Abstract
The purpose of this study was to evaluate the efficacy of two brief interventions and the inclusion of a 1-month booster session with college students who were referred to attend alcohol education following an alcohol-related incident. Participants (N=225; 48.9% male) were randomly assigned to receive one session of a Brief Motivational Interview (BMI) or computer-delivered intervention (CDI) with the Alcohol 101 CD-ROM. Participants were also randomly assigned to booster/no booster. At 3-month follow up participants in BMI reported greater help seeking and use of behavioral strategies to moderate drinking. At 12-month follow up, BMI participants were drinking more frequently and CDI participants were consuming a greater number of drinks per occasion than at baseline. Mediation analyses showed that the use of specific behavioral strategies fully mediated the effect of the BMI condition on drinking volume. There was no intervention effect on alcohol problems and the booster condition did not significantly affect outcomes. Promoting specific behaviors in the context of in-person brief interventions may be a promising approach to reducing drinking volume among identified at-risk students.
1. Introduction
Heavy drinking peaks during late adolescence and early adulthood and is especially common among 18 – 24 year-old young adults who attend college (Chen, Dufour, & Yi, 2004/2005). These patterns of heavy drinking place college students at high risk for alcohol-related health and social problems, including extreme intoxication and college disciplinary infractions. Alcohol intoxication and related behaviors are the most common reasons for cases of emergency medical care and campus discipline (Stone & Lucas, 1994; Wright & Slovis, 1996), and arrests and violations of campus alcohol and drug policies have been increasing over the past decade (The National Center on Addiction and Substance Abuse, 2007; Porter, 2006).
1.1. Interventions for College Student Problem Drinking
1.1.1. Counselor delivered brief motivational interventions
College student drinkers generally report mild to moderate drinking problems and little motivation to change their drinking, and therefore they are an ideal population to target with brief motivational interventions (BMIs; Larimer, Cronce, Lee, & Kilmer, 2004/2005). BMIs typically incorporate the principles and methods of Motivational Interviewing (MI; Miller & Rollnick, 2002), a supportive and nonjudgmental therapeutic approach that is specifically designed to work through the ambivalence that often accompanies health behavior change. BMIs provide an opportunity for students to discuss their alcohol use and their interest in moderating consumption and avoiding related high-risk behaviors. BMIs typically include personalized normative feedback (PNF), advice, and behavioral strategies for avoiding alcohol-related harm. PNF usually includes information contrasting the student’s drinking with drinking patterns of other college students, an approach intended to correct overestimation of peer drinking (Neighbors, Larimer, & Lewis, 2004). BMIs with college students have strong empirical support relative to no-treatment control conditions and relative to interventions that provide generic information about alcohol (Marlatt et al., 1998; Murphy et al., 2001).
1.1.2. Computerized interventions
Computer or internet-based alcohol education programs are rapidly being adopted on college campuses (Walters, Miller, & Chiauzzi, 2005). Stand-alone programs and internet sites are increasingly being used for universal prevention for incoming freshmen, and as a requirement for alcohol-related judicial cases. Preliminary studies have been conducted with an interactive CD-ROM program (Alcohol 101; Century Council, 1998) that takes participants through a “virtual party”. Reis, Riley, Lokman, and Baer (2000) compared Alcohol 101 to an educational class and a no-intervention group. Students in the Alcohol 101 condition reported greater knowledge about alcohol and how to protect themselves and their friends relative to the other conditions, but no behavioral outcomes were reported. Sharmer (2001) evaluated Alcohol 101 in a classroom setting with a general sample of undergraduates. The Alcohol 101 condition included an instructor guide and was compared to a motivational speaker and to a no-intervention control group; no group differences in alcohol use were found at 1-, 2-, and 3- month follow ups. Donohue, Allen, Maurer, Ozols, & DeStefano (2004) compared Alcohol 101 to Cognitive Behavior Therapy in college students who reported consuming at least one drink in the past month and found no group differences in alcohol consumption at 1-month follow up. To date no studies have been conducted with students screened for risk, although the most common use of the program has been for disciplinary sanctions (Anderson & Cohen, 2001) and the program is distributed to over 1,200 colleges (Century Council, 2003).1
1.1.3. Intervention with mandated students
Most colleges have required programs for students who receive medical treatment for intoxication or who receive an alcohol-related infraction (Anderson & Gadaleto, 2001). Typical approaches include disciplinary sanctions, citations, fines, mandatory educational programs and counseling. A few studies show the promise of motivationally focused group counseling relative to control and comparison conditions (Fromme & Corbin, 2004; LaChance, 2004). Counselor-delivered BMI also has shown promise with mandated students; Borsari and Carey (2005) compared a BMI session to an individual alcohol education session among mandated students who reported recent heavy drinking or alcohol problems. BMI participants showed a significantly greater reduction in alcohol problems at 3 and 6 month follow up. However, White et al. (2006) found no differences in consumption or alcohol problems between a counselor-delivered BMI vs. PNF-only with mandated students at 3-month follow up. In sum, recent evidence indicates that counselor-delivered interventions may be effective among heavy drinking mandated students, but alternative conditions have also shown promise.
Promoting help seeking is a goal of brief alcohol intervention (Heather, 1995), is important in the recovery from serious alcohol problems (Dawson, Grant, Stinson, & Chou, 2006), and may be especially important with college students, as problem recognition tends to be low (Caldwell, 2002) and few voluntarily seek help on campus (Colby, Raymond, & Colby, 2000). Receiving additional counseling beyond any university mandate may be of particular importance for students who have been identified by their university as having had a recent alcohol-related incident, as they show greater evidence of risk than other students (Black & Wood, under review; Caldwell, 2002; Flynn & Brown, 1991; Fromme & Corbin, 2004; Labrie, Tawalbeh, & Earleywine, 2006). There is evidence that MI promotes engagement in treatment (Brown & Miller, 1993; Connors, Walitzer, & Dermen, 2002), and one study of college students found that those with more alcohol education experiences reported they were more likely to seek treatment if in need (Yu, Evans, & Perfetti, 2003). However, help seeking as an outcome of BMI effects has not well evaluated in research with at-risk college students.
1.2. Efficacy of booster sessions
Although some research with adult problem drinkers suggests that additional contact improves brief intervention outcomes (Longabaugh et al., 2001), and such contact is recommended by clinical guidelines (USDHHS, 1993), other findings are contradictory (WHO Brief Intervention Study Group, 1996). Moreover, studies with college student volunteers have not found an advantage for multiple-session interventions (Baer et al., 1992), but none have manipulated the amount of additional contact with mandated students who might benefit from additional opportunity to discuss and/or reflect on their behavior.
1.3. Mediators of intervention efficacy
Investigating the underlying processes of behavior change is critical for the advancement of intervention research (Kazdin & Nock, 2003; Longabaugh et al., 2005). Few studies of BMI with college students have evaluated putative mechanisms of intervention effects and very few have determined significant mediators of the effects of BMI. Several possible mediators are supported by theories of behavior change. Motivation for change is a presumed target of BMIs (Miller & Rollnick, 2002). There is evidence that motivation to change is low among mandated students (Caldwell, 2002), that higher motivation predicts greater drinking reductions following BMI with voluntary students (Fromme & Corbin, 2004), and that motivation increases following intervention with mandated students (Palmer, 2004). However, no studies with mandated college students have evaluated motivation as a mediator of BMI.
Providing information about harm reduction strategies is a common approach of intervention approaches with college students (Dimeff et al., 1999; Walters & Baer, 2006). These strategies typically include modifying behavior to change the way an individual drinks (e.g., setting a drinking limit or alternating nonalcoholic drinks). Several studies have found that the more frequently students used protective strategies, the less likely they were to report alcohol-related harm (Benton et al., 2004; Haines, Barker & Rice, 2006; Martens et al., 2004). Martens et al. (2004) recommended assessing the use of protective behavioral strategies and incorporating them into personalized feedback, and one recent study found the use of such strategies mediated the efficacy of a mailed personalized feedback (Larimer et al., 2007). However, this intervention component has not been evaluated in the context of an in-person BMI as an outcome or mediator.
Normative feedback alone can reduce alcohol use among college students relative to no treatment (Neighbors et al., 2004) and comparison groups (McNally & Palfai, 2003). Other studies have found change in perceptions of peer drinking to mediate reductions in alcohol use (Borsari & Carey, 2000; Walters, Vader, & Harris, 2006), but this promising mechanism has not been evaluated with mandated students.
