Abstract
Purpose
The primary research hypothesis was that the magnitude and duration of the perceived burden from altered sensation reported by patients following bilateral sagittal split osteotomy (BSSO) and trauma to the third division of the trigeminal nerve is lessened when facial sensory retraining exercises are performed in conjunction with standard opening exercises as compared to standard opening exercises alone.
Subjects and Methods
186 subjects were enrolled in a multi-center double-blind two parallel group stratified block randomized clinical trial. Oral and facial pain, unusual sensations, numbness and loss of sensitivity, were scored from “no problem” to “serious problem” before surgery, 1,3, and 6 months after surgery.
Analysis
A proportional odds model for the ordered multinomial response was used to compare the responses of the two exercise groups.
Results
The two exercise groups did not differ significantly at any postsurgical time in the perceived problem level from mouth or face pain. The difference between the two groups at each visit was not statistically significant for unusual sensations although the trend was for the sensory retraining group to have a higher likelihood of reporting fewer problems. By 6 months, the likelihood of a subject reporting lower problem or interference level related to numbness or less lip sensitivity was significantly higher in the sensory-retraining group, approximately twice that of the opening exercise only group.
Conclusion
The results from this clinical trial support the premise that a simple noninvasive exercise program initiated shortly after orthognathic surgery can lessen the objectionable impression of negative altered sensations.
Introduction
Although there are no exact numbers available, it is likely that more than a million people in the U.S. suffer from altered facial sensation in a given year. Over 50% of mandibular fractures between the mental foramen and sigmoid notch, (1,2) 38% of posterior mandibular implant placements, (3) 1:750,000 of mandibular nerve blocks, (4) and .5 to 4% of third molar extractions (5) result in long-term facial sensory impairment. Virtually all patients experience at least temporary neurosensory impairment following orthognathic surgery for correction of developmental dentoskeletal disharmonies (6) and over half may never recover normal orofacial sensory function (7).
Pharmacological, psychological, and surgical treatments have been evaluated as methods to promote recovery from altered facial sensation, (8,9) but little systematic evidence exists on the success of simpler and less intrusive therapies such as sensory retraining. Sensory retraining or sensory reeducation has been used, with documented clinical success, in patients with injured hand nerves since the 1960's. (10-15) Anecdotally, the use of sensory retraining has been reported in patients with injured trigeminal nerves. (16,17) The intent of this physical/behavioral therapy is to improve the patient's ability to interpret the altered sensory response from injured sensory nerves and to improve the patient's perception of function.
Laboratory and animal research has shown that sensory training enhances central nervous system reorganization, and in particular that of the somatosensory cortex. (18-20) The reorganization and changes in the response properties of individual cortical neurons strongly suggest that altered sensory signals are better interpreted and translated into functionally meaningful motor functions. If the clinical findings from the hand surgery literature apply to the trigeminal region as well, sensory retraining would be expected to help patients with altered oral-facial sensation following nerve injury by i) improving patients' ability to interpret lip/chin sensations and movements, ii) improving perioral motor function subjectively and objectively, and iii) lessening the objectionable impression of numb/paresthetic sensations in the lip and chin.
Candidates for orthognathic surgery constitute an ideal subject group for the investigation of novel putative therapies such as sensory retraining for at least two reasons. First, baseline data can be obtained before altered sensation develops, i.e. presurgically, and these baseline responses can be compared subsequently to those obtained during the severe loss in sensation that often occurs immediately after surgery and to responses obtained over longer periods of time during the recovery process. Second, the surgery is elective, and the patients are typically healthy young adults without complicated medical and psychological histories, complications which would make detection of a therapeutic effect more difficult. To evaluate these possibilities, we conducted a multi-center double blind parallel two-arm stratified block randomized clinical trial. The intent was to assess whether the magnitude and duration of patient-reported burden from altered sensation are lessened when facial sensory retraining exercises are performed in conjunction with standard opening exercises than when the opening exercises are performed alone. The analyses presented in this paper strictly focus on ‘burden’ as defined by the patient report of objectionable impressions of numb or unusual sensations, including pain, in the facial, perioral and oral regions. Subsequent manuscripts will address patient-reported burden from altered orofacial function (e.g., perceived difficulty with speaking or drooling) and burden defined by nerve-injury associated alterations in threshold measures of sensory function (e.g., altered touch detection and two-point discrimination thresholds).
Methods and Materials
Subjects
Subjects were screened at a university based clinic and a community based practice. Written consent/assent (and parental permission if the subject was younger than 18) was obtained in accordance with the policies of the Biomedical Institutional Review Board. A HIPAA authorization was obtained for use of protected health information.
Subjects, between 13 and 50 scheduled for a BSSO either alone or combined with a maxillary procedure for treatment of a developmental dentofacial disharmony, were enrolled. Genioplasty was permitted but implant surgery to the chin was not. Subjects were excluded if they had a congenital anomaly or acute trauma; had had previous facial surgery; were pregnant; reported moderate to severe numbness or unusual feeling on the face prior to surgery (added in September, 2002); had a medical condition associated with systemic neuropathy (ex., diabetes, hypertension, kidney problems); or were unable to follow written English instructions or unwilling to sign informed consent. The eligibility of subjects who, at baseline, self-reported on the SCL-90-R indications of homicidality or suicidality (a score of ‘2’ on either item) was determined after a consultation with a licensed mental health professional.
Enrollment
Enrollment began December, 2001 and closed April 1, 2005. One hundred ninety-one subjects gave consent. Five subjects are not included in the intent-to-treat analysis: three had not had surgery by the closing date; one withdrew after baseline data collection; and one with an unreported medical condition (meeting exclusion criteria) withdrew after the first level of the exercise program. The number of subjects enrolled at each of the two centers was approximately equal (Table 1).
Table 1.
