Abstract
What is already known about this subject
Severe hypoglycaemia has been reported after concomitant use of clarithromycin and glibenclamide.
Glibenclamide is a substrate for the transporters P-glycoprotein and OATP2B1.
Clarithromycin inhibits P-glycoprotein and grapefruit juice inhibits OATP2B1.
What this study adds
Clarithromycin increases the plasma concentration of glibenclamide.
A pharmacokinetic interaction may explain reported hypoglycaemia during simultaneous administration of clarithromycin and glibenclamide.
Grapefruit juice has no effect on the pharmacokinetics of glibenclamide.
Aims
Case reports suggest that clarithromycin can increase the glucose-lowering effect of glibenclamide which is metabolized mainly by CYP2C9 and is a substrate for P-glycoprotein and OATP2B1. Our objective was to evaluate whether the P-glycoprotein inhibitor, clarithromycin, increases and the putative OATP2B1 inhibitor, grapefruit juice, decreases plasma concentrations of glibenclamide.
Methods
In a randomized three-phase crossover study, 12 subjects ingested 250 mg clarithromycin or placebo twice daily or 200 ml grapefruit juice three times daily for 2 days. On day 3, they ingested 0.875 mg glibenclamide with sugar water or grapefruit juice. Concentrations of glibenclamide and clarithromycin in plasma, glucose in blood, and excretion of hydroxyglibenclamide into urine were measured up to 12 h.
Results
Clarithromycin increased the peak concentration (Cmax) of glibenclamide to 1.25-fold (95% confidence interval (CI) 1.12, 1.40; P < 0.01) and the area under the plasma concentration-time curve to 1.35-fold (95% CI 1.21, 1.50; P < 0.01) compared with the placebo phase. The time to Cmax, the half-life of glibenclamide, and the amount of hydroxyglibenclamide excreted into urine remained unaltered. Grapefruit juice did not change the pharmacokinetics of glibenclamide. Clarithromycin concentrations implied a good compliance. Blood glucose did not deviate between the phases.
Conclusions
Clarithromycin increased plasma concentrations of glibenclamide, possibly by inhibiting P-glycoprotein in the intestinal wall. Although not seen with the present study design, clarithromycin may enhance the effect of glibenclamide by increasing plasma glibenclamide concentrations, which warrants close monitoring of blood glucose during their co-administration. Grapefruit juice had no effect on glibenclamide pharmacokinetics.
Keywords: clarithromycin, glibenclamide, grapefruit juice, OATP2B1, P-glycoprotein, pharmacokinetics
Introduction
The bioavailability of the oral sulphonylurea antidiabetic glibenclamide is high (over 90%) when used as a micronized formulation, whereas the bioavailability of the nonmicronized formulation is greatly dependent on gastric pH [1, 2]. Glibenclamide is extensively bound to plasma proteins (99%) and metabolized mainly by CYP2C9 [2–4]. Accordingly, inhibitors and inducers of CYP2C9 can change the pharmacokinetics and pharmacodynamics of glibenclamide [5, 6]. In a recent in vitro study, glibenclamide was identified as a substrate for an uptake transporter, organic anion transporting polypeptide OATP2B1 (OATP-B) [7], which is expressed, for example, in the intestine and the liver [8]. In addition, glibenclamide is a substrate for the efflux transporter P-glycoprotein [9]. In the intestinal wall, both of these transporters are expressed in the brush border of epithelial cells, but they have opposite roles there. OATP2B1 facilitates and P-glycoprotein limits the absorption of substrate drugs.
Grapefruit juice increases plasma concentrations of several CYP3A4 substrate drugs [10–15], most likely by inhibiting intestinal CYP3A4 [16]. Recently, grapefruit juice has been reported to reduce considerably plasma concentrations of fexofenadine, celiprolol, and talinolol [17–19]. The decreased bioavailability of fexofenadine during concomitant grapefruit juice consumption may be a consequence of inhibition of OATP1A2 (previously known OATP-A), in the intestinal wall [17, 20]. As grapefruit juice is also thought to be an inhibitor of OATP2B1 [7], an inhibition of intestinal OATP2B1 by grapefruit juice could reduce the absorption of glibenclamide.
