the research assistants distributed self-administered questionnaires to the participants in a private room. This postscreening questionnaire sought more details about the domestic violence and assessed comfort level and time spent screening. After patients completed the questionnaire, the women received a stipend of $10 for their participation. At the end of the study, medical staff and physicians completed a self-administered questionnaire on their time spent screening and their overall comfort with screening but not about a specific patient.
Data Collection
Patients were screened for domestic violence using 2 brief screening tools: HITS (hurt-insult-threaten-scream)18 and WAST (Woman Abuse Screening Tool)-Short16 (Supplemental Appendix at: http://www.annfammed.org/cgi/content/full/5/5/430/DC1). HITS is one of the shortest screening tools, forms an easily remembered acronym, has been tested with diverse populations, and has been tested and used in family medicine practices. Answers were summed to form an interval scale of the total HITS score, which could range from 4 to 20. Using a cutoff score of 10.5, Sherin et al found that HITS accurately classified 91% of nonvictims and 96% of victims.18 HITS has a Cronbach’s α of 0.80 and is highly correlated with the Conflict Tactics Scales (r = 0.85).18,19
WAST-Short consists of 2 items from the 8-item WAST. Women responded to the 2 items with a 3-point response set and met the criteria for domestic violence exposure if they answered “a lot of tension/ great difficulty” to either question. The remaining 6 items were included in the postscreening questionnaire to validate results from the domestic violence screening. For the 8-item WAST, answers were summed to form an interval scale, ranging from 3 to 24. The WAST has a reliability of 0.75, and abused women identified by WAST-Short score significantly higher on WAST than women who were not abused.10 WAST has been tested in only predominantly white and middle-class populations, however.10
Women who had positive findings on HITS or WAST-Short in the 3 protocols met the criteria for domestic violence exposure.
Data on patient comfort levels with the screening instruments, the screening method, and time spent screening were collected using a patient postscreening questionnaire. Questions addressing comfort with screening were adapted from previous studies,10,16 with answers ranging from not at all (1) to very comfortable (4). Patient comfort levels with each item of HITS and WAST were assessed in the postscreening questionnaire (Supplemental Appendix). Answers were summed to form interval scales of the total HITS, WAST, and overall comfort scores. We included a question on how comfortable the patient was with the assigned screening method. A clinician survey assessed the physicians’ and medical staff’s comfort level with the screening tools and the assigned screening protocol. Scales similar to the patient comfort scales were used.
We calculated the sample size based on a previous study by the authors and the literature.10,13,19 We expected patient disclosure rates of 6% for the self-administered questionnaire, 16% for the medical staff interview, and 9% for the physician interview. We hypothesized 0.3 differences in comfort level scores (3.0, 3.3, 3.6, respectively; SD = 0.5). Screening for domestic violence with 167 women from each method for a total of 501 provides more than 80% power to detect such differences at α = .05 (2-tailed test). Institutional Review Board approval for this study was obtained.
Analysis
Analysis was done using SPSS version 14.0.2 (SPSS, Inc, Chicago, Ill). Outcome measures were domestic violence disclosure, patient or clinician comfort level, and time spent screening. To determine the reliability and validity of HITS and WAST-Short, we calculated Cronbach’s coefficient α, correlations of the 2 instruments with WAST, and assessed the relation of domestic violence disclosure by HITS and WAST-Short to WAST scores. Then, χ2 tests and ANOVA were conducted to compare differences in domestic violence disclosure, patient and clinician comfort levels, and time spent screening among the 3 protocols.
RESULTS
Participants
During the 10 months in the practices, 730 women were eligible to participate in the study. Of these women, 200 refused to participate, and 7 did not complete the questionnaire because of the waiting time for a private room. A total of 523 (72%) eligible patients participated in the study. Institutional Review Board regulations did not allow us to collect demographic data for nonrespondents; however, percentages of African American and Hispanic women in the sample and the 4 practices were similar (84% and 86%, respectively).
Table 1 ▶ displays the demographic characteristics of participants. The 3 randomly allocated groups were similar on all but 2 variables. Women interviewed by medical staff were more likely to be employed (P = .005), and those who completed self-administered questionnaires had visited the practice more often in the previous year (P = .005).
Table 1.