Demographic and surgical characteristics for the entire sample and for subjects randomized to each of the exercise groups.
| All Subjects | Sensory Retraining (+ Opening Exercises ) | Opening Exercises Only | P-value | |
|---|---|---|---|---|
| Age | ||||
| Mean | 25.1 | 24.6 | 25.5 | .61 |
| Std | 11.8 | 12.1 | 11.5 | |
| % Female | 71 | 72 | 70 | .82 |
| % Caucasian | 94 | 95 | 93 | .58 |
| % Mandible Only | 61 | 62 | 61 | .91 |
| % Genioplasty | 29 | 29 | 29 | .93 |
| % Center 1 | 49.5 | 48.9 | 50 | .88 |
Randomization
Subjects were randomized to one of the two exercise programs using a stratified block randomization. The stratification factors for randomization were center, the surgical procedure (mandibular only vs. two-jaw osteotomies) and the addition of a genioplasty (yes vs. no). These stratification factors were selected based on previous studies indicating that the rate of sensory recovery is affected by the type of surgery performed and the number of procedures performed in the same area (21-23). Stratification was performed for the purpose of balancing the assignment of the two exercise groups within these characteristics at each enrollment center. Separate randomization schedules were constructed for each center using randomly alternating, permuted blocks of 4 and 8, assuring that approximately equal numbers of sensory-retraining and opening-only exercise assignments would be made at each center. The block size was randomly selected to prohibit determination of the next likely assignment. The randomization schedule was prepared using Proc Plan (24) for each of the 8 (2 centers X 2 surgical procedures x 2 genioplasty additions) stratum.
The randomization schedule was maintained by the coordinator at each center who also acted as the exercise trainer. The assignment labels were kept in envelopes in numerical sequence separately by stratum. A subject was assigned to an exercise group based on the next sequential treatment assignment number from the appropriate stratum envelope and the assignment recorded in a patient assignment log. The assignment number but not the exercise group was recorded in the subject's casebook.
Misclassifications
Twelve subjects were incorrectly randomized. In the original protocol, the classification of the surgery procedure was determined from the surgical treatment plan. When it was noted that the actual surgery performed did not always agree with the surgical treatment plan, the protocol was amended so the classification was determined from operative notes detailing the actual surgery performed. For all analyses, however, subjects were categorized according to the surgical procedure used for randomization purposes (intention-to-treat).
Exercise Programs and Training
There were three, time-dependent levels of instructions for the sensory-retraining and opening-only exercise programs given during training sessions at 1 week, 1 month (4 to 6 weeks), and 3 months after surgery. The time points were selected based on their use in clinical studies of the impact of sensory reeducation in patients with injured median or ulnar nerve (11) and in clinical studies of sensory impairment in patients following orthognathic surgery. (25-28) The exercises were started early after surgery -- 1 week when the affected area was often insensate -- to obtain the maximum affect of sensory retraining.(29) The three levels of sensory retraining were designed to increasingly challenge patients in a similar manner to that of the early and late phases of sensory education commonly used after injuries to the hand nerves.(12,14,15,30) Patients learned to discriminate moving from non-moving touch, orientation of moving touch, and direction of moving touch, in turn. The opening-only exercise program was based on current clinical practice at our Institution. A synopsis of the instructions given at each session is provided in Table 2. 1The subject viewed a video tape explaining and demonstrating the exercises appropriate for that session. The exercise trainer answered any questions and verified the subject could perform the exercises.
Table 2.
Synopsis of instructions given to the opening-only exercise group and the sensory-retraining group at each of the 3 training sessions. Subjects in the sensory-retraining group also were instructed and ask to perform the opening exercises.
| Visit | Opening Exercises (3x/day) | Sensory Retraining Exercises (2x/day) |
|---|---|---|
|
| ||
| 1 Week | -Simple open/close and side/side using jaw muscles only | -Alternate simple touch and stroke with cosmetic brush (Motion training). |
| -Movement until discomfort only not till pain | -Feedback from mirror. | |
| -“Hold and Relax” | -Visualization with eyes closed. | |
|
| ||
| 1 Month | -“Hold and Relax” | -Alternate up/down and side/side strokes (Orientation training). |
| -“Finger Stretch” for simple open/close | -Feedback from mirror. | |
| -Movement until discomfort only not till pain | -Visualization with eyes closed. | |
|
| ||
| 3 Months | -If Opening ≥35mm | -Alternate up→down and down→up strokes (Directionality training). |
| Occasionally repeat exercises. | -Feedback from mirror. | |
| -If Opening < 35mm | -Visualization with eyes closed. | |
| Increase frequency of exercises, | ||
Before each exercise session, the trainer consulted with the attending surgeon regarding any instructions for removal of elastics and contra-indications to the exercises. As a result, the exercise program was not implemented according to protocol for eleven subjects (6%): Ten were not permitted to start the exercise program at 1 week postsurgery for clinical reasons, and one had the exercise program delayed or interrupted. Six of these subjects had been assigned to the sensory-retraining and five to the opening-only exercise groups. There were no serious adverse events.
Outcome Measures
Prior to surgery and at 1 month (4 to 6 weeks), 3 months, and 6 months following surgery, participants were appointed for data collection visits. Two patient perception questionnaires were completed at each visit: Postsurgical Perceptions (PSP) and Problems with Facial Sensation(PFS) (31). Responses to the items on Postsurgical Perceptions reflected the level of interference of post-surgery sensory alteration on the patient's daily routine, health, and quality of life. Responses to the items on the Problems with Facial Sensation reflected the level of interference on different aspects of orofacial sensation and function. For both questionnaires, the individual items were rated from “no problem” (1) to “serious problem” (7) and subjects were instructed to report the magnitude of the problem during the past two weeks.
Based on the literature, five items (Table 3) were theorized to be linked to the hypothesized effect of sensory retraining. These items assessed the patient's perception of difficulty with pain inside the mouth (Mouth Pain), pain in facial areas (Face Pain), unusual feelings in the face or mouth (Unusual Feelings), numbness in facial areas or around the mouth (Numbness), and loss of sensitivity in the lips to touch as, e.g., when using a straw or kissing (Less Lip Sensitivity). A visit burden score for altered sensation was calculated as the average of the responses to the five items.
Table 3.
Five items selected from the Patient Perception Questionnaires for evaluation of perceived problems with altered sensation.
| Instructions: Doctors need to know when patients have problems after orthognathic surgery. Listed below are problems that some patients have mentioned as being a concern after orthognathic surgery. Choose the response which best describes how much of a problem in each area you have experienced in the past two weeks. |
|
| Each item is rated from No Problem (1) to Serious Problem (7). |
Three subjects did not complete data collection at 3 months and three at 6 months. Missing values were assigned the score of the nearest preceding data collection visit with a recorded value (last observation carried forward).
Masking
The attending surgeon and the research associate responsible for data collection were masked to the exercise group assignment throughout the entire clinical trial. The statistician was masked to the subject's assignment until all subjects had completed the 6 month data collection visit.
Sample Size Determination
Initial sample size calculations were performed based on variability estimates from a previous study using the PSP and PFS. The two-group repeated measures ANOVA with the Greenhouse-Geisser correction, computed using methods taken from Muller and Barton (32) in Nquery, Version 4 (33) was used.