1.4. Study purpose
This trial evaluated the efficacy of a counselor-delivered BMI versus computer-delivered intervention (CDI; Alcohol 101) with students mandated to intervention.2 The efficacy of BMI with high-risk and mandated college students is stronger than the efficacy evidence for the Alcohol 101 program and therefore we hypothesized that BMI would be more efficacious in reducing alcohol use and problems than CDI. We also expected that the booster session would enhance intervention effects. We explored motivation to change, normative perceptions, and use of protective behavioral strategies as mediators of effects on drinking outcomes. The trial was designed to evaluate long-term follow up and recidivism.
2. Method
2.1. Participants
Participants were students at a private university in New England who were required to attend a session of health education following medical evaluation for intoxication or a disciplinary hearing for an alcohol-related violation. Participation was a voluntary alternative to having an individual session with a university health educator. Seniors were excluded because they would graduate during the 12-month follow-up period. From September, 2000 through May, 2004, 348 students were eligible and 227 (65%) agreed to participate (Figure 1).
Figure 1.
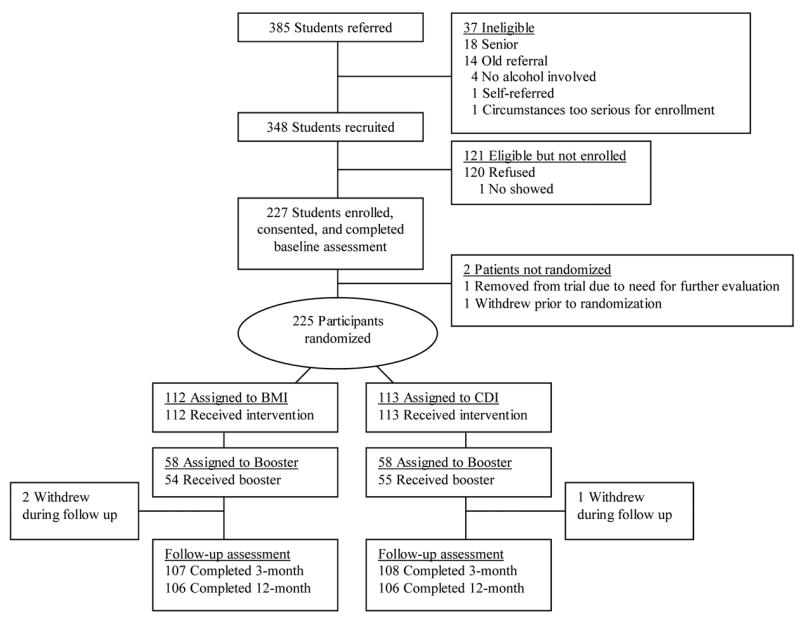
Flow chart of patient eligibility, enrollment, and participation.
2.2. Procedures
All procedures were approved by the University Institutional Review Board. During the baseline session with a research counselor, information was collected about the alcohol-related event that precipitated the referral. Participants then completed a packet of questionnaires. At the end of the session the counselor opened an envelope containing the baseline condition assignment, prepared by the project coordinator according to a random numbers table. Participants returned for interventions in approximately one week.
2.2.1. Staff training and supervision
Counselors were eight master’s or Ph.D. level practitioners. Research assistants who conducted the follow-up sessions were four bachelor’s level staff. Counselors received 30 hours of training in MI, and were supervised weekly by NB or JM. Audiotapes of BMI sessions were reviewed regularly.
2.2.2. Intervention conditions
Interventions were conducted in a private office by the same counselor who had completed the baseline assessment. Following the interventions, participants completed a measure of motivation to change. Information sheets about follow-up and handouts about alcohol and college life were given to all participants.
2.2.3. Brief Motivational Intervention condition
The BMI consisted of four major parts: introduction and review of the alcohol event, assessing motivation, enhancing motivation, and establishing goals. The introduction consisted of explaining what the session would entail, reminding participants about confidentiality and its limits, and explaining that the counselor would not be telling them what to do about their alcohol use. Counselors briefly reviewed the participant’s event as a starting point for the subsequent discussion. Assessing motivation involved an exploration of the positive and negative aspects of drinking for participants, and parents’ and friends’ attitudes about drinking in order to identify important social influences.
Enhancing motivation consisted of providing personalized feedback and encouraging participants to envision their future. Feedback reports included: 1) a summary of drinking and consequences experienced in the event; 2) a comparison of the participant’s alcohol use vs. age- and gender-based national norms; 3) estimated past-month average and peak blood alcohol concentration (BAC) and the effects of different BAC levels; 4) alcohol-related consequences; and 5) participant risks, including interpretation of the AUDIT score and alcohol-related sex risks. Counselors facilitated discussion about the feedback, and asked participants to consider the outcomes if they decided to make a change and if they decided not to. The final pages of the feedback report indicated whether participants had sought help for their drinking and listed strategies for reducing alcohol use, personalized to identify strategies participants had reported previously using. For participants who were interested in discussing goals for change, the counselors reviewed which strategies had been helpful and discussed alternatives. Throughout the session, counselors used MI principles and methods (Miller & Rollnick, 2002).
2.2.4. Computer-Delivered Intervention condition
The CDI condition consisted of an individual session with Alcohol 101 (Century Council, 1998). This program features a “virtual party” that has a number of different “rooms”, starting with a virtual bar in which participants can observe the effects of gender, weight, drink type, and speed of consumption on BAC. Other components include video testimonies about alcohol-related consequences, video clips of various drinking scenarios, and multiple-choice questions about alcohol and its effects. The program also provides personalized normative feedback about participants’ drinking pattern and perception of peer drinking (derived from questions asked at the beginning of the Alcohol 101 program).
Participants received instructions on the use of the program, and sat at a desktop computer with headphones. Participants were required to spend 45 minutes using the program. At the end of the session the counselor used a feature of the program to record the components the participant had seen (to be used for those assigned to booster). Participants next completed post-session measures and received project handouts.
2.2.5. Booster condition
At the end of the intervention session the counselor opened an envelope containing the participant’s randomly assigned booster condition. Boosters were conducted one month after baseline. The BMI booster was a 25-minute session conducted by the same counselor as baseline, and consisted of a review of the baseline session and discussion of what had occurred since that session. Progress toward goals was discussed, and according to the interest of the participant, new goals were set. CDI booster participants used the Alcohol 101 program for 25 minutes after being given a list of the elements they had already seen and being shown how to locate other elements.
2.2.6. Follow-up assessments
A research assistant who was blind to intervention condition conducted the 3-and 12-month follow-up assessments in person, or by phone and mail for those due during a school break (22% of follow-up assessments). As at baseline, the sessions consisted of interviewer-administered and self-administered measures. Participants were paid $25 and $30 for the 3 and 12 month follow-ups, respectively, and a $40 bonus if both follow-ups were completed within two weeks of their due dates.
2.3. Measures
2.3.1. Internal validity
Adherence to the BMI protocol was measured by ratings of session audiotapes. Two independent raters (one masters, one doctoral level, both with clinical experience) rated 20% of each counselor’s BMI session tapes. Adherence was evaluated by measuring the degree to which each of 12 session components (e.g., reference event, pros/cons, provide feedback) was administered. This measure, modified from earlier work (Barnett, Monti, & Wood, 2001), has a scale of 1 (below expectations; not administered or administered poorly), 2 (meets expectations; administered adequately), or 3 (above expectations; administered particularly well). Although a written protocol of the session was used by counselors, we did not expect every component to be administered by every counselor. Consistent with MI style, they were trained to use their clinical judgment about the direction the session took. Nevertheless, we did expect that the majority of intervention components would be addressed, for consistency across cases. Clinical competence in eight MI principles and methods (e.g., develop discrepancy, roll with resistance) was rated on the same 3-point scale. We expected that for both adherence and competence the average score for each element would be 2 or higher. In addition, the two global scores Empathy and MI Spirit from the Motivational Interviewing Treatment Integrity coding system (MITI; Moyers, Martin, Manuel, Hendrickson, & Miller, 2005a), were rated using a 1 (low) to 7 (high) scale. A score of 6 or higher reflects clinician competency (Moyers, Martin, Manuel, & Miller, 2004b).
