We recently reported a meta-analysis of 94 randomized placebo-controlled trials of blood pressure-lowering drugs in which the prevalence of headache was reported [1]. On average, one-third fewer people reported headache in the treated groups than in the placebo groups [odds ratio (OR) 0.67; 95% confidence interval (CI) 0.61, 0.74; P < 0.001]. There was a statistically significantly reduced prevalence of headache in separate analyses of four classes of blood pressure-lowering drugs, thiazides, β-blockers, ACE inhibitors and angiotensin-II receptor antagonists, an observation that suggested that blood pressure reduction itself prevents headache.
We excluded calcium channel blockers in this analysis because they are likely to affect the prevalence of headache in two opposite ways, tending to reduce the prevalence because they lower blood pressure but to increase it because they cause vasodilation. We here present the results on calcium channel blockers and headache, the net effect according to dose, from our meta-analysis of randomized trials [1, 2].
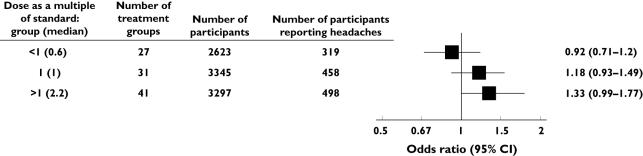
There were 60 randomized placebo-controlled trials of calcium channel blockers in fixed dose that recorded data on headache, with 99 treatment groups and 8087 participants in total. We divided the 99 treatment groups into three categories according to dose: standard dose (as previously defined [2], 31 treatment groups), below standard dose (median 0.6-fold, 27 treatment groups) and above standard dose (median 2.2-fold, 41 treatment groups). We analysed the data as previously reported [1], calculating the OR (odds of headache:no headache in participants allocated calcium channel blockers divided by that for placebo) for each category.
The effect on headache showed a striking effect of dose (see Figure 1), with a trend which was statistically significant (P= 0.03). Calcium channel blockers reduced headache at low (below standard) dose (OR 0.92, 95% CI 0.71, 1.2), increased it at high (above standard) dose (OR 1.33, 95% CI 0.99, 1.77) and had an intermediate effect at standard dose (OR 1.18, 95% CI 0.93, 1.49).
Figure 1.
Meta-analysis of 60 randomized placebo-controlled trials of calcium channel blockers: odds ratio of headache in relation to dose
The effect of dose on the risk of headache supports the two opposing actions. The increase in risk caused by vasodilation is likely to be strongly dose dependent, because the prevalence of other symptoms caused by vasodilation (flushing, ankle oedema) is strongly dose dependent [2]. The reduction in risk through lowering blood pressure is not likely to be strongly dose dependent, however, because in the trials of the other four categories of blood pressure-lowering drugs no detectable association between dose of drug and headache was apparent, an observation that is not surprising because the association of blood pressure reduction with dose is weak [2]. The effect of vasodilation on headache predominates over that of blood pressure reduction at standard and greater than standard doses, but not at below standard doses. This is of practical importance in specifying medical therapy designed to improve the efficacy and safety of blood pressure-lowering therapy.
References
- 1.Law M, Morris JK, Jordan R, Wald NJ. Headaches and the treatment of blood pressure: results from a meta-analysis of 94 randomized placebo-controlled trials with 24000 participants. Circulation. 2005;112:2301–6. doi: 10.1161/CIRCULATIONAHA.104.529628. [DOI] [PubMed] [Google Scholar]
- 2.Law MR, Wald NJ, Morris JK, Jordan RE. Value of low dose combination treatment with blood pressure lowering drugs: analysis of 354 randomised trials. BMJ. 2003;326:1427–15. doi: 10.1136/bmj.326.7404.1427. [DOI] [PMC free article] [PubMed] [Google Scholar]