Since the primary interest was the comparison of the exercise group effect on the burden scores summed across visits, the sample size of 85 was chosen to provide 90% power with .05 two-sided significance to detect a marginal mean difference between the exercise groups with a moderate effect size of 0.4 (34). Assuming a retention rate at two years of 70%, the target sample size per group was set at 122 or a total of 244.
An interim descriptive analysis of unmasked data from the clinical trial confirmed the initial estimates of standard deviations and correlational pattern as reasonably accurate and the proposed effective sample size of 85 per group to be appropriate. Since by January 2005, only one subject had withdrawn from the study and the intermittent missing visit rate did not exceed 5% for any visit, the Data Safety and Monitoring Board approved a change in the proposed retention rate to 90% and a decrease in the target recruitment goal to 180 participants.
Statistical Analysis
A cumulative burden score was calculated as the sum of the visit-specific burden scores at 1, 3, and 6 months to serve as the subject-based, overall outcome measure. By placing equal emphasis on the three time points, the measure represented the total burden of altered sensation reported by each patient during the first six months after orthognathic surgery.
The cumulative burden score from the two exercise groups were compared using a nonparametric analysis of covariance for sets of two-way tables (35). The presurgery (baseline) data served as the covariate, giving results that statistically adjust for different baseline values of burden among subjects. Stratification factors (number of jaws operated and presence of a genioplasty) were also included. Details of the procedure are provided in the appendix. Level of significance was set at 0.05.
Although succinct, the cumulative burden score may not be sufficiently sensitive to detect differences between the two exercise groups regarding the impact of altered sensation on patients' quality of life. Consideration of only the cumulative or the visit-specific burden scores may mask differences between the two exercise groups in recovery that occur for some but not all of the five items. It is also possible that group differences on two or more items could be reversed in sign, yielding the same cumulative or visit-specific burden scores.
For this reason, a secondary repeated measures analysis was performed for each of the five items using a proportional odds model for the ordered multinomial response fit with generalized estimating equations implemented with an across-time working independence correlation structure (35-37). Each model included the stratification factors (number of jaws operated and presence of a genioplasty), visit (1 month, 3 months, and 6 months), the visit-by-exercise group interaction, as well as the primary explanatory variable, exercise group. Details of the procedure are provided in the appendix. The stratification factors were maintained in all analyses as design features even though neither number of jaws operated nor presence of genioplasty was significantly related to the perception of problems (Appendix). Level of significance was set at 0.05.
Results
186 subjects gave consent for the Sensory Retraining Clinical Trial, were randomized to exercise programs (sensory retraining exercises in conjunction with standard opening exercises or standard opening exercises only), and completed the first exercise training session. The demographic characteristics of the subjects for the entire sample as well as the comparison of the demographic characteristics of the two exercise groups as randomized are presented in Table 1. As expected based on randomization, the percentages for each of the stratification factors were very similar for the two exercise groups. The two groups were also similar in average age and percentage of females and Caucasians.
Cumulative Burden Score
The cumulative burden score was not significantly different (p = 0.43) between the two exercise groups (Table 4). However, the recovery trend over the six month period differed substantially for the five item (Figures 1-5).
Table 4.
Percentiles (25th, 50th, 75th) for the Pre-surgery (baseline) and Cumulative Post-surgery Burden from altered sensation by Exercise Group
| Exercise Group | Pre-surgery | Cumulative Post-surgery | ||||
|---|---|---|---|---|---|---|
| 25th | median | 75th | 25th | median | 75th | |
| Opening Only | 1.0 | 1.0 | 1.6 | 5.0 | 7.5 | 9.4 |
| Sensory Retraining | 1.0 | 1.0 | 1.4 | 5.2 | 6.4 | 8.7 |
Figure 1.
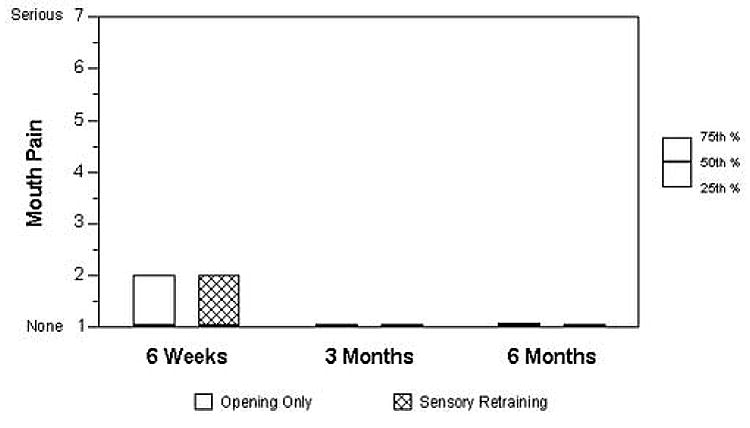
Descriptive Statistics Comparing the Sensory-Retraining and Opening-Only Exercise Groups for the Problem or Interference Level Associated with Pain inside the Mouth over the six Month Post-surgical Period
Figure 5.
Descriptive Statistics Comparing the Sensory-Retraining and Opening-Only Exercise Groups for the Problem or Interference Level Associated with Less Lip Sensitivity over the 6 Month Post-surgical Period
Mouth and Face Pain
The subjects' perception of problems in everyday life related to mouth and face pain decreased rapidly. By three months, 75% of all subjects reported no problem or interference related to pain inside the mouth (Table 5; Figure 1) and by six months, more than 75% reported no problem or interference related to pain in facial areas (Table 5; Figure 2). The proportional odds model incorporating the time-by-exercise group interaction indicated no statistically significant difference in the problem level from mouth pain or face pain between the two exercise groups at any time (The P values for the repeated measures proportional odds models are provided in the Appendix).
Table 5.