Sample Characteristics of Participants by Domestic Violence Screening Protocol
| Variable | Total n=523 | Self-Report n=173 | Medical Staff Interview n=169 | Physician Interview n=181 | P Value |
| Race/ethnicity, % | |||||
| White | 11.7 | 15.1 | 10.7 | 9.4 | .769 |
| African American | 70.6 | 67.4 | 70.8 | 73.3 | |
| Hispanic | 13.8 | 13.4 | 14.9 | 13.3 | |
| Other | 3.8 | 4.1 | 3.6 | 3.9 | |
| Age, mean, y | 35.6 | 35.8 | 35.9 | 35.3 | .886 |
| Completed college, % | 29.5 | 32.4 | 29.0 | 27.2 | .561 |
| Income , mean, $ | 20,423 | 20,232 | 20,650 | 20,388 | .974 |
| Employed (including part-time), % | 72.6 | 64.5 | 80.4 | 72.9 | .005 |
| Married, % | 33.4 | 28.3 | 38.9 | 33.1 | .117 |
| Currently pregnant, % | 4.5 | 4.1 | 4.8 | 4.5 | .953 |
| Length of the relationship, mean, y | 8.2 | 7.8 | 8.9 | 7.9 | .586 |
| Medicare/Medicaid, % | 51.5 | 57.6 | 47.3 | 49.7 | .140 |
| New patient, % | 19.8 | 16.8 | 24.6 | 18.4 | .167 |
| Visits in the past year, mean, No. | 4.3 | 4.8 | 4.2 | 3.8 | .005 |
Disclosure of Domestic Violence
Table 2 ▶ shows no difference in the prevalence of a positive screening result for domestic violence among 3 methods of administering HITS and WAST-Short. Overall, 14.2% of women had positive findings on 1 or both instruments. A higher proportion of women had positive findings with WAST-Short than with HITS (12.5% vs 6.3%, respectively), perhaps because the WAST-Short questions are more general.
Table 2.
Patient Disclosure and Patient and Clinician Comfort Level, by Screening Protocol
| Variable | Total | Self-Report | Medical Staff Interview | Physician Interview | P Value |
| Patients, No. | 523 | 173 | 169 | 181 | |
| Patient domestic violence disclosure, % | |||||
| HITS | 6.3 | 6.4 | 5.9 | 6.7 | .959 |
| WAST-Short | 12.5 | 13.3 | 11.8 | 12.2 | .914 |
| Overall | 14.2 | 14.5 | 13.0 | 15.0 | .862 |
| Patient comfort with screening tools, mean, score* | |||||
| HITS | 3.5 | 3.5 | 3.6 | 3.6 | .434 |
| WAST-Short | 3.6 | 3.5 | 3.6 | 3.6 | .519 |
| Overall | 3.5 | 3.5 | 3.6 | 3.6 | .446 |
| Patient comfort with screening method, mean, score*†‡ | 3.4 | 3.4 | 3.5 | 3.4 | .656 |
| Patient perception of helpfulness for screening, mean, score‡ | 3.2 | 3.3 | 3.1 | 3.2 | .453 |
| Time spent screening, min | 4.4 | 4.8 | 4.4 | 4.0 | .100 |
| Clinicians, No. | 33 | N/A | 14 | 19 | |
| Clinician comfort with screening methods, mean, score*§ | |||||
| Self-administered | 3.4 | N/A | 3.2 | 3.6 | .181 |
| Medical staff | 3.1 | N/A | 3.1 | 3.2 | .801 |
| Physician | 3.4 | N/A | 3.4 | 3.4 | .788 |
| Clinician comfort with screening tools, mean, score*¶ | |||||
| HITS | 3.1 | N/A | 2.8 | 3.2 | .184 |
| WAST-Short | 3.3 | N/A | 3.0 | 3.5 | .039 |
| Overall | 3.1 | N/A | 2.9 | 3.3 | .100 |
HITS = hurt, insult, threaten, scream; N/A = not applicable; WAST-Short = 2-items of the Woman Abuse Screening Tool.
* Range: not at all comfortable (1) to very comfortable (4).
† Most patients (93.4%) reported being comfortable with the assigned protocol.
‡ Women who disclosed domestic violence and those who did not were similar in perception of helpfulness for screening and comfort with screening across methods; the only exception was those who disclosed domestic violence were slightly less comfortable with medical staff screening (P=.021).