The macrolide clarithromycin, a potent inhibitor of CYP3A4 and P-glycoprotein, increases the plasma concentrations of several P-glycoprotein substrate drugs. For instance, increased bioavailability of oral digoxin by clarithromycin can be explained by inhibition of P-glycoprotein [21]. Severe hypoglycaemia has been reported after concomitant administration of clarithromycin with glibenclamide [22, 23]. Clarithromycin could increase the plasma concentrations of glibenclamide by inhibiting P-glycoprotein and increase the glucose-lowering effect of this sulphonylurea. The present study was conducted to investigate possible effects of clarithromycin and grapefruit juice on the pharmacokinetics of glibenclamide in healthy subjects.
Methods
Subjects
Twelve healthy volunteers (10 men and two women, age range 20–27 years and weight range 51–98 kg) participated in the study. Each subject was ascertained to be healthy by means of a medical history, clinical examination, and routine laboratory tests including blood glucose before they were enrolled in the study. A negative pregnancy test was required of the female participants. The subjects were not using any continuous medication, e.g. oral contraceptives, and all of them were nonsmokers. Use of grapefruit, orange, or apple products was forbidden during the study and from 3 days before the first study day. The study protocol was approved by the Ethics Committee for Studies in Healthy Subjects of the Hospital District of Helsinki and Uusimaa and by the National Agency for Medicines. Subjects gave their written informed consent before entering the study.
Study design
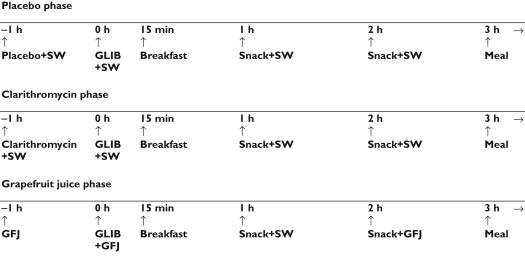
A randomized crossover study design with three phases was used with a washout period of 2 weeks. In the placebo phase, the volunteers ingested placebo (placebo for clarithromycin), at 07.00 h and 18.00 h on days 1 and 2, and at 08.00 h on day 3. In the clarithromycin phase, the volunteers ingested 250 mg clarithromycin (one Klacid 250 mg tablet, Abbot Scandinavia AB, Solna, Sweden) at 07.00 h and 18.00 h on days 1 and 2, and at 08.00 h on day 3. In addition, on day 3 of the placebo and clarithromycin phases, the volunteers ingested 200 ml 8% sugar water (8 g sucrose per 100 ml tap water to balance the carbohydrate content of grapefruit juice) at 08.00 h, 09.00 h, and 11.00 h (Figure 1). In the grapefruit juice phase, the volunteers ingested 200 ml normal-strength grapefruit juice (Valio täysmehu, Valio, Helsinki, Finland) at 07.00 h, 12.00 h, and 20.00 h for 2 days. On day 3, they ingested 200 ml grapefruit juice at 08.00 h, 09.00 h, and 11.00 h. In addition, on day 3 of each of the three phases, the volunteers ingested 100 ml sugar water at 10.00 h. In each phase, the subjects received 0.875 mg (one half of a Semi Euglucon 1.75 mg tablet, Roche Diagnostics GmbH, Mannheim, Germany) orally at 09.00 h (with 200 ml sugar water in the placebo and clarithromycin phases, and with 200 ml grapefruit juice in the grapefruit juice phase) on day 3. The percentage deviation of the weight of halved glibenclamide tablets did not exceed 2%. The volunteers fasted overnight before the administration of glibenclamide. After ingestion of the drug, they were seated for the first 3 h. A standardized breakfast was served precisely 15 min, and a standardized snack rich in carbohydrates was served precisely 1 h and 2 h after the administration of glibenclamide. A standardized warm meal was served after 3 h, and a standard light meal was served after 7 h. The breakfast was eaten within 10 min and contained approximately 370 kcal energy, 70 g carbohydrates, 8 g protein, and 6 g fat. Food intake was identical during each day of glibenclamide administration. The subjects were under direct medical supervision during the days of administration of glibenclamide. Drinks and food rich in carbohydrates, glucose for intravenous use, and glucagon for intramuscular use were available.