Percentage of patients who reported No (1), Little-to-Somewhat (2-4), or Moderate-to-Severe (5-7) Difficulty or Problem Level experienced in the past two weeks with altered sensations or pain.
| PAS Item | 1 Month | 3 Months | 6 Months | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No | L/S | M/S | No | L/S | M/S | No | L/S | M/S | ||||||||||
| O | S | O | S | O | S | O | S | O | S | O | S | O | S | O | S | O | S | |
| Mouth Pain | 60 | 57 | 35 | 36 | 5 | 8 | 79 | 80 | 17 | 16 | 4 | 4 | 88 | 78 | 9 | 21 | 3 | 1 |
| Facial Pain | 51 | 53 | 42 | 38 | 7 | 9 | 68 | 74 | 27 | 22 | 5 | 3 | 79 | 82 | 18 | 15 | 2 | 2 |
| Unusual Feelings | 22 | 16 | 55 | 53 | 22 | 30 | 30 | 43 | 58 | 47 | 12 | 10 | 51 | 57 | 47 | 37 | 2 | 6 |
| Numbness | 6 | 4 | 46 | 42 | 48 | 53 | 12 | 19 | 63 | 62 | 25 | 19 | 23 | 36 | 68 | 51 | 9 | 13 |
| Less Lip Sensitivity | 21 | 21 | 48 | 46 | 31 | 34 | 33 | 39 | 49 | 46 | 18 | 16 | 38 | 56 | 55 | 34 | 7 | 10 |
Figure 2.
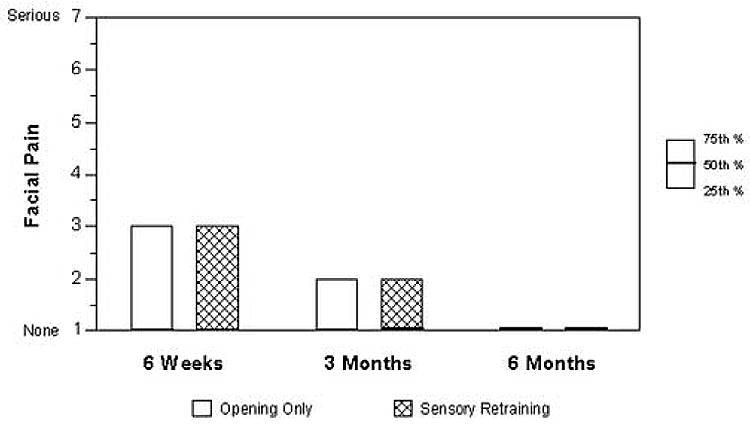
Descriptive Statistics Comparing the Sensory-Retraining and Opening-Only Exercise Groups for the Problem or Interference Level Associated with Pain on the face over the six Month Post-surgical Period
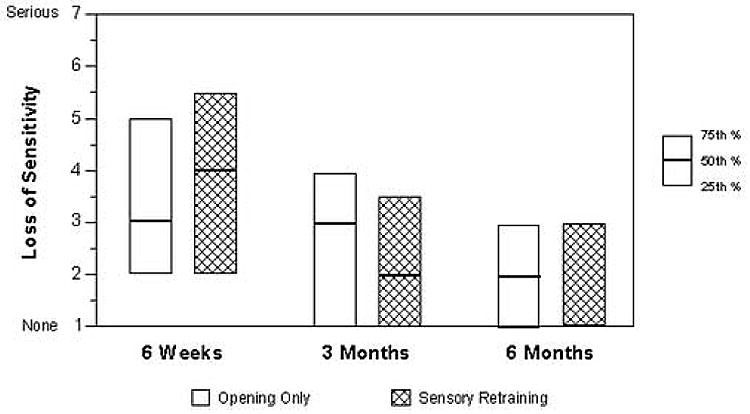
Unusual Feelings
In contrast to pain, approximately half of the subjects continued to report at least mild interference in everyday life related to unusual feelings in the face or mouth at 6 months postsurgery (Table 5;Figure 3). The distributions of responses were slightly higher at 1 month and slightly lower at the 3 month and 6 month visits in the sensory-retraining group. At 6 months, 52% of the opening-only group and 58% of the sensory-retraining group reported no problem related to unusual feelings. Although the time-by-exercise group interaction was statistically significant (Appendix), the difference between the two groups at each visit time was not statistically significant (Table 6; Figure 3).
Figure 3.
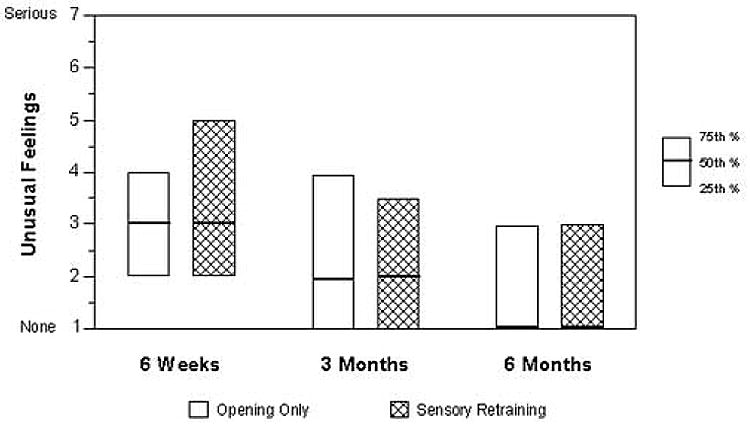
Descriptive Statistics Comparing the Sensory-Retraining and Opening-Only Exercise Groups for the Problem or Interference Level Associated with “Unusual Feelings” over the 6 Month Post-surgical Period
Table 6.
Cumulative Odds Ratio Estimates and 95% Confidence Intervals for the Comparison of the Two Exercise Groups at Each of the Three Post-Op Visits. The odds ratios indicate the odds of subjects in the sensory-retraining group reporting lower problem levels related to the altered sensation and pain items than those in the opening-only exercise group
| Unusual Feelings | Numbness | Less Lip Sensitivity | ||||
|---|---|---|---|---|---|---|
| Odds Ratio (se) | 95% CI | Odds Ratio(se) | 95% CI | Odds Ratio(se) | 95% CI | |
| 1 Month | 0.67 (0.17) | 0.40, 1.11 | 0.95 (0.25) | 0.57, 1.58 | 0.87 (0.23) | 0.52, 1.45 |
| 3 Months | 1.58 (0.42) | 0.93, 2.66 | 1.50 (0.39) | 0.90, 2.50 | 1.54 (0.41) | 0.91, 2.59 |
| 6 Months | 1.20 (0.33) | 0.69, 2.07 | 1.92 (0.51) | 1.14, 3.25 | 1.83 (0.50) | 1.07, 3.13 |
Numbness and Less Lip Sensitivity
More than two-thirds of all subjects reported problems or interference in everyday life related to numbness in facial areas or around the mouth at 6 months postsurgery (Table 5;Figure 4); and approximately half of the subjects continued to report problems related to loss of sensitivity in the lips (Table 5;Figure 5). For the two items that specifically target negative symptoms of altered sensation, the median problem level reported was slightly higher in the sensory-retraining group at 1 month, but lower by 6 months. At 6 months, only 22% percent of the subjects in the opening-only exercise group reported no problem or interference in everyday life related to numbness, while 37% of the subjects in the sensory-retraining group reported no problem (Table 5). A similar difference between groups was observed for loss of sensitivity in the lips (38% no problem vs. 57%). The proportional odds model indicated a statistically significant time-by-exercise group interaction (Appendix) for these negative symptom items. The two exercise groups did not differ statistically at the 1 and 3 month visits. However, by 6 months, the likelihood of a subject reporting lower problem or interference levels related to numbness or less lip sensitivity was significantly higher in the sensory-retraining group (Table 6). The odds of reporting lower problem levels or less interference in the sensory retraining group was approximately twice that of the opening-only exercise group.