§ Most clinicians (84.5%) were comfortable with the screening methods.
¶ Subgroup analysis indicated that physicians preferred WAST-Short to HITS (P = .043) and self-administered questionnaire to medical staff interview (P=.007).
Internal Reliability and Validity of Instruments
The internal reliability of the short screening instruments was good, and each was highly correlated with the WAST total score. Cronbach’s α was .79 for HITS and .80 for WAST. The correlations of HITS and WAST-Short total scores with WAST total scores were 0.77 (P <.001) and 0.81 (P <.001), respectively. Those who had positive results on HITS or WAST-Short had WAST total scores that were significantly higher than those who had negative results (P <.001 for both instruments). Cronbach’s α was .97 for the patient overall comfort scale and .95 for the clinician overall comfort scale.
Patient Comfort and Time Spent Screening
Most patients (93.4%; total n = 523) reported being comfortable with the assigned protocol. Comparisons of the mean scores of patient comfort showed no differences in HITS, WAST-Short, and overall comfort among protocols. Women whose screening results were positive for domestic violence and those whose were not were similar in perception of helpfulness of screening and comfort with screening across methods. One exception was that those with positive screening results for domestic violence were slightly less comfortable with medical staff screening (P = .021). Time spent screening ranged from 2 to 15 minutes and was similar among the 3 methods.
Clinician Comfort
Most clinicians (84.5%; total n = 33) were comfortable with the screening methods regardless of whether the clinician interviewed the patient or the questionnaire was self-administered. Comfort levels with each screening protocol were similar for physicians and medical staff across methods. Physicians and medical staff were comfortable with the screening tools (mean score = 3.1), although physicians were slightly more comfortable with WAST-Short compared with the medical staff (P = .039). Subgroup analysis indicated that physicians preferred WAST-Short to HITS (P = .043), and self-administered questionnaire to medical staff interview (P = .007).
DISCUSSION
Our findings provide support that rates of domestic violence disclosure are similar with self-administered screening, medical staff interview, and physician interview. The prevalence rate of domestic violence in our study is similar to findings from previous studies.12–14 Overall, 1 in 7 women in intimate relationships had positive findings for domestic violence. Consistent with prior studies, our findings show that patients and clinicians are comfortable with domestic violence screening.10,13–17 Although MacMillan et al found that a face-to-face approach was less preferred by patients,12 we found that patient comfort levels were similar among clinician interviews and self-completed questionnaires. We also found that physicians were comfortable regardless of screening tools and screening methods. This study provides implications for cost savings if self-administered screening tools are used.
This study has some limitations. Provision of a stipend might affect the participant’s rating of their comfort with screening. Even so, the stipend did not seem to affect the comparative ratings of the 3 screening protocols. There was no validation of the time spent; however, the reported time is reasonable given the brevity of the questionnaire. Nonparticipants and participants might differ in demographic characteristics and in abuse, which may introduce unknown bias. Our study only screened women patients, because women are 7 to 14 times more likely than men to suffer injuries.20 We did not have physicians and medical staff assess their comfort with screening each patient. Finally, this study was conducted in urban clinical settings with predominantly minority patient populations, indicating that WAST and WAST-Short may be acceptable screening instruments in such settings.
In conclusion, domestic violence is common in urban family medicine settings. Screening patients for domestic violence using a self-administered questionnaire is as effective as clinician screening in terms of disclosure, comfort, and time spent screening. Brief screening tools such as those used in this study can be helpful to busy clinicians, but in practice, clinicians would still need to conduct further assessment to confirm the domestic violence victim’s status.
Acknowledgments
The authors thank the departmental writing group for their comments on an earlier version of this manuscript.
Conflicts of interest: none reported
Funding support: Preparation of this article was supported by a grant from the American Academy of Family Physicians Foundation (#G0415).