Figure 1.
Carbohydrate intake and meals in relation to administration of glibenclamide 0.875 mg (GFJ = grapefruit juice, SW = sugar water, GLIB = glibenclamide)
Sampling and determination of blood glucose
On the days of administration of glibenclamide, a forearm vein of each subject was cannulated and kept patent with an obturator. Timed blood samples were drawn into tubes that contained ethylenediaminetetraacetic acid (EDTA) 1 h before and 0.5, 1, 1.5, 2, 2.5, 3, 4, 5, 7, 9, and 12 h after administration of glibenclamide. Blood glucose was determined immediately after each blood sampling by the glucose oxidase method with the Precision G Blood Glucose Testing System (Medisense, Bedford, Mass., USA). Additional blood glucose measurements were performed when necessary. Plasma was separated after the determination of blood glucose and stored at −70°C until analysis of drug concentrations.
The urine was collected cumulatively from 0–12 h, the volume was measured, and an aliquot was stored at −70°C until analyzed.
Determination of drug concentrations in plasma and urine
The internal standard glimepiride (Hoechst Marion Roussel, Frankfurt, Germany) was added to each sample (1.0 ml), followed by 1.0 ml 0.1 m hydrochloric acid-potassium chloride buffer. Glibenclamide (Orion Pharma, Espoo, Finland) and hydroxyglibenclamide were extracted with diethyl ether as previously described [24]. The organic phase was evaporated to dryness under a stream of nitrogen at 30°C and the residue was dissolved in acetonitrile (57%):10 mmol l−1 ammonium formate solution (pH 3.5, 43%). Concentrations of glibenclamide and hydroxyglibenclamide were quantified by liquid chromatography-tandem mass spectrometry with a Perkin-Elmer SCIEX API 2000 LC/MS/MS System (Sciex Division of MDS Inc, Toronto, Ontario, Canada) [25]. Chromatography was performed on a Hypersil BDS-C18 reversed phase column (100 × 4 mm internal diameter, 3 µm particle size; Agilent, Waldbronn, Germany) protected by a Hypersil BDS-C18 guard column (4 × 4 mm internal diameter, 5 µm particle size; Agilent). Liquid chromatographic separation was isocratic and the mobile phase consisted of 10 mmol l−1 ammonium formate (pH 3.5; 43%) and acetonitrile (57%). An aliquot of 10 µl was injected at the mobile phase flow rate of 0.5 ml min−1. The mass spectrometer was operated in the positive atmospheric pressure chemical ionization mode and the samples were analysed via multiple reaction monitoring employing precursor ion to product ion. The ion transitions were m/z 494 to m/z 369 for glibenclamide, m/z 510 to m/z 369 for hydroxyglibenclamide, and m/z 491 to m/z 352 for glimepiride. The limit of quantification for plasma glibenclamide, defined as the lowest concentration with signal-to-noise ratio greater than 10, was 0.25 ng ml−1. The interday coefficient of variation (CV) for plasma glibenclamide was 7.2% at 0.5 ng ml−1 (n = 19), 2.9% at 5.0 ng ml−1 (n = 19), 2.7% at 50 ng ml−1 (n = 18), and 3.9% at 150 ng ml−1 (n = 18). A signal to noise ratio of 10:1 was used as the limit of detection for hydroxyglibenclamide, and its concentration in urine is given in arbitrary units (U) relative to the ratio of its peak height and that of the internal standard (glimepiride). The interday CV for urine hydroxyglibenclamide was 6.5% (n = 10).