Figure 4.
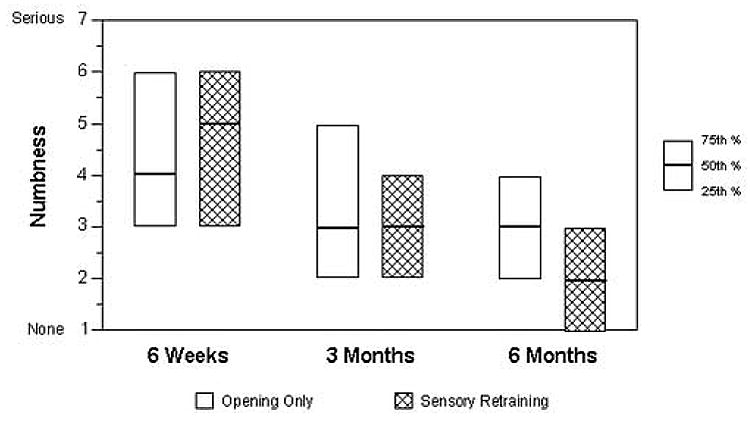
Descriptive Statistics Comparing the Sensory-Retraining and Opening-Only Exercise Groups for the Problem or Interference Level Associated with Numbness over the 6 Month Post-surgical Period
Discussion
The sensory branches of the trigeminal nerve carry information about facial movements, pressures, and expressions to those areas of the cerebral cortex that underlie recognition and discrimination of skin stimuli and determine “how the face feels” (i.e., facial sensibility). Damage to the nerve by any means negatively affects the quality of facial sensibility as well as the patient's ability to translate altered and impoverished patterns of nerve activity into functionally meaningful motor behaviors. (38-42). After healing of damaged tissues, residual altered sensation is predominately associated with nerve injury and resulting changes within the central nervous system.
The emphasis of this paper differs notably from that of previous studies on sensory retraining of the hand after injuries to the median and/or ulnar nerve. With few exceptions, hand studies have concentrated on the return of functional sensation defined by patients' ability to manipulate and identify small objects and to use the hands in skilled purposeful manners. (10-15, 43) Patients' ability to discriminate two from one point of contact, particularly for moving stimuli (viz., the moving two-point discrimination threshold), is often measured as it correlates most highly with patient's ability to use the hand in a dexterous manner (44,45). Overall, sensory recovery is scored by objective testing using a modified Medical Research Council Scale from no recovery (S0) to complete recovery (S4)(17,30). Although this scale incorporates the presence of hyperesthesia or over-responsiveness to tactile stimuli, it does not include patients' subjective reports or assessment of the burden imposed by the altered sensation.
Only rarely have patients' subjective reports been considered of primary interest when evaluating the effectiveness of sensory retraining protocols implemented for injuries of the hand nerves.(43) The present emphasis on patient-reported burden of altered sensation on daily life was motivated in large part by recognition of the different functions of the facial versus digital sensory innervation: The terminal distribution of the inferior alveolar nerve, i.e., the mental nerve, innervates skin functionally more akin to that innervated by the radial nerve than by the median and ulnar nerves of the hand.(46) Both the skin of the back of the hand and of the hairy lower lip / chin of the face deform in response to movements during function, and as such, the evoked neural discharge serves a proprioceptive role as well as conscious awareness of these affectively important areas of the body.(47,48) Neither the back of the hand nor the face in humans assumes explorative and manipulative roles, in contrast to the finger tips and palmer surfaces of the hands. Since initiation of the clinical trial, others have suggested that the goals of orofacial sensory reeducation should include decreased hyperesthesia and decreased subjective differences, such as in numbness, between affected and unaffected skin areas.(17) Perhaps best stated by Callahan, “If sensory reeducation results in a person's increased ability … or to better enjoy the tactile sensations of everyday living, then reeducation has been meaningful and successful.” (15)
Cumulative Burden Score
In previous work we found that difficulty in everyday life imposed by altered sensation was related to the quality of the alteration. For example, unusual feelings were more problematic for subjects reporting dysesthetic sensations than those reporting paresthetic sensations. Paresthetic sensations, in turn, were more problematic than simpler losses in sensation or numbness. (49) It was thought that patients who experience positive (dysesthetic or paresthetic) sensations after healing of the tissues might have a heightened awareness of abnormal and intrusive sensation on the lower lip and chin, eroding their quality of life more severely than simple loss of sensation from the lower face. The cumulative burden score of the present study was constructed to include the patient's perceived difficulty with dysesthetic (painful), paresthetic, and hypoesthetic sensations. However, the recovery trend over the six month period differed substantially for the five questionnaire items, and the reported difficulty with positive (painful) versus negative (numb) altered sensations was affected very differently by sensory retraining indicating that the cumulative burden score was not sufficiently discriminating(Figures 1-5).
Mouth and Face Pain
The present study found no evidence that sensory retraining lessened the unfavorable impact of painful altered sensations on the face or in the mouth (Figures 1 and 2). This is likely related to the low proportion of subjects (∼ 30%) who reported any problem related to pain as early as three months postoperatively and the relatively low incidence of neuropathic complications after orthognathic surgery. (50) Additionally, studies of sensory retraining after injuries to the hand nerves do not report alterations in pain per se because patients who are in pain are generally not candidates for sensory retraining. (51) The skin stimulation required for sensory retraining may be prohibitive in patients with unpleasant hypersensitivities to touch (allodynia, hyperalgesia, hyperpathia).(16,17,51) Behavioral desensitization, pharmacologic therapies, physical therapies, or transcutaneous nerve stimulation may be required before these patients will accept or comply with sensory retraining protocols. On other hand, some forms of vibrotactile stimulation used in sensory retraining may also be used to ‘desensitize’ the skin, (15) and desensitization is often viewed as part of sensory retraining. (15,17,30,43) That is, sensory retraining teaches the patient to ignore or blot out the new, post-injury unpleasant sensations to optimally tune into and decipher the weakened and damaged signals from the tissues.