REFERENCES
- 1.Coker AL, Reeder CE, Fadden MK, Smith PH. Physical partner violence and Medicaid utilization and expenditures. Public Health Rep. 2004;119(6):557–567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Naumann P, Langford D, Torres S, Campbell J, Glass N. Women battering in primary care practice. Fam Pract. 1999;16(4):343–352. [DOI] [PubMed] [Google Scholar]
- 3.Friedman LS, Samet JH, Roberts MS, Hudlin M, Hans P. Inquiry about victimization experiences. A survey of patient preferences and physician practices. Arch Intern Med. 1992;152(6):1186–1190. [DOI] [PubMed] [Google Scholar]
- 4.Thompson RS, Rivara FP, Thompson DC, et al. Identification and management of domestic violence: a randomized trial. Am J Prev Med. 2000;19(4):253–263. [DOI] [PubMed] [Google Scholar]
- 5.Erickson MJ, Hill TD, Siegel RM. Barriers to domestic violence screening in the pediatric setting. Pediatrics. 2001;108(1):98–102. [DOI] [PubMed] [Google Scholar]
- 6.Cummins A, Little D, Seagrave M, Ricken A, Esparza V, Richardson-Nassif K (2002). Vermont Family Practitioners’ Perceptions on Intimate Partner Violence. North American Primary Care Research Group (NAPCRG) 30th Annual Meeting, New Orleans, LA.
- 7.Gerber MR, Leiter KS, Hermann RC, Bor DH. How and why community hospital clinicians document a positive screen for intimate partner violence: a cross-sectional study. BMC Fam Pract. 2005;6:48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McGrath ME, Bettacchi A, Duffy SJ, Peipert JF, Becker BM, St Angelo L. Violence against women: provider barriers to intervention in emergency departments. Acad Emerg Med. 1997;4(4):297–300. [DOI] [PubMed] [Google Scholar]
- 9.Rodriguez MA, Quiroga SS, Bauer HM. Breaking the silence. Battered women’s perspectives on medical care. Arch Fam Med. 1996;5(3):153–158. [DOI] [PubMed] [Google Scholar]
- 10.Brown JB, Lent B, Schmidt G, Sas G. Application of the Woman Abuse Screening Tool (WAST) and WAST-Short in the family practice setting. J Fam Pract. 2000;49(10):896–903. [PubMed] [Google Scholar]
- 11.Ramsay J, Richardson J, Carter YH, Davidson LL, Feder G. Should health professionals screen women for domestic violence? Systematic review. BMJ. 2002;325(7359):314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.MacMillan HL, Wathen CN, Jamieson E, et al. Approaches to screening for intimate partner violence in health care settings: a randomized trial. JAMA. 2006;296(5):530–536. [DOI] [PubMed] [Google Scholar]
- 13.McFarlane J, Christoffel K, Bateman L, Miller V, Bullock L. Assessing for abuse: self-report versus nurse interview. Public Health Nurs. 1991;8(4):245–250. [DOI] [PubMed] [Google Scholar]
- 14.Canterino JC, VanHorn LG, Harrigan JT, Ananth CV, Vintzileos AM. Domestic abuse in pregnancy: A comparison of a self-completed domestic abuse questionnaire with a directed interview. Am J Obstet Gynecol. 1999;181(5 Pt 1):1049–1051. [DOI] [PubMed] [Google Scholar]
- 15.Fogarty CT, Brown JB. Screening for abuse in Spanish-speaking women. J Am Board Fam Pract. 2002;15(2):101–111. [PubMed] [Google Scholar]
- 16.Brown JB, Lent B, Brett PJ, Sas G, Pederson LL. Development of the Woman Abuse Screening Tool for use in family practice. Fam Med. 1996;28(6):422–428. [PubMed] [Google Scholar]
- 17.Gerbert B, Bronstone A, Pantilat S, McPhee S, Allerton M, Moe J. When asked, patients tell: disclosure of sensitive health-risk behaviors. Med Care. 1999;37(1):104–111. [DOI] [PubMed] [Google Scholar]
- 18.Sherin KM, Sinacore JM, Li XQ, Zitter RE, Shakil A. HITS: a short domestic violence screening tool for use in a family practice setting. Fam Med. 1998;30(7):508–512. [PubMed] [Google Scholar]
- 19.Chen PH, Rovi S, Vega M, Jacobs A, Johnson MS. Screening for domestic violence in a predominantly Hispanic clinical setting. Fam Pract. 2005;22(6):617–623. [DOI] [PubMed] [Google Scholar]
- 20.Screening for family and intimate partner violence: recommendation statement. Ann Intern Med. 2004;140(5):382–386. [DOI] [PubMed] [Google Scholar]