For determination of clarithromycin (I.D.C. Abbott Laboratories LTD., Queensborough, England) [26], saturated sodium carbonate solution (0.4 ml) and the internal standard roxithromycin (Roussel Uclaf, Paris, France) were added to plasma (0.5 ml). The samples were vortexed with 2.5 ml tertiary-butyl methyl ether. After centrifugation, the organic phase was transferred and evaporated to dryness under a stream of nitrogen at 35°C. The residue was dissolved with acetonitrile (32%):methanol (10%):5 mmol l−1 ammonium acetate (58%, pH 5) solution. Clarithromycin concentrations were quantified by liquid chromatography-tandem mass spectrometry with the SCIEX API 2000 LC/MS/MS System [27]. An aliquot of 3 µl was injected at a mobile phase flow rate of 0.2 ml min−1. Separation was performed on SunFire C18 column (100 × 2.1 mm internal diameter, 3.5 µm particle size, Waters Corporation, Milford, MA, United States). The mass spectrometer was operated in the positive electrospray ionization mode and the samples were analyzed via multiple reaction monitoring mode. The ion transitions were m/z 748.4 to m/z 158 for clarithromycin and m/z 837.5 to m/z 158 for roxithromycin. The quantification limit was 0.2 ng ml−1 and the interday CV was 6.9% at 20 ng ml−1 (n = 6), 2.5% at 500 ng ml−1 (n = 8), and 6.8% at 4000 ng ml−1 (n = 8).
Pharmacokinetic calculations
The peak concentration in plasma (Cmax) and time to Cmax (tmax) were obtained directly from the original data. The terminal log-linear phase of the plasma glibenclamide concentration-time curve was identified visually for each subject. The elimination rate constant (λz) was determined by a linear regression analysis of the log-linear part of the plasma concentration-time curve. The area under the glibenclamide concentration-time curve from time 0 to infinity (AUC(0,∞)) was calculated with extrapolation to infinity by dividing the last measured concentration by λz. On average, 2.3% (5.6% maximum) of the AUC(0, ∞) was extrapolated. The elimination half-life (t1/2) was calculated by the equation:
The pharmacokinetics of clarithromycin were characterized by Cmax and AUC(0,13 h), that is, the AUC from 1 h before up to 12 h after the administration of glibenclamide.
Pharmacodynamic response
The decremental area (the net area below the baseline) under the blood glucose concentration-time curve was used to characterize the pharmacodynamic response to the administration of glibenclamide. It was calculated by the linear trapezoidal rule from time 0–3 h and 0–7 h. The maximum increase and the maximum decrease compared with the baseline blood glucose concentration (before the administration of glibenclamide) were also calculated for the time period 0–3 h.
Statistical methods
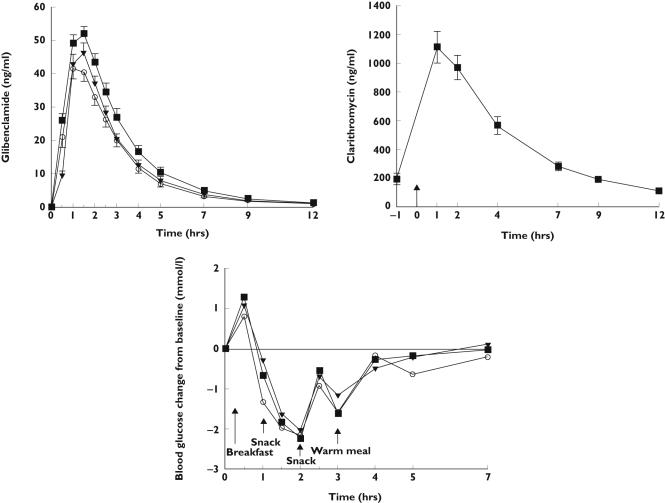
The data are expressed in the text and Table 1 as mean values ± SD, except for tmax, which is expressed as median with range. For clarity, in Figure 2, the glibenclamide and clarithromycin concentration data are expressed as mean ± SEM and blood glucose changes as mean values. The pharmacokinetic variables and the glucose response data after the three treatments (pharmacokinetic variables of glibenclamide after log-transformation) were compared by use of repeated measures analysis of variance (anova) and a posteriori testing with the paired t-test with the Bonferroni correction. For all pharmacokinetic variables except tmax, 95% confidence intervals (CI) were calculated on the geometric mean ratio between the clarithromycin and placebo (control) phases and between the grapefruit juice and control phases. For all pharmacodynamic variables, 95% CIs were calculated on the mean difference between phases. The tmax values were analyzed by Friedman's two-way anova and the Wilcoxon signed-rank test. The statistical program Systat for Windows, version 6.0.1 (SPSS Inc, Chicago, Ill) was used for the analysis. Differences were considered statistically significant when P < 0.05.
Table 1.