Unusual Feelings
Sensory retraining tended to lessen the unfavorable impact of unusual feeling. However, the difference between the two groups was not statistically significant at any given postsurgery visit (Table 6). It may be that ‘unusual feelings’ was too broad in context to differentiate clearly between the two groups since dysesthetic, paresthetic and hypoesthetic sensations could all be construed as unusual. The burden these sensations impose on patients' daily life varies with the qualitative nature of the sensations, (49) and the qualitatively different sensations are differentially responsive to sensory retraining. Although the current study did not question subjects specifically about paresthesias, a positive benefit of sensory retraining in reducing paresthesias on the hand has been demonstrated previously. Imai et al. (43) studied patients with injured median nerves (clean cut and repaired), about half of whom received sensory reeducation. Although patients in both groups reported paresthesias, the sensory-retrained group reported less interference with daily life.
Numbness and Less Lip Sensitivity
Sensory retraining significantly lessened the unfavorable impact of hypoesthetic altered sensations and negative symptoms on the face and lips that can be attributed to loss of innervation (Figures 4 and 5). As noted previously, more than two-thirds of all subjects reported difficulty or problems related to numbness at 6 months postsurgery and approximately half of the subjects continued to report problems related to loss of lip sensitivity. The recovery trend for these two items suggests that sensory retraining exercises are most effective on decreasing the perceived burden associated with hypoesthetic altered sensations: The problem levels reported by the sensory-retraining group were slightly higher at 1 month, but lower by 6 months. At 1 month when surgically traumatized tissues were healing, sensory loss was most noticeable. Because the retraining exercises demanded greater attention to the sensory loss and its severity, a transient increase in the burden might be expected over the first months after surgery, followed by the longer term, hypothesized effect of lower burden. Overall, the results from this clinical trial support the premise that a simple noninvasive exercise program initiated shortly after orthognathic surgery can lessen the objectionable impression of negative altered sensations.
Future Directions
The findings of this clinical trial are encouraging and support further investigations and efforts to refine sensory reeducation protocols. Subjects were recruited from both a university-based and a community-based practice and both of the areas served are “Standard Metropolitan Areas”. The subjects enrolled were predominantly female and Caucasians. Although greater ethnic diversity would have been desirable, the enrollment reflects the demographics of the participating practices. The findings of a positive benefit from sensory retraining are limited to healthy individuals whose trauma and nerve injury are from an acute onset and are of a known duration. Whether retraining exercises would be beneficial for patients with trigeminal nerve-injury or could be successfully used as desensitization for neuropathic pain patients is not known. Many questions remain unanswered. Is a reduction in patient-reported burden due to a reduction in the altered sensation, a change in the patient's impression of the alteration, or both? Is there specificity to the sensory retraining exercises: e.g., are other retraining exercises, employing different types of tactile stimuli, equally, or more, effective to the ones used in the clinical trial? How does the retraining effect vary with patient compliance? Can visual, auditory cues and/or mental exercises be incorporated in sensory retraining to improve or speed up the effect? This simple noninvasive exercise program is a largely unexplored avenue of treatment that may help those who suffer from altered facial sensations.
Acknowledgments
As a Phase III clinical trial, a Data Safety and Monitoring Board was required by NIDCR to monitor the project. We wish to thank Dr. John Gregg, chair, Drs Hillary Broder, Tonya King, Eric Rath, Helen Sharp, Christian Stohler, and Michael Terrin for their guidance and support during this project. Special thanks to the study coordinators: Harold Jennings; Atousa Safavi; Colleen Farmer and applications programmer, Debora Price. Special thanks to staff at Oral and Maxillofacial Surgery for their assistance and accommodation of the research protocol within the practice setting. This project was supported in part by NIH grant DE01367.
Appendix
Cumulative Burden Analysis Procedure
The procedure was as follows: 1) within each stratification level, the cumulative burden scores and the presurgery scores were ranked 2) within each stratification level, the ranked cumulative score was regressed via a simple linear regression on the ranked covariate to produce residuals 3) a Mantel-Haenszel stratified linear rank statistic was calculated using SAS's Proc Freq procedure (Stokes, Davis and Koch 2000; chapter 7.7) with number of jaws operated and addition of genioplasty as the stratification variables; exercise group as the row variable and the residuals as the column variables.
Item Specific Analysis Procedure
The model for each item was fit and empirical sandwich standard errors robust to misspecification of the correlation structure were produced using Proc Genmod (SAS/STAT®). Reference cell parameterization was used with the sensory-retraining group and the 6 month visit as the reference levels. In this parameterization, the p-value for the main effect of exercise group was the comparison of the two groups at the 6 month visit. For those items for which the time-by-exercise group interaction was statistically significant, odds ratios and their 95% confidence intervals were computed at each visit for the comparison of exercise groups. The reported cumulative odds ratios indicate the odds of subjects in the sensory-retraining group reporting lower problem levels related to the individual altered sensation and pain items than those in the opening-only exercise group.
Score Statistic P-values for Variable-Added-Last Tests from Individual Item-specific Repeated Measures Analysis based upon Proportional Odds Models Fit with Generalized Estimating Equations
| Altered Sensation | Pain | ||||
|---|---|---|---|---|---|
| Source | Unusual Feelings | Numbness | Less Lip Sensitivity | In Mouth | Facial Regions |
| Exercise Group | 0.52 | 0.02 | 0.03 | 0.07 | 0.88 |
| No. of jaws operated | 0.27 | 0.30 | 0.06 | 0.21 | 0.84 |
| Genioplasty | 0.07 | 0.38 | 0.39 | 0.11 | 0.055 |
| Baseline Value | 0.04 | 0.29 | 0.08 | 0.03 | 0.01 |
| Visit | <.001 | <0.001 | <.001 | <.001 | <.001 |
| Exercise * Visit | 0.004 | 0.04 | 0.04 | 0.24 | 0.82 |
Footnotes
Video tapes demonstrating each exercise at each level (2 exercise programs × 3 levels = 6 tapes) were produced by Video Services of the Center for Instructional Technology at the University of North Carolina. Written instructions provided to subjects and copies of the instructional tapes are available from the corresponding author upon request
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Ceib Phillips, Professor, Department of Orthodontics, University of North Carolina, Chapel Hill, NC 27599.