2.3.2. Demographics, incident characteristics, and alcohol problem screen
Age, race, year in school, and self-reported weight were collected at baseline. The nature of the incident, number of standard drinks (12 oz. beer, 1.25 oz. liquor, 4 oz. wine) and length of time spent drinking were recorded for purposes of estimating BAC (Alco-Calculator, 1983). The Alcohol Use Disorders Identification Test (AUDIT), a 10-item screening measure for hazardous alcohol use (Saunders et al., 1993), was administered for the BMI feedback.
2.3.3. Outcome measures
Alcohol use was measured with an interviewer-administered Timeline Followback (TLFB; Sobell & Sobell, 1995) calendar. At baseline, data were collected for 30 days prior to the drinking incident; at follow-up data were collected for the past 30 days. For each day, number of standard drinks and the length of time spent drinking were recorded. Computed variables were number of drinking days, number of heavy drinking days (5 or more drinks for males, 4 or more drinks for females), average number of drinks per drinking day, and average BAC. The Young Adult Alcohol Problems Screening Test (YAAPST; Hurlbut & Sher, 1992) is a 27-item measure that assesses past-year alcohol problems. Items were dichotomized and summed for a total score (α= .78). The timeframe was adjusted to 3 months at the follow-ups. Help seeking for alcohol-related issues was measured with five items about whether the participant had received individual, group, family or residential counseling, or had been to a 12-step meeting for drinking. Based on response distributions (a high proportion of 0 scores), items were converted to a dichotomous indicator of any help seeking during each time period. To measure recidivism, participants reported any alcohol-related violations or medical treatment for alcohol use at follow ups; University records also were reviewed for these outcomes.
2.3.4. Process variables
Motivation to change alcohol use was measured with the Contemplation Ladder (Becker et al., 1996) which was administered pre- and post-intervention. This instrument contains an image of a ladder in which each rung represents a level of motivation. Response options range from 0 (no thought of changing) to 10 (taking action to change [e.g., cutting down]). Perception of peer drinking was measured with an item from the Drinking Norms Rating Form (Baer et al., 1991) that assessed the participant’s perception of how much an average university student of the same sex drinks on one day on a scale of 1 (0 drinks) to 6 (more than 8 drinks). Behavioral strategies for limiting drinking were measured with 22 items from the Self Control Questionnaire (SCQ; Werch & Gorman, 1986), which queries participants about how frequently they use specific strategies to deliberately limit drinking. These items were included on the strategies list provided in the BMI condition. Examples of items are “Set the number of drinks you will have ahead of time” and “Drink nonalcoholic beverages between alcoholic drinks.” Scores of 1 (never) to 5 (always) were summed for a total score with internal consistency of α =.89.
2.4. Data Analysis
T-tests and repeated measures analysis of variance (ANOVA) and analysis of covariance (ANCOVA) were used for continuous outcomes. Two separate analyses were conducted for each outcome (3 months and 12 months). Chi-square analyses were used for dichotomous outcomes. Multiple regression was used to investigate mediators of intervention effects.
3. Results
3.1. Sample Description and Baseline Comparison of Conditions
There were no significant gender or class year differences between participants and students who declined to participate. Demographic and incident information for participants is presented in Table 1. Of the 225 participants, 112 were assigned to BMI, 113 were assigned to CDI, and 116 (51.6%) were assigned to the booster condition (58 each in BMI and CDI). There were no differences between baseline conditions or between booster conditions on demographics, type of referral, motivation, alcohol consumption or alcohol problems.
Table 1.
Description of participants
| Measure | M (SD) or % |
|---|---|
| Male | 110 (48.9%) |
| Age | 18.8 (0.87) |
| School Year | |
| Freshmen | 150 (66.7%) |
| Sophomores | 45 (20.0%) |
| Juniors | 30 (13.3%) |
| Racea | |
| White | 170 (75.6%) |
| Asian | 34 (15.1%) |
| Hispanic | 29 (12.9%) |
| Black | 8 (3.6%) |
| Native American | 5 (2.2%) |
| Other | 6 (2.7%) |
| Reason for referral | |
| Medical evaluation | 185 (82.2%) |
| Disciplinary infraction | 28 (12.4%) |
| Both | 12 (5.3%) |
| Drinks prior to incident | 8.9 (5.5) |
| Incident estimated BAC | .245 (.140) |
Proportions do not equal 100% because 25 participants (10.0%) reported more than one category.
3.2. Booster and Follow-up Completion
Of participants assigned to booster, 94.0% were completed, with no differences in completion rates by condition. There were no baseline differences in alcohol consumption or in alcohol problems between those who completed boosters and those who did not. Follow-up rates for the 3- and 12-month follow-ups were 94.7% and 95.1%, respectively, with no differences in rates between intervention or booster conditions. There were no demographic, alcohol consumption or alcohol problems differences between completers and non-completers.
3.3. Evaluation of Internal Validity
Complete audiotapes of 93 BMI sessions (83.0%) were available, and 20% (n = 19; 17% of BMI sessions) of each counselor’s tapes were randomly selected and reviewed. For adherence items, intraclass correlations (ICCs) were .58 to .93, indicating good to excellent interrater agreement. The average rating for the main components of the protocol was 2.04 (SD = 0.22; Median = 2.08), with 75% – 100% of expected components being administered, indicating that essential components were administered consistently. MI competence items are presented in Table 2. ICCs for these items were .55 to .88. All but one of these components had an average of 2.0 or higher, and the average values for the MITI global scores were greater than 6, an established level of competence (Moyers et al., 2005a). Intervention administration was consistent with our expectations, in that the vast majority of interventions were conducted at or above our standards.
Table 2.
Rater scores for Motivational Interview principles and methods
| Item | (N = 19) M (SD) |
|---|---|
| Competence Ratings | |
| Develop discrepancy | 2.05 (0.23) |
| Roll with resistance | 2.16 (0.38) |
| Support self-efficacy | 2.00 (0.49) |
| Open-ended questions | 2.16 (0.38) |
| Reflective listening | 2.11 (0.46) |
| Affirm | 2.22 (0.55) |
| Summarize | 1.63 (0.50) |
| Elicit change talk | 2.21 (0.42) |
| MITI Global Scores | |
| (MITI) Empathy | 6.05 (0.78) |
| (MITI) MI Spirit | 6.05 (0.62) |
Note: Competence ratings were answered on a 3-point scale: 1 “below expectations”, 2 “meets expectations”, 3 “above expectations”. MITI global items were answered on a 7-point scale from 1 “low” to 7 “high”. Two cases had more than one component that received a “1” (these cases had two components that received a “1”). The median score was 2.0 for every component, including the summary component.
3.4. Outcomes for Alcohol Use and Related Problems
3.4.1. Alcohol use
Baseline and follow-up data are presented in Table 3. Separate 2 (intervention condition) X 2 (booster condition) X 2 (time) ANOVAs were conducted on number of drinking days, number of heavy drinking days, drinks per drinking day, and estimated average BAC for the two follow-up time points. For number of drinking days, a significant main effect of time at the 3-month follow up indicated a significant overall reduction in number of days of past month drinking reported across conditions from baseline to 3 months. At the 12-month follow up a significant intervention condition by time interaction was found. Follow-up simple effects tests indicate that participants in the BMI condition significantly increased number of drinking days from baseline to 12 months, F(1,209) = 9.01, p < .01 (Within-groups [WG] effect size [Cohen’s d] = .23), whereas CDI participants did not change over time. The main effect of booster condition, the 2-way interactions with booster, and the 3-way interaction were not significant. For number of heavy drinking days in the past month, a significant main effect of time from baseline to 3 months was found, which reflected a reduction in heavy drinking days across both groups. No other main effects or interactions were significant at either 3 or 12 months. For average number of drinks per drinking day, a significant intervention condition by time effect was found at 12 months. Follow-up tests show that participants in the CDI condition significantly increased their number of drinks per drinking day, F(1,187) = 4.02, p < .05, (WG effect size [Cohen’s d] = .18) while participants in the BMI condition did not change significantly over time. No other effects were significant. For average BAC, there was a borderline significant condition by time effect that favored the BMI group. No main effects or other interactions were significant.
Table 3.
