The use of herbal remedies in the Western world has recently increased dramatically. Events such as the withdrawal of kava kava and warnings regarding drug interactions with St John's Wort have clearly shown that herbal remedies, like conventional pharmaceutical products, can cause harm [1]. However, herbal remedies are often regarded by the public as ‘safe’ and ‘natural’, and therefore patients may not spontaneously reveal their use when asked a medication history. We report some audit findings regarding the extent of herbal medicine intake by patients admitted acutely to a medical assessment unit, and specifically highlight the case of one patient where the use of such compounds may have contributed to the admission.
A 77-year-old lady was admitted to hospital with epigastric pain and haematemesis. She was haemodynamically stable without a significant drop in blood haemoglobin. Her clotting was normal. The patient had had identical symptoms 4 months previously and a gastroscopy at that time had shown a large sliding intrathoracic hiatus hernia with severe oesophagitis. She had been started on lansoprazole 30 mg daily and surgery was planned. Further questioning on the second admission revealed that the patient had been taking garlic, St John's Wort, feverfew, echinacea and ginseng, in addition to her usual prescribed medication (which did not include nonsteroidal anti-inflammatory drugs). The herbal remedies were stopped at this time. She went on to have a Nissen fundoplication and made a full recovery.
This patient was identified during an audit of acute medical emergency admissions to our hospital. Following their admission by the attending doctor, patients were further questioned about their intake of over-the-counter, herbal and homeopathic medications, and this was compared with their history in the case notes. Of the 100 patients (40 males) questioned, 24 (24%) were taking herbal remedies using a total of 40 products, with some patients on more than one product. The most popular product was garlic. Most of these patients (20; 83%) were using herbal remedies concomitantly with a prescription medication. Eleven (46%) of the 24 patients were taking herbal remedies which have either documented toxicity or a known interaction with prescription drugs. Only one (4.2%) of the patients taking a herbal preparation had its use documented in the case notes.
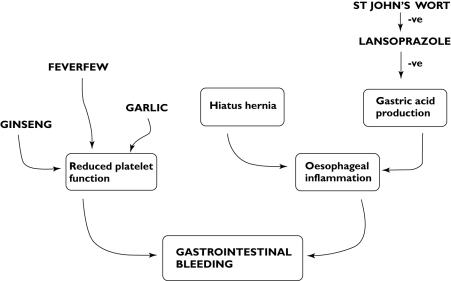
Herbal remedies cause problems either through their inherent toxicity or by interacting with other drugs or herbals [2]. For example, kava kava (Piper methysticum), taken for anxiety, was withdrawn from general sale in 2003 after 78 cases of hepatoxicity related to its use were reported [3]. St John's Wort, an extract from the plant Hypericum perforatum used in the management of mild to moderate depression, can induce various P450 isoforms and the drug efflux pump P-glycoprotein [4, 5]. The induction of these proteins results in increased drug clearance and can therefore reduce the concentrations and effectiveness of certain drugs. The patient described highlights the potentially dangerous interactions that can occur with herbal medicines. The patient had a known history of gastro-oesophageal disease treated appropriately with lansoprazole, yet presented with haematemesis and was also found to be on five herbal preparations. Garlic, feverfew and ginseng all inhibit platelet aggregation and may therefore increase the risk of bleeding. The antiplatelet action of garlic (Alium sativum) has been blamed for spontaneous postoperative bleeding [6], and both feverfew (Tanacetum parthenium) and ginseng also have a significant inhibitory effect on platelet aggregation mediated by inhibiting the production and/or release of prostaglandins and thromboxanes [7]. Although individually these herbals may have mild effects on platelets, in combination they may have had a significant effect on platelet function in this patient, increasing the likelihood of bleeding from an inflamed oesophagus. A contributory factor may also have been an interaction between lansoprazole and St John's Wort. Lansoprazole is metabolized by the P450 isoform CYP2C19, which is induced by St John's Wort [8]. Thus, in our patient, the induction oflansoprazole metabolism may have reduced its plasma concentrations and hence its effectiveness in treating the gastro-oesophageal reflux (Figure 1).