Greg Essick, Professor, Department of Prosthodontics, University of North Carolina, Chapel Hill, NC 27599.
John S Preisser, Research Associate Professor, Department of Biostatistics, School of Public Health, University of North Carolina, Chapel Hill NC.
Timothy A Turvey, Professor, Department of Oral and Maxillofacial Surgery, University of North Carolina, Chapel Hill, NC 27599.
Myron Tucker, Private Practice, 411 Billingsley Road, Charlotte, NC 28211.
Dongming Lin, MPH Candidate, Department of Biostatistics, University of North Carolina, Chapel Hill, NC 27599.
References
- 1.Marchena JM, Padwa BL, Kaban LB. Sensory abnormalities associated with mandibular fractures: incidence and natural history. J Oral Maxillofac Surg. 1998;56:822. doi: 10.1016/s0278-2391(98)90003-9. [DOI] [PubMed] [Google Scholar]
- 2.Ibizuka T, Lindquist C. Sensory disturbances associated with rigid internal fixation of mandibular fractures. J Oral Maxillofac Surg. 1991;49:1264. doi: 10.1016/0278-2391(91)90301-2. [DOI] [PubMed] [Google Scholar]
- 3.Ellis LG. Altered sensation following mandibular implant surgery: a retrospective study. J Prosthetic Dent. 1992;68:664. doi: 10.1016/0022-3913(92)90384-m. [DOI] [PubMed] [Google Scholar]
- 4.Pogrel MA, Thamby S. The etiology of altered sensation in the inferior alveolar, lingual, and mental nerves as a result of dental treatment. J Calif Dent Assoc. 1999;26:534. [PubMed] [Google Scholar]
- 5.Donoff RB, Colin W. Neurologic complications of oral and maxillofacial surgery. Oral Maxillofac Surg Clin North Am. 1990;2:452. [Google Scholar]
- 6.Phillips C, Essick G, Zuniga J, Tucker M, Blakey GH., III Qualitative Descriptors Used by Patients following Orthognathic Surgery to Portray Altered Sensation. J Oral Maxillofac Surg. 2006a doi: 10.1016/j.joms.2005.11.100. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Westermark A, Bystedt H, von Konow L. Inferior alveolar nerve function after sagittal split osteotomy of the mandible: Correlation with degree of intraoperative nerve encounter and other variables in 496 operations. Br J Oral Maxillofac Surg. 1998;36:429. doi: 10.1016/s0266-4356(98)90458-2. [DOI] [PubMed] [Google Scholar]
- 8.LaBanc JP, Gregg JM. Oral and Maxillofacial Surgery Clinics of North America. Vol. 4. WB Saunders Co; Philadelphia: 1992. Trigeminal Nerve Injury: Diagnosis and Management. [Google Scholar]
- 9.Kaban LB, Pogrel MA, Perrott DH, editors. Complications on Oral and Maxillofacial Surgery. W.B.Saunders; Philadelphia: 1997. [Google Scholar]
- 10.Salter MI. Sensory re-education of the hand. Prog Phys Ther. 1970;1:264. [PubMed] [Google Scholar]
- 11.Wynn Parry CB, Salter M. Sensory re-education after median nerve lesions. Hand. 1976;8:250. doi: 10.1016/0072-968x(76)90010-3. [DOI] [PubMed] [Google Scholar]
- 12.Dellon AL, Curtis RM, Edgerton MT. Reeducation of sensation in the hand after nerve injury and repair. Plast Reconstr Surg. 1974;53:297. doi: 10.1097/00006534-197403000-00008. [DOI] [PubMed] [Google Scholar]
- 13.Dellon AL. Functional sensation and its reeducation. Clin Plast Surg. 1984;11:95. [PubMed] [Google Scholar]
- 14.Dellon AL. Re-education of sensation. In: Dellon AL, editor. Evaluation of sensibility and re-education of sensation in the hand. Baltimore, MD: John D Lucas; 1988. pp. 203–246. [Google Scholar]
- 15.Gregg JM. Nonsurgical management of traumatic trigeminal neuralgias and sensory neuropathies. Atlas Oral Maxillofac Surg Clin North Am. 1992;4:375. [Google Scholar]
- 16.Callahan AD. Methods of compensation and re-education for sensory dysfunction. In: Hunter JM, Mackin EJ, Callahan AD, editors. Rehabilitation of the Hand. St Louis, MO: CV Mosby; 1995. pp. 701–714. [Google Scholar]
- 17.Meyer RA, Rath EM. Sensory rehabilitation after trigeminal nerve injury or nerve repair. Atlas Oral Maxillofac Surg Clin North Am. 2001;13:365. [Google Scholar]
- 18.Forence SL, et al. Sensory enrichment after peripheral nerve injury restores cortical, not thalamic, receptive field organization. Eur J Neurosci. 2001;13:1755. doi: 10.1046/j.0953-816x.2001.01555.x. [DOI] [PubMed] [Google Scholar]
- 19.Lundborg G. Nerve injury and repair – a challenge to the plastic brain. J Peripher Nerv Syst. 2003;8:209. doi: 10.1111/j.1085-9489.2003.03027.x. [DOI] [PubMed] [Google Scholar]
- 20.Johansson BB. Brain plasticity in health and disease. Keio J Med. 2004;53:231. doi: 10.2302/kjm.53.231. [DOI] [PubMed] [Google Scholar]
- 21.Nishioka GJ, Zysset MK, Van Sickels JE. Neurosensory disturbance with rigid fixation of the bilateral sagittal split osteotomy. J Oral Maxillofac Surg. 1987;45:20. doi: 10.1016/0278-2391(87)90081-4. [DOI] [PubMed] [Google Scholar]
- 22.Posnick JC, Al-Quattan MM, Stepner NM. Alteration in facial sensibility in adolescents following sagittal split and chin osteotomies of the mandible. Plast Reconstr Surg. 1996;97:920. doi: 10.1097/00006534-199604001-00006. [DOI] [PubMed] [Google Scholar]
- 23.Essick GK, Austin S, Phillips C, Kiyak HA. Short-term sensory impairment after orthognathic surgery. Oral Maxillofac Surg Clin North Am. 2001;13:295. [Google Scholar]
- 24.SAS/STAT® 9.1 User's Guide. Cary, NC: SAS institute. Inc; 2004. [Google Scholar]