Alcohol consumption and alcohol problem outcomes in intervention and booster conditions at 3- and 12-month follow up
| Measure | BMI (N = 112) M (SD) | CDI (N = 113) M (SD) | BST (N = 116) M (SD) | No BST (N = 109) M (SD) | df | F (Time) | F (Interv. x Time) | F (BST x Time) |
|---|---|---|---|---|---|---|---|---|
| No. drinking days | ||||||||
| Baseline | 5.23 (4.82) | 6.05 (5.14) | 5.60 (5.27) | 5.69 (4.70) | ||||
| 3 mo. follow up | 4.74 (3.83) | 4.75 (4.37) | 4.75 (4.37) | 4.65 (3.99) | 1,205 | 5.42* | 1.34 | 0.19 |
| 12 mo. follow up | 6.37 (4.67) | 5.89 (4.01) | 5.89 (4.01) | 6.05 (4.18) | 1,207 | 4.23* | 4.67* | 0.73 |
| No. heavy drinking days | ||||||||
| Baseline | 2.77 (3.55) | 3.17 (4.05) | 3.05 (4.05) | 2.88 (3.55) | ||||
| 3 mo. follow up | 2.41 (2.84) | 2.08 (2.61) | 2.56 (3.26) | 1.89 (1.94) | 1,205 | 10.26** | 2.67 | 1.14 |
| 12 mo. follow up | 3.21 (3.91) | 2.95 (3.56) | 3.24 (4.02) | 2.92 (3.43) | 1,207 | 0.38 | 1.67 | 0.63 |
| Ave. no. drinks per drinking day | ||||||||
| Baseline | 4.92 (2.53) | 4.45 (2.36) | 4.90 (2.87) | 4.45 (1.89) | ||||
| 3 mo. follow up | 4.77 (2.89) | 4.49 (2.41) | 4.87 (2.89) | 4.37 (2.39) | 1,173 | 1.56 | 0.58 | 0.24 |
| 12 mo. follow up | 4.64 (2.78) | 4.87 (2.86) | 4.84 (3.07) | 4.66 (2.53) | 1,185 | 0.64 | 4.52* | 1.26 |
| Ave. estimated BAC | ||||||||
| Baseline | .097 (.06) | .088 (.06) | .096 (.06) | .089 (.05) | ||||
| 3 mo. follow up | .085 (.06) | .092 (.06) | .095 (.06) | .091 (.06) | 1,143 | 0.35 | 3.20† | 0.18 |
| 12 mo. follow up | .083 (.05) | .089 (.06) | .091 (.06) | .085 (.06) | 1,154 | 0.98 | 3.40† | 0.67 |
|
| ||||||||
| F (Interv) | F (BST) | |||||||
|
| ||||||||
| Alcohol problems | ||||||||
| 3 mo. follow up | 3.42 (3.03) | 3.03 (2.58) | 3.37 (3.09) | 3.09 (2.52) | 1,194 | 0.17 | 0.61 | |
| 12 mo. follow up | 2.98 (2.59) | 3.17 (3.05) | 3.05 (3.01) | 3.11 (2.63) | 1,204 | 1.84 | 0.22 | |
|
| ||||||||
| N (%) | N(%) | N(%) | N(%) | χ2(Interv) | χ2(BST) | |||
|
| ||||||||
| Help seeking | ||||||||
| 3 mo. follow up | 10 (9.7%) | 3 (2.9%) | 8 (7.5%) | 5 (5.0%) | 1 | 4.09* | 0.59 | |
| 12 mo. follow up | 7 (6.6%) | 7 (6.7%) | 6 (5.7%) | 8 (7.6%) | 1 | 0.00 | 0.31 | |
Note. BMI = Brief Motivational Intervention; CDI = Computer-Delivered Intervention; BST = Booster; BAC = Blood Alcohol Concentration; YAAPST = Young Adult Alcohol Problems Screening Test. On the alcohol consumption measures three participants had missing data at baseline. N’s are slightly different between follow-ups and between measures, due to missing data on self-administered measures. The alcohol consumption measures reflect the past month; alcohol problems and help seeking reflect the past 3 months. Repeated measures analyses conducted with the consumption variables compared follow-up to baseline.
p<.08.
p<.05.
p < .01.
p < .001
3.4.2. Alcohol problems
A 2 (intervention) X 2 (booster) ANCOVA was conducted on the 3- and 12-month YAAPST total score with the baseline score as the covariate. No main or interaction effects of intervention or booster were detected (Table 3).
3.4.3. Help seeking for alcohol issues
At the 3-month follow up 13 participants reported having sought help for alcohol since baseline; 14 participants reported seeking help between 3- and 12-month follow up (see Table 3). Chi-square analyses revealed a significant effect of BMI on help seeking at 3 months (Between-groups effect size = .28), but no group differences at 12 months. No main effect or interactions with booster were found.
3.4.4. Recidivism
In the year following the intervention, 32 subsequent incidents were identified by self-report, and 3 more by records only, for a total of 35 (15.8%); 18 (16.2%) participants in BMI and 17 (15.5%) in CDI. Rates of recidivism were not significantly different between intervention χ2(1, N = 221) = .024, ns, or booster (16 in booster, 19 in no booster), χ2(1, N = 221) = .41, ns.
3.5. Process Outcomes
3.5.1. Motivation to change alcohol use
Pre- and post-intervention scores on the contemplation ladder were evaluated in a 2 X 2 (intervention by time) ANOVA (Table 4). There was a main effect of time, with an increase in motivation from pre-to post-intervention, but no interaction of intervention condition with time.
Table 4.
Effect of intervention and booster condition on process variables
| Measure | BMI (N = 111) M (SD) | CDI (N = 111) M (SD) | BST (N = 114) M (SD) | No BST (N = 108) M (SD) | df | F (Time) | F (Interv. x Time) | F (BST x Time) |
|---|---|---|---|---|---|---|---|---|
| Motivation | ||||||||
| Baseline | 5.25 (3.40) | 5.51 (3.44) | -- | -- | ||||
| Post-intervention | 5.82 (3.67) | 5.90 (3.32) | -- | -- | 1,182 | 4.93* | 0.16 | -- |
| Perception of peer drinking | ||||||||
| Baseline | 3.15 (0.79) | 3.20 (0.78) | 3.16 (0.76) | 3.19 (0.76) | ||||
| 3 mo. follow up | 2.96 (0.71) | 3.00 (0.80) | 3.02 (0.74) | 2.94 (0.77) | 1,202 | 9.48** | 0.05 | 0.69 |
| 12 mo. follow up | 2.86 (0.68) | 3.12 (0.82) | 2.99 (0.78) | 2.99 (0.75) | 1,206 | 7.95** | 3.25† | 0.21 |
| Behavioral strategies | ||||||||
| Baseline | 61.20 (12.88) | 64.43 (14.42) | 62.50 (13.84) | 63.29 (13.73) | ||||
| 3 mo. follow up | 63.56 (15.00) | 62.43 (15.12) | 62.76 (14.56) | 63.23 (15.59) | 1,193 | 0.86 | 4.62* | 0.50 |
| 12 mo. follow up | 63.71 (15.79) | 62.61 (15.42) | 63.27 (15.28) | 63.05 (15.94) | 1,198 | 0.51 | 8.49** | 0.76 |
Note. BMI = Brief Motivational Intervention; CDI = Computer-Delivered Intervention; BST = Booster. Perception of peer drinking reflects perception of typical number of drinks per occasion. N’s are slightly different between follow-ups and between measures, due to missing data on self-administered measures.
p<.08.
p<.05.
p < .01.
p < .001
3.5.2. Behavioral strategies to limit drinking
The 2 X 2 X 2 ANOVAs on the total strategies score showed significant treatment condition by time interactions at 3- and 12-month follow ups (Table 4). Simple effects tests showed a significant increase from baseline in the use of strategies among BMI participants at 3 months, F(1,195) = 4.77, p < .05 (WG effect size [Cohen’s d] = .18), and 12 months, F(1,200) = 6.37, p < .05 (WG effect size [Cohen’s d] = .19), but no change among CDI participants at either follow up. No booster effects were found.
3.5.3. Perceptions of peer drinking
Perceptions of peer typical quantity were evaluated in 2 X 2 X 2 (intervention by booster by time) ANOVAs at 3 and 12 months. Significant time effects reflecting decreases in perceived peer quantity were found at both follow-up time points (Table 4). The interaction of intervention condition with time approached significance at the 12-month follow-up, indicating a trend toward BMI reducing perception of peer quantity. No booster main effects or interactions were found.