Figure 1.
An example of potential pharmacokinetic and pharmacodynamic interactions between pathology, prescribed and herbal medicines
The use of herbal remedies varies: an Australian study of medical and surgical patients indicated that 70% had used at least one preparation in the preceding 12 months [9]. In the UK, figures of 44% in rheumatology outpatients [10] and 12.8% in a survey of 22 000 people [11] have been reported. Our figure of 24% is consistent with the notion that these preparations are widely used. Given such high usage, it is vital to ask patients specifically about their herbal remedy use during a routine drug history. However, in practice, this is rarely done [9]. Our audit data are consistent with this in that only one out of the 24 patients (4.2%) had herbal use documented in their case notes. This is an important clinical governance issue, since these allegedly innocent therapies may be responsible, at least in part, for medical problems or adverse reactions requiring admission to hospital.
References
- 1.Medicines and Healthcare Products Regulatory Agency. Report on the ‘Safety of Herbal Medicinal Products’. London: MHRA; 2002. [Google Scholar]
- 2.Izzo AA, Ernst E. Interactions between herbal medicines and prescribed drugs. A systematic review. Drugs. 2001;61:2163–75. doi: 10.2165/00003495-200161150-00002. [DOI] [PubMed] [Google Scholar]
- 3.Clouatre DL. Kava-kava: examining new reports of toxicity. Toxicol Lett. 2004;150:85–96. doi: 10.1016/j.toxlet.2003.07.005. [DOI] [PubMed] [Google Scholar]
- 4.Roby CA, Anderson GD, Kantor E, Dryer DA, Burstein AH. St John's Wort: effect on CYP3A4 activity. Clin Pharmacol Ther. 2000;67:451–7. doi: 10.1067/mcp.2000.106793. [DOI] [PubMed] [Google Scholar]
- 5.Hennessy M, Kelleher D, Spiers JP, Barry M, Kavanagh P, Back D, Mulcahy F, Feely J. St John's wort increases expression of P-glycoprotein: implications for drug interactions. Br J Clin Pharmacol. 2002;53:75–82. doi: 10.1046/j.0306-5251.2001.01516.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Burnham BE. Garlic as a possible risk factor for postoperative bleeding. Plast Reconstr Surg. 1995;95:213. doi: 10.1097/00006534-199501000-00060. [DOI] [PubMed] [Google Scholar]
- 7.Abebe W. Herbal medication: potential for adverse interactions with analgesic drugs. J Clin Pharm Ther. 2002;27:391–401. doi: 10.1046/j.1365-2710.2002.00444.x. [DOI] [PubMed] [Google Scholar]
- 8.Wang LS, Zhou G, Zhu B, Wu J, Wang JG, Abd El-Aty AM, Tong L, Liu J, Yang TL, Wang D, Zhong XY, Zho HH. St John's wort induces both cytochrome P450 3A4-catalyzed sulfoxidation and 2C19-dependent hydroxylation of omeprazole. Clin Pharmacol Ther. 2004;75:191–7. doi: 10.1016/j.clpt.2003.09.014. [DOI] [PubMed] [Google Scholar]
- 9.Cockayne NL, Duguid M, Shenfiels GM. Health professionals rarely record history of complementary and alternative medicines. Br J Clin Pharmacol. 2004;59:254–8. doi: 10.1111/j.1365-2125.2004.02328.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Holden W, Joseph J, Williamson L. Use of herbal remedies and potential drug interactions in rheumatology outpatients. Ann Rheum Dis. 2005;64:790. doi: 10.1136/ard.2004.029991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Harrison RA, Holt D, Pattison DJ, Elton PJ. Who and how many people are taking herbal supplements? A survey of 21,923 adults. Int J Vitam Nutr Res. 2004;74:83–6. doi: 10.1024/0300-9831.74.3.183. [DOI] [PubMed] [Google Scholar]