- 25.Yoshida T, et al. Impairment of the inferior alveolar nerve after sagittal split osteotomy. J Craniomaxillofac Surg. 1989;17:271. doi: 10.1016/s1010-5182(89)80095-2. [DOI] [PubMed] [Google Scholar]
- 26.Karas ND, Boyd SB, Sinn DP. Recovery of neurosensory function following orthognathic surgery. J Oral Maxillofac Surg. 1990;48:124. doi: 10.1016/s0278-2391(10)80199-5. [DOI] [PubMed] [Google Scholar]
- 27.Van Boven RW, Johnson KO. A psychophysical study of the mechanisms of sensory recovery following nerve injury in humans. Brain. 1994;117:149. doi: 10.1093/brain/117.1.149. [DOI] [PubMed] [Google Scholar]
- 28.Fridrich KL, Holton TJ, Pansegrau KJ, Buckley MJ. Neurosensory recovery following the mandibular bilateral sagittal split osteotomy. J Oral Maxillofac Surg. 1995;53:1300. doi: 10.1016/0278-2391(95)90588-x. [DOI] [PubMed] [Google Scholar]
- 29.Daniele HR, Aguado L. Early compensatory sensory re-education. J Reconstr Microsurg. 2003;19:107. doi: 10.1055/s-2003-37815. [DOI] [PubMed] [Google Scholar]
- 30.Waylett-Rendall J. Sensibility evaluation and rehabilitation. Orthop Clin North Am. 1988;19:43. [PubMed] [Google Scholar]
- 31.Phillips C, Bennett E. Psychological Ramifications of Orthognathic Surgery. In: Fonseca R, editor. Oral and Maxillofacial Surgery. Vol. 2. WB Saunders; Philadelphia: 2000. pp. 506–534. [Google Scholar]
- 32.Muller KE, Barton CN. Approximate power for repeated measures ANOVA lacking sphericity. J Am Stat Assoc. 1989;84:549. [Google Scholar]
- 33.Elashoff JD. nQuery Advisor® Version 4.0 User's Guide. Los Angeles, CA: 2000. [Google Scholar]
- 34.Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2. Lawrence Erlbaum Assoc; Hillsdale, NJ: 1988. [Google Scholar]
- 35.Preisser JS, Koch GG. Categorical data analysis in public health. Annu Rev Public Health. 1997;18:51. doi: 10.1146/annurev.publhealth.18.1.51. [DOI] [PubMed] [Google Scholar]
- 36.Lipsitz, Kim, Zhao L. Analysis of repeated categorical data using generalized estimating equations. Stat Med. 1994;15:1149. doi: 10.1002/sim.4780131106. [DOI] [PubMed] [Google Scholar]
- 37.Stokes ME, Davis CS, Koch GG. Categorical data analysis using the SAS® system. 2. Cary, NC: SAS Institute Inc; 2000. [Google Scholar]
- 38.Putnam AHB, Ringel RL. Some observations of articulation during labial sensory deprivation. J Speech Hear Res. 1972;15:529. doi: 10.1044/jshr.1503.529. [DOI] [PubMed] [Google Scholar]
- 39.Stranc MF, Fogel ML. Lip function: A study of oral continence. Brit J Plast Surg. 1984;37:550. doi: 10.1016/0007-1226(84)90148-6. [DOI] [PubMed] [Google Scholar]
- 40.Sandstedt P, Sorensen S. Neurosensory disturbances of the trigeminal nerve: A long-term follow-up of traumatic injuries. J Oral Maxillofac Surg. 1995;53:498. doi: 10.1016/0278-2391(95)90055-1. [DOI] [PubMed] [Google Scholar]
- 41.Lemke RR, et al. Effects of hypesthesia on oral behaviors of the orthognathic surgery patient. J Oral Maxillofac Surg. 1998;56:153. doi: 10.1016/s0278-2391(98)90856-4. [DOI] [PubMed] [Google Scholar]
- 42.Essick GK. Invited Discussion of: Effects of hypesthesia on oral behaviors of the orthognathic surgery patient. J Oral Maxillofac Surg. 1998;56:158. doi: 10.1016/s0278-2391(98)90856-4. (Lemke RR, Clark GM, Bays RA, Tiner BD, Rugh JD) [DOI] [PubMed] [Google Scholar]
- 43.Imai H, Tajima T, Natsumi Y. Successful reeducation of functional sensibility after median nerve repair at the wrist. J Hand Surg. 1991;16A:60. doi: 10.1016/s0363-5023(10)80014-0. [DOI] [PubMed] [Google Scholar]
- 44.Dellon AL. The moving two-point discrimination test: clinical evaluation of the quickly adapting fiber/receptor system. J Hand Surg. 1978;3:474. doi: 10.1016/s0363-5023(78)80143-9. [DOI] [PubMed] [Google Scholar]
- 45.Dellon AL, Kallman CH. Evaluation of functional sensation in the hand. J Hand Surg. 1983;8:865. doi: 10.1016/s0363-5023(83)80083-5. [DOI] [PubMed] [Google Scholar]
- 46.Trulsson M, Essick GK. Low-threshold mechanoreceptive afferents in the human lingual nerve. J Neurophysiol. 1997;77:737. doi: 10.1152/jn.1997.77.2.737. [DOI] [PubMed] [Google Scholar]
- 47.Edin BB, Johansson N. Skin strain patterns provide kinaesthetic information to the human central nervous system. J Physiol. 1995;1:243. doi: 10.1113/jphysiol.1995.sp020875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Gandevia SC, Phegan CML. Perceptual distortions of the human body image produced by local anaesthesia, pain and cutaneous stimulation. J Physiol. 1999;2:609. doi: 10.1111/j.1469-7793.1999.609ae.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Phillips C, Essick G, Blakey GH, III, Tucker M. Relationship between Perception of Post-surgical Sequelae and Qualitative Descriptors of Altered Sensation following BSSO. J Oral Maxillofac Surg. 2006 b doi: 10.1016/j.joms.2005.11.100. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Essick GK. Psychophysical assessment of patients with posttraumatic neuropathic trigeminal pain. J Orofac Pain. 2004;18:345–354. [PubMed] [Google Scholar]
- 51.Mackinnon SE, Dellon AL. Surgery of the peripheral nerve. New York: Thieme; 1988. pp. 531–532. [Google Scholar]