3.6. Mediation Analyses
Based on the above analyses, the increased use of behavioral strategies measured at 3 months was investigated as a mediator of intervention effects on the two drinking outcomes that were significantly different between conditions through a series of multiple regressions (cf. Baron & Kenny, 1986; MacKinnon, Fairchild, & Fritz, 2007). Step A regressed the behavioral strategies change score on intervention, Step B regressed the alcohol use variable (the change score from baseline to 12 months) on intervention, and Step C regressed the alcohol use change score on the behavioral strategies change score. A final regression included both intervention and behavioral strategies, and established whether the effect of the intervention was reduced or eliminated when the behavioral strategies change score was included in the same equation. Separate mediation analyses were conducted for the two drinking outcomes (drinks per drinking day and number of drinking days) that were significantly different between intervention conditions.
3.6.1. Mediation of intervention effect on drinks per drinking day
The outcomes for the mediation steps are in Table 5. Prior analyses established that the intervention condition had a significant effect on the outcome of behavioral strategies (Step A) and on drinks per drinking day (Step B). The analyses for behavioral strategies indicated that the increased use of strategies at 3 months was significantly related to less of an increase in drinking volume at 12 months (Step C), and this relationship between strategies and consumption was maintained when intervention condition was included in the equation, while the effect of intervention was not. This indicates that the intervention group difference on drinking volume was mediated by the use of the behavioral strategies in the BMI condition.
Table 5.
Tests of mediation of behavioral strategies on drinking volume and drinking frequency
| Model 1: Tests of mediation for behavioral strategies on drinking volume | B | SE B | β | Model | |
|---|---|---|---|---|---|
| Adj. R2 | F | ||||
| Step A: Intervention effect on behavioral strategies | 2.47 | 1.08 | 0.16* | 0.02 | 5.26* |
| Step B: Intervention effect on drinks per drinking day | −0.79 | 0.38 | −0.15* | 0.02 | 4.29* |
| Step C: Behavioral strategies effect on drinks per drinking day | −0.07 | 0.03 | −0.21** | 0.04 | 7.95** |
| Final step: Effect of behavioral strategies and intervention on drinks per drinking day | |||||
| Behavioral strategies | −0.07 | 0.03 | −0.19* | 0.05 | 5.24** |
| Intervention | −0.63 | 0.40 | −0.12 | ||
| Model 2: Tests of mediation for behavioral strategies on drinking frequency | B | SE B | β | Model | |
| Adj. R2 | F | ||||
| Step A: Intervention effect on behavioral strategies | 2.47 | 1.08 | 0.16** | 0.03 | 5.26* |
| Step B: Intervention effect on number of drinking days | 1.41 | 0.65 | 0.15* | 0.02 | 4.70* |
| Step C: Behavioral strategies effect on number of drinking days | −0.03 | 0.05 | −0.04 | 0.00 | 0.35 |
| Final step: Effect of behavioral strategies and intervention on drinks per drinking day | N/A | ||||
| Behavioral strategies | |||||
| Intervention | |||||
Note. For intervention, 0 = CDI and 1 = BMI. N/A = Not Applicable since an earlier step in the mediational analyses was not significant. The drinks per drinking day variable was calculated by subtracting the baseline value from the 12-month value, so a positive difference score indicates an increase in the behavior. The number of drinking days variable was calculated by subtracting the baseline value from the 12-month value, so a positive difference score indicates an increase in the behavior. The behavioral strategies measure was calculated by subtracting the baseline score from the 3-month score so a positive difference score indicates an increase in use of strategies.
p< 05.
p < .01
3.6.2. Mediation of intervention effect on drinking frequency
The set of regressions for drinking frequency showed a different pattern, in that the step that measured the influence of behavioral strategies on number of drinking days (Step C) was not significant (Table 5). This indicated that the increased use of behavioral strategies at 3-month follow up was not related to drinking frequency at 12 months.3
4. Discussion
This trial is the first to evaluate the efficacy of a motivational interview session including personalized feedback against a computerized intervention with students who were required by their university to attend the intervention. Participants who received computerized alcohol education increased the number of drinks consumed per occasion and showed no change in frequency one year after the intervention, whereas participants who received the in-person counseling session had not changed their drinking quantity but drank more often at one year. There was also a trend for the BMI participants to have a lower average estimated BAC at both follow ups. We found that BMI participants were more likely to seek additional counseling and used more drinking reduction strategies in the months after their intervention than CDI participants, and found a trend indicating that the BMI group reduced their perception of other students’ drinking. Contrary to our hypotheses, we did not find group differences on alcohol problems, nor did we find an effect of the additional booster sessions. Our rates of recidivism were similar to those reported elsewhere (Kompalla & McCarthy, 2001), but were not different between conditions.
The finding that BMI was not associated with reductions in drinking or related problems is surprising in light of the generally positive results of other BMI trials (Larimer & Cronce, this volume). However, this trial had a high proportion of freshmen, and conducted a lengthier follow-up than other studies of mandated students (Barnett & Read, 2005; Borsari & Carey, 2005; Tevyaw, Borsari, Colby, & Monti, 2007; White et al., 2006); it may be that the increase in drinking was a natural progression of alcohol use in a young at-risk sample, or a function of the longer follow up. This trial is different from many other efficacy studies of BMI, in that ours was a comparison of two active treatment conditions, which is an inherently more difficult design to detect consistent group differences (Kazdin, 1986; Lambert & Bergin, 1994). The only published study with mandated students to date that showed significant differences between two active conditions was Borsari & Carey (2005), who included a minority (30%) of the students referred for alcohol violations because they screened for risk. Other studies of individual intervention with unscreened mandated students published since our study was initiated (White et al., 2006; Tevyaw et al., 2007) included all participants (i.e., didn’t screen for risk), and also concluded there were no significant differences between active conditions. Therefore, although our ambiguous findings were disappointing, they are consistent with other studies that had similar samples.
Although the group differences at 12 months did not reflect a differential decrease in use, the absence of an increase is a desired outcome in the context of secondary prevention and harm reduction. The BMI condition had a distinct harm reduction approach, such that there was no judgment about whether participants drank or did not drink, but some attention to the avoidance of heavy drinking and problems. In other words, the BMI may have led to participants focusing more on how much they were drinking in a drinking episode rather than whether they drank or how often they drank.
The increased use of drinking reduction strategies that were emphasized in the BMI apparently was important for the intervention group differences on the drinking quantity outcome. Our analyses indicated that the use of these strategies increased in the BMI group at 3 months, and that this increase fully mediated the difference between intervention groups at one year. Although the direction of the drinking outcome (i.e., that it reflected an increase in the CDI condition and no change in the BMI group), mediation analyses can still be meaningful (Longabaugh & Wirtz, 2001; MacKinnon, Fairchild, & Fritz, 2007). It may be that the greater use of strategies in the BMI group suppressed the increase found in the CDI group, but we cannot be confident of this interpretation without a control group. This is one of very few studies to show mediation of MI (Apodaca & Longabaugh, 2006) and is consistent with the growing literature on the efficacy of promoting specific strategies for reducing alcohol-related harm in young adults (Larimer et al., 2007). Although this study provides evidence of a mechanism of BMI, and suggests that emphasizing drinking reduction strategies may be useful, this element was not effective in reducing risky drinking in our population. Given the interpretive limitations, these constructs should be further studied and the findings replicated.
Whereas the CDI condition apparently minimized change in drinking frequency, we did not find a mechanism for this effect. There may be elements of the CDI condition that focused to a greater extent on how often students drink, but there were no explicit components of the Alcohol 101 program that concentrated on reducing frequency, nor did the program have an explicit abstinence message. Alternately, the harm reduction approach in the BMI may have led to an unanticipated increase in drinking frequency, but this is not a finding that has been previously observed (Burke, Arkowitz, & Menchola, 2003; Rubak, Sandbæk, Louritzen, & Christensen, 2005).
Our finding that individuals in the BMI condition were more likely to pursue additional counseling is consistent with basic tenets of MI, that even brief interactions with an empathic counselor can start a process of personal change (Miller & Rollnick, 2002). The personal interaction in the BMI session and/or the opportunity to discuss the need for additional counseling may have made participants more comfortable with pursuing additional help. The proportion of participants who sought further counseling is low, but higher than self-referral rates of college students at risk for alcohol problems reported elsewhere (Wechsler et al., 1994).
The hypothesis that participants who received a booster session would show greater effects was not supported. It is possible that conducting a 25-minute session one month after the initial intervention was too short, or that the timing of the booster was not optimal. More frequent boosters might be more efficacious (Stout et al., 1999), but this possibility has not been explored with college students.
Some strengths of this study are the inclusion of a large gender-balanced sample of mandated students, extensive counselor training and supervision, fidelity checks indicating that BMI was administered as designed and in a way consistent with MI principles, and use of an active comparison condition that controlled for total intervention time and tested the comparative efficacy of an approach that is increasingly being adopted. In addition, the temporal relationship in the evaluation of mediation was optimal (i.e., the measurement of the mediators preceded measurement of the outcome; Kazdin & Nock, 2003). Finally, intervention group differences in alcohol use did not emerge until the 12-month follow up, reflecting the importance of longer follow ups, particularly with students who have had a recent serious event.
4.1. Limitations
Limitations of this study include the lack of a natural history control group, which makes it impossible to know whether measured changes might have occurred without intervention. One of the practical constraints in the research with adjudicated or mandated students is the need for a rapid response to the incident. Other studies (Fromme & Corbin, 2004) have used a wait-list control but the need to intervene with this population requires that the wait list group not wait too long for intervention, so studies using this design will tend to not have controls that go beyond a few months. Other limitations are that the interventions confounded content with method of delivery (i.e., in person vs. computer). The study was conducted at a single private university and only 65% of eligible students were enrolled, limiting generalizability, although no demographic differences between students who enrolled and those who refused were found. Two-thirds of the sample was freshmen, which is typical in studies of events that come to the attention of college authorities (Wright & Slovis, 1996), but this and the exclusion of seniors may compromise generalizability to other classes. This sample may be atypical of adjudicated/mandated populations, as it had a high proportion of medical cases and their drinking. However, comparisons made to other published studies indicate that this sample had higher drinking rates than at least one study (White et al., 2006), and lower than others (Borsari & Carey, 2005; LaBrie, Lamb, Pedersen, & Quinlan, 2006; Tevyaw et al., 2007).4 Finally, it is possible that the impact of the precipitating event and/or the baseline assessment (including the TLFB; Carey et al., 2006) may have had behavioral effects, especially on the reductions from baseline to 3-month follow up.
4.2. Constraints/complexities with this population
In addition to administrative and ethical requirements to avoid no-treatment control groups, the nature of the mandated student population including heterogeneity in drinking patterns and uncontrolled delays between the mandate and the intervention may make it difficult to find differences between intervention conditions. Furthermore, the event itself and subsequent campus (e.g., judicial hearings), social group, or family responses are difficult to measure but may promote change, be related to the delay between the incident and the intervention, and/or interact with intervention (Barnett, Goldstein, Murphy, Colby, & Monti, 2006).
4.3. Implications
Findings from this study have implications for college responses to alcohol policy violations. We found ambiguous results in drinking outcome measures and no group differences on alcohol problems; however, we found greater help seeking and use of protective strategies in the in-person motivational intervention. In addition, our results suggest that protective strategies are an important mechanism of action for BMIs. Research on the efficacy of interventions that focus on facilitating additional help and promoting harm reduction strategies is warranted. Given the prevalence and severity of alcohol-related incidents with college students (Hingson et al., 2005), the costs associated with maintaining a staff to conduct in-person interventions may be worthwhile for some students, but a thorough cost-effectiveness analysis is needed. Lower cost approaches such as personalized feedback reports without in-person intervention seem to function well in comparison to more intensive interventions (e.g., Murphy et al., 2004; Walters & Neighbors, 2005; White et al., 2006) and may be preferred by college students (Black & Coster, 1996). Policies that apply lower sanctions or fines for first offenses and/or lower severity offenses, which many colleges and universities use, have not been well studied (except Cohen & Rogers, 1997). Other models that should be considered include investigating triaging or stepped care approaches (Borsari, Tevyaw, Barnett, Kahler, & Monti, 2007) that would restrict the more labor intensive interventions for higher risk offenses or repeat offenses. The absence of reductions in heavy drinking days and problems in particular in this study indicate that additional programs and/or formats should be considered for students who come to the concern of their college administrators.
Acknowledgments
This study was supported in part by Grants AA12158 and AA07459 from the National Institute on Alcohol Abuse and Alcoholism, and by a Senior Research Career Scientist Award to Dr. Monti from the Medical Research Service Office of Research and Development, Department of Veterans Affairs.
The authors wish to thank the counselors who conducted the interventions, and the research assistants who conducted the follow up interviews. We also wish to thank Suzanne Sales for data analytic assistance, and MaryLou McMillan and Frances Mantak for their assistance with the University Office of Health Education.
Portions of this study were presented in a symposium at the Research Society on Alcoholism, in Ft. Lauderdale, FL in 2003.
Footnotes
Descriptions and efficacy of other computerized and electronic interventions can be found in Walters et al. (2005) and Walters, Hester, Chiauzzi, & Miller (2005)
Alcohol 101 has motivational components, including personalized feedback and information intended to enhance risk perception, but for purposes of this study we labeled our conditions BMI and CDI.
We thought it important to attempt to identify additional mechanisms specific to the CDI condition. We therefore evaluated alcohol knowledge as measured by a post-test survey provided by the Alcohol 101 program. Participants in the CDI condition showed significantly greater alcohol knowledge than the BMI condition immediately after the intervention, t(223) = -3.06, p < .01, however, this knowledge score was not significantly related to 12-month drinking volume, β = -.09, ns, or drinking frequency, β = 0.04, ns. (i.e., Step C in the mediation chain was nonsignificant for both drinking outcomes).
Exploratory analyses indicated that medical and disciplinary referrals in our sample did not have differential responses to intervention.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Alco-calculator. Center of Alcohol Studies. Rutgers University; 1983. [Google Scholar]
- Alcohol 101 Plus: Making Safe and Responsible Decisions on Campus Fact Sheet. http://www.alcohol101plus.org/main/press.cfm. Accessed April 10, 2007.
- Anderson DS, Cohen AY. Evaluation of the Alcohol 101 program: Report of findings 2001 [Google Scholar]
- Anderson DS, Gadaleto AF. Results of the 2000 College Alcohol Survey: Comparison with 1997 results and baseline year. Fairfax, VA: Center for Advancement of Public Health, George Mason University; 2001. [Google Scholar]
- Apodaca TR, Longabaugh R. Evaluating mechanisms of change in motivational interviewing; Paper presented at the Mechanisms of Change satellite session at the 29th annual national meeting of the Research Society on Alcoholism; Baltimore, MD. Jun, 2006. [Google Scholar]
- Baer JS, Marlatt GA, Kivlahan DR, Fromme K, Larimer ME, Williams E. An experimental test of three methods of alcohol risk reduction with young adults. Journal of Consulting and Clinical Psychology. 1992;64:974–979. doi: 10.1037//0022-006x.60.6.974. [DOI] [PubMed] [Google Scholar]
- Baer JS, Stacy A, Larimer M. Biases in the perception of drinking norms among college students. Journal of Studies on Alcohol. 1991;52:580–586. doi: 10.15288/jsa.1991.52.580. [DOI] [PubMed] [Google Scholar]
- Barnett NP, Goldstein AL, Murphy JG, Colby SM, Monti PM. i'll never drink like that again”: Characteristics of alcohol-related incidents and predictors of motivation to change in college students. Journal of Studies on Alcohol. 2006;67(5):754–763. doi: 10.15288/jsa.2006.67.754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnett NP, Monti PM, Wood MD. Motivational interviewing for alcohol-involved adolescents in the emergency room. In: Wagner EF, Waldron HB, editors. Innovations in Adolescent Substance Abuse Intervention. Oxford: Elsevier; 2001. pp. 143–168. [Google Scholar]
- Barnett NP, Read JP. Mandatory alcohol intervention for alcohol-abusing college students: A systematic review. Journal of Substance Abuse Treatment. 2005;29:147–158. doi: 10.1016/j.jsat.2005.05.007. [DOI] [PubMed] [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51(6):1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Becker B, Maio RF, Longabaugh One for the road: Current concepts and controversies in alcohol intoxication and injury research; Paper presented at the Annual meeting of the Society for Academic Emergency Medicine; Denver, CO. 1996. [Google Scholar]
- Benton SL, Schmidt JL, Newton FB, Shin K, Benton SA, Newton DW. College student protective strategies and drinking consequences. Journal of Studies on Alcohol. 2004;65(1):115–121. doi: 10.15288/jsa.2004.65.115. [DOI] [PubMed] [Google Scholar]
- Black DR, Coster DC. Interest in a stepped approach model (sam): Identification of recruitment strategies for university alcohol programs. Health Education Quarterly. 1996;23(1):98. doi: 10.1177/109019819602300107. [DOI] [PubMed] [Google Scholar]
- Black JT, Wood MD. High-risk drinking on campus: Investigating the importance of adjudication status. 2007 Manuscript under review. [Google Scholar]
- Borsari B, Carey KB. Effects of a brief motivational intervention with college student drinkers. Journal of Consulting and Clinical Psychology. 2000;68(4):728–733. [PubMed] [Google Scholar]
- Borsari B, Carey KB. Two brief alcohol interventions for college student drinkers. Psychology of Addictive Behaviors. 2005;19:296–302. doi: 10.1037/0893-164X.19.3.296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borsari B, Tevyaw TO, Barnett NP, Kahler CW, Monti PM. Stepped care for mandated college students: A pilot study. American Journal on Addiction. 2007;16(2):131–137. doi: 10.1080/10550490601184498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown JM, Miller WR. Impact of motivational interviewing on participation and outcome in residential alcoholism treatment. Psychology of Addictive Behaviors. 1993;7(4):211–218. [Google Scholar]
- Burke BL, Arkowitz H, Menchola M. The efficacy of motivational interviewing: A meta-analysis of controlled clinical trials. Journal of Consulting and Clinical Psychology. 2003;71(5):843–861. doi: 10.1037/0022-006X.71.5.843. [DOI] [PubMed] [Google Scholar]
- Caldwell PE. Drinking levels, related problems and readiness to change in a college sample. Alcoholism Quarterly. 2002;20(2):1–15. [Google Scholar]
- Carey KB, Carey MP, Maisto SA, Henson JM. Brief motivational interventions for heavy college drinkers: A randomized controlled trial. Journal of Consulting and Clinical Psychology. 2006;74(5):943–954. doi: 10.1037/0022-006X.74.5.943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Century Council. Alcohol 101 (Interactive CD-ROM Program) 1998 Available at www.centurycouncil.org.
- Chen CM, Dufour MC, Yi H. Alcohol consumption among young adults ages 18–24 in the United States: Results from the 2001–2002 NESARC Survey. Alcohol Research and Health. 20042005;28:269–280. [Google Scholar]
- Cohen F, Rogers D. Effects of alcohol policy change. Alcohol and Drug Education. 1997;42(2):69–82. [Google Scholar]
- Colby JJ, Raymond GA, Colby SM. Evaluation of a college policy mandating treatment for students with substantiated drinking problems. Journal of College Student Development. 2000;41:395–404. [Google Scholar]
- Connors GJ, Walitzer KS, Dermen KH. Preparing clients for alcoholism treatment: Effects on treatment participation and outcomes. Journal of Consulting and Clinical Psychology. 2002;70(5):1161–1169. doi: 10.1037//0022-006x.70.5.1161. [DOI] [PubMed] [Google Scholar]
- Dawson DA, Grant BF, Stinson FS, Chou P. Estimating the effect of help-seeking on achieving recovery from alcohol dependence. Addiction. 2006;101:824–834. doi: 10.1111/j.1360-0443.2006.01433.x. [DOI] [PubMed] [Google Scholar]
- Dimeff LA, Baer JS, Kivlahan DR, Marlatt GA. Brief alcohol screening and intervention for college students: A harm reduction approach. Guilford Press; 1999. [Google Scholar]
- Donohue B, Allen D, Maurer A, Ozols J, DeStefano G. A controlled evaluation of two prevention programs in reducing alcohol use among college students at low and high risk for alcohol related problems. Journal of Alcohol and Drug Education. 2004;48(1):13–33. [Google Scholar]
- Flynn CA, Brown WE. The effects of a mandatory alcohol education program on college student problem drinkers. Journal of Alcohol and Drug Education. 1991;37(1):15–24. [Google Scholar]
- Fromme K, Corbin W. Prevention of heavy drinking and associated negative consequences among mandated and voluntary college students. Journal of Consulting and Clinical Psychology. 2004;72:1038–1049. doi: 10.1037/0022-006X.72.6.1038. [DOI] [PubMed] [Google Scholar]
- Haines MP, Barker G, Rice RM. The personal protective behaviors of college student drinkers: Evidence of indigenous protective norms. Journal of American College Health. 2006;55(2):69–75. doi: 10.3200/JACH.55.2.69-76. [DOI] [PubMed] [Google Scholar]
- Heather N. Brief intervention strategies. In: Hester RK, Miller WR, editors. Handbook of alcoholism treatment approaches. Boston: Allyn & Bacon; 1995. pp. 105–122. [Google Scholar]
- Hingson RW, Heeren T, Winter M, Wechsler H. Magnitude of alcohol-related morbidity and mortality among U.S. college age students 18–24: Changes from 1998 – 2001. Annual Review of Public Health. 2005;26:259–279. doi: 10.1146/annurev.publhealth.26.021304.144652. [DOI] [PubMed] [Google Scholar]
- Hurlbut SC, Sher KJ. Assessing alcohol problems in college students. Journal of American College Health. 1992;41:49–58. doi: 10.1080/07448481.1992.10392818. [DOI] [PubMed] [Google Scholar]
- Kazdin AE. Comparative outcome studies of psychotherapy: Methodological issues and strategies. Journal of Consulting and Clinical Psychology. 1986;54(1):95–105. doi: 10.1037//0022-006x.54.1.95. [DOI] [PubMed] [Google Scholar]
- Kazdin AE, Nock MK. Delineating mechanisms of change in child and adolescent therapy: Methodological issues and research recommendations. Journal of Child Psychology and Psychiatry. 2003;44(8):1116–1129. doi: 10.1111/1469-7610.00195. [DOI] [PubMed] [Google Scholar]
- Kompalla SL, McCarthy MC. The effect of judicial sanctions on recidivism and retention. College Student Journal. 2001;35(2):223–231. [Google Scholar]
- LaBrie JW, Lamb TF, Pedersen ER, Quinlan T. A group motivational interviewing intervention reduces drinking and alcohol-related consequences in adjudicated college students. Journal of College Student Development. 2006;47(3):267–280. [Google Scholar]
- LaBrie JW, Tawalbeh S, Earleywine M. Differentiating adjudicated from nonadjudicated freshmen men: The role of alcohol expectancies, tension, and concern about health. Journal of College Student Development. 2006;47(5):521. [Google Scholar]
- LaChance H. Group motivational intervention for underage college student drinkers in mandated university-based programming. Dissertation Abstracts International: Section B: The Sciences and Engineering. 2004;2004;65(6-B):3167. [Google Scholar]
- Lambert MJ, Bergin AE. The effectiveness of psychotherapy. In: Bergin AE, Garfield SL, editors. Handbook of psychotherapy and behavior change. 4. John Wiley & Sons; 1994. p. 143. [Google Scholar]
- Larimer ME, Cronce JM, Lee CM, Kilmer JR. Brief interventions in college settings. Alcohol Research and Health. 20042005;28:94–104. [PMC free article] [PubMed] [Google Scholar]
- Larimer ME, Lee CM, Kilmer JR, Fabiano PM, Stark CB, Geisner IM, et al. Personalized mailed feedback for college drinking prevention: A randomized clinical trial. Journal of Consulting and Clinical Psychology. 2007;75(2):285–293. doi: 10.1037/0022-006X.75.2.285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Longabaugh R, Donovan DM, Karno MP, McCrady BS, Morgenstern J, Tonigan JS. Active ingredients: How and why evidence-based alcohol behavioral treatment interventions work. Alcoholism: Clinical and Experimental Research. 2005;29(2):235–247. doi: 10.1097/01.alc.0000153541.78005.1f. [DOI] [PubMed] [Google Scholar]
- Longabaugh R, Woolard R, Nirenberg T, Minugh PA, Becker B, Clifford P, Carty K, Sparadeo F, Gogineni A. Evaluating the effects of a brief motivational intervention for injured drinkers in the emergency department. Journal of Studies on Alcohol. 2001;62(6):806–816. doi: 10.15288/jsa.2001.62.806. [DOI] [PubMed] [Google Scholar]
- Longabaugh R, Wirtz PW. Causal chain analysis. In: Longabaugh R, Wirtz PW, editors. Project MATCH Hypotheses: Results and Causal Chain Analyses. Project MATCH Monograph Series. Vol. 8. Rockville, MD: National Institute on Alcohol Abuse and Alcoholism; 2001. pp. 18–28. [Google Scholar]
- Mackinnon DP, Fairchild AJ, Fritz MS. Mediation analysis. Annual Review of Psychology. 2007;58:593–614. doi: 10.1146/annurev.psych.58.110405.085542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marlatt GA, Baer JS, Kivlahan DR, Dimeff LA, Larimer ME, Quigley LA, Somers JM, Williams E. Screening and brief intervention for high-risk college student drinkers: Results form a two-year follow-up assessment. Journal of Consulting and Clinical Psychology. 1998;66:604–615. doi: 10.1037//0022-006x.66.4.604. [DOI] [PubMed] [Google Scholar]
- Martens MP, Taylor KK, Damann KM, Page JC, Mowry ES, Cimini MD. Protective behavioral strategies when drinking alcohol and their relationship to negative alcohol-related consequences in college students. Psychology of Addictive Behaviors. 2004;18(4):390–393. doi: 10.1037/0893-164X.18.4.390. [DOI] [PubMed] [Google Scholar]
- McNally AM, Palfai TP. Brief group alcohol interventions with college students: Examining motivational components. Journal of Drug Education. 2003;33(2):159–176. doi: 10.2190/82CT-LRC5-AMTW-C090. 2003. [DOI] [PubMed] [Google Scholar]
- Miller WR, Rollnick S. Motivational interviewing: Preparing people for change. 2. New York: Guilford Press; 2002. [Google Scholar]
- Moyers TB, Martin T, Manuel JK, Hendrickson SML, Miller WR. Assessing competence in the use of motivational interviewing. Journal of Substance Abuse Treatment. 2005a;28:19–26. doi: 10.1016/j.jsat.2004.11.001. [DOI] [PubMed] [Google Scholar]
- Moyers TB, Martin T, Manuel JK, Miller WR. The Motivational Interviewing Intergrity (MITI) Code: Version 2.0. 2005b Available at: http://motivationalinterview.org/library/index.html.
- Murphy JG, Benson TA, Vuchinich RE, Deskins MM, Eakin D, Flood AM, et al. A comparison of personalized feedback for college student drinkers delivered with and without a motivational interview. Journal of Studies on Alcohol. 2004;65(2):200–203. doi: 10.15288/jsa.2004.65.200. [DOI] [PubMed] [Google Scholar]
- Murphy JG, Duchnick JJ, Vuchinich RE, Davison JW, Karg R, Olson AM, Smith AF, Coffey TT. Relative efficacy of a brief motivational intervention for college student drinkers. Psychology of Addictive Behaviors. 2001;15:373–379. doi: 10.1037//0893-164x.15.4.373. [DOI] [PubMed] [Google Scholar]
- Neighbors C, Larimer ME, Lewis MA. Targeting misperceptions of descriptive drinking norms: Efficacy of a computer delivered personalized normative feedback intervention. Journal of Consulting and Clinical Psychology. 2004;72:434–447. doi: 10.1037/0022-006X.72.3.434. [DOI] [PubMed] [Google Scholar]
- Palmer RS. Dissertation Abstracts International: Section B: The Sciences and Engineering. 2004. Efficacy of the alcohol skills training program in mandated and nonmandated heavy drinking college students. [Google Scholar]
- Porter JR. Arrests for alcohol rise on campus. The Chronicle of Higher Education. 2006 October 27; [Google Scholar]
- Reis J, Riley W, Lokman L, Baer J. Interactive multimedia preventive alcohol education: A technology application in higher education. Journal of Drug Education. 2000;30(4):399–421. doi: 10.2190/LWMQ-9CQA-B78H-9MA7. [DOI] [PubMed] [Google Scholar]
- Rubak S, Sandbæk A, Lauritzen T, Christensen B. Motivational interviewing: A systematic review and meta-analysis. British Journal of General Practice. 2005 April;:305–312. [PMC free article] [PubMed] [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, De La Fuente J, Grant M. Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption-II. Addiction. 1993;88:791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- Sharmer L. Evaluation of alcohol education programs on attitude, knowledge, and self-reported behavior of college students. Evaluation and the Health Professions. 2001;24:336–357. doi: 10.1177/01632780122034957. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB. Alcohol timeline followback users' manual. Toronto, Canada: Addiction Research Foundation; 1995. [Google Scholar]
- Stone GL, Lucas J. Disciplinary counseling in higher education: A neglected challenge. Journal of Counseling and Development. 1994;72:234–238. [Google Scholar]
- Stout RL, Rubin A, Zwick W, Zywiak W, Bellino L. Optimizing the cost-effectiveness of alcohol treatment: A rationale for extended case monitoring. Addictive Behaviors. 1999;24(1):17–35. doi: 10.1016/s0306-4603(98)00029-x. [DOI] [PubMed] [Google Scholar]
- Tevyaw TO, Borsari B, Colby SM, Monti PM. Peer enhancement of a brief motivational intervention with mandated college students. Psychology of Addictive Behaviors. 2007;21(1):114–119. doi: 10.1037/0893-164X.21.1.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The National Center on Addiction and Substance Abuse. Wasting the Best and the Brightest: Substance Abuse at America’s Colleges and Universities. Commission on Substance Abuse at Colleges and Universities; Columbia University: 2007. [Google Scholar]
- US Department of Health and Human Services. Center for Substance Abuse Treatment, Treatment Improvement Protocol Series (Publication No. 93–2010) 1993. Guidelines for treatment of alcohol and other drug-abusing adolescents. [Google Scholar]
- Walters ST, Baer JS. Talking with college students about alcohol: Motivational strategies for reducing abuse. New York: Guilford; 2006. [Google Scholar]
- Walters ST, Hester RK, Chiauzzi E, Miller E. Demon rum: High-tech solutions to an age-old problem. Alcoholism: Clinical and Experimental Research. 2005;29(2):270. doi: 10.1097/01.alc.0000153543.03339.81. [DOI] [PubMed] [Google Scholar]
- Walters ST, Miller E, Chiauzzi E. Wired for wellness: e-interventions for addressing college drinking. Journal of Substance Abuse Treatment. 2005;29:139–145. doi: 10.1016/j.jsat.2005.05.006. [DOI] [PubMed] [Google Scholar]
- Walters ST, Neighbors C. Feedback interventions for college alcohol misuse: What, why and for whom? Addictive Behaviors. 2005;30(6):1168–1182. doi: 10.1016/j.addbeh.2004.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walters ST, Vader AM, Harris TR. Prevention Science. Springer Netherlands: 2006. A controlled trial of web-based feedback for heavy drinking college students. published in advance online. [DOI] [PubMed] [Google Scholar]
- Wechsler H, Davenport A, Dowdall GW, Moeykens B, Castillo S. Health and behavioral consequences of binge drinking in college: A national survey of students at 140 campuses. Journal of the American Medical Association. 1994;272:1672–1677. [PubMed] [Google Scholar]
- Werch CE, Gorman DR. Factor analysis of internal and external self-control practices for alcohol consumption. Psychological Reports. 1986;59:1207–1213. doi: 10.2466/pr0.1986.59.3.1207. [DOI] [PubMed] [Google Scholar]
- White HR, Morgan TJ, Pugh LA, Celinska K, Labouvie EW, Pandina RJ. Evaluating two brief substance-use interventions for mandated college students. Journal of Studies on Alcohol. 2006;67(2):309–317. doi: 10.15288/jsa.2006.67.309. [DOI] [PubMed] [Google Scholar]
- World Health Organization Brief Intervention Study Group. A cross-national trial of brief interventions with heavy drinkers. American Journal of Public Health. 1996;86(7):948–955. doi: 10.2105/ajph.86.7.948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright SW, Slovis CM. Drinking on campus: Undergraduate intoxication requiring emergency care. Archives of Pediatric and Adolescent Medicine. 1996;150:699–702. doi: 10.1001/archpedi.1996.02170320045007. [DOI] [PubMed] [Google Scholar]
- Yu J, Evans PC, Perfetti L. Attitudes toward seeking treatment among alcohol-using college students. The American Journal of Drug and Alcohol Abuse. 2003;29(3):671–690. doi: 10.1081/ada-120023464. [DOI] [PubMed] [Google Scholar]