Pharmacokinetic variables of 0.875 mg glibenclamide in 12 healthy volunteers after 3 days of pretreatment with clarithromycin (250 mg twice daily), placebo (control), or grapefruit juice (200 ml thrice daily)
| Variable | Placebo (control) phase | Clarithromycin phase | Grapefruit juice phase |
|---|---|---|---|
| Cmax (ng ml−1) | 43.6 ± 9.24 | 54.0 ± 8.21* | 46.6 ± 9.81 |
| Geometric mean ratio (95% CI) | 1 | 1.25 (1.12, 1.40) | 1.07 (0.93, 1.23) |
| tmax (h) | 1.25 (1–1.5) | 1.5 (1–2) | 1.5 (1–1.5) |
| t1/2 (h) | 2.4 ± 0.32 | 2.3 ± 0.31 | 2.3 ± 0.32 |
| Geometric mean ratio (95% CI) | 1 | 0.96 (0.91, 1.02) | 0.98 (0.90, 1.07) |
| AUC(0,∞) (ng ml−1 h) | 133 ± 40.4 | 177 ± 46.4* | 139 ± 33.7 |
| Geometric mean ratio (95% CI) | 1 | 1.35 (1.21, 1.50) | 1.07 (0.99, 1.15) |
| Metabolite excreted (0–12 h) (U) | 6230 ± 2210 | 7690 ± 1850 | 7160 ± 1640 |
| Geometric mean ratio (95% CI) | 1 | 1.26 (0.88, 1.82) | 1.19 (0.84, 1.67) |
Data are mean values ± SD unless otherwise shown; tmax data are given as median with range. Geometric ratio is clarithromycin or grapefruit juice phase compared with placebo phase. Cmax, peak plasma concentration; tmax, time to reach Cmax; t1/2, half-life; AUC(0,∞), area under the plasma concentration-time curve from time 0 to infinity.
P < 0.01 vs. placebo and grapefruit juice phases.
Figure 2.
Upper panel Mean ± SEM plasma concentrations of glibenclamide after single oral doses of 0.875 mg glibenclamide in 12 healthy volunteers. Glibenclamide was taken after 3 days of pretreatment with clarithromycin 250 mg twice a day (▪) or placebo (○) or after ingestion of 200 ml grapefruit juice 3 times a day (▾). Middle panel Mean ± SEM plasma concentrations of clarithromycin on day of glibenclamide administration (↑ shows the time of glibenclamide administration). Lower panel Mean change in blood glucose after administration of glibenclamide during clarithromycin phase (▪), placebo phase (○), and grapefruit juice phase (▾)
Results
Pharmacokinetics of glibenclamide
The mean plasma concentrations of glibenclamide were higher in the clarithromycin phase than in the placebo and grapefruit juice phases (Figure 2). During the clarithromycin phase, the mean AUC(0,∞) of glibenclamide was 1.35-fold (P < 0.01) and the Cmax was 1.25-fold (P < 0.01) compared with the respective values during the placebo phase (Table 1), but the tmax and t1/2 were not altered. Grapefruit juice did not significantly change the pharmacokinetics of glibenclamide. There were no significant differences in the amount of hydroxyglibenclamide excreted into urine between the three phases.
Clarithromycin concentrations
Plasma concentrations of clarithromycin indicated a good compliance with its ingestion (Figure 2), and the concentrations were about 30-fold higher than those of glibenclamide. The mean Cmax and AUC(0,13 h) of clarithromycin were 1123 ng ml−1 (range 596–1710 ng ml−1) and 4750 ng ml−1 h (range 2710–7090 ng ml−1 h), respectively. The median tmax was 2 h (range 2–3 h).
Blood glucose concentrations
There were no statistically significant differences in the blood glucose concentrations between the clarithromycin, grapefruit juice, and placebo phases (Table 2, Figure 2). No subject experienced severe hypoglycaemia.
Table 2.
The blood glucose response to 0.875 mg oral glibenclamide in 12 healthy volunteers after 3 days of pretreatment with clarithromycin (250 mg twice daily), placebo (control), or grapefruit juice (200 ml thrice daily)
| Blood glucose variable | Placebo (control) phase | Clarithromycin phase | Grapefruit juice phase |
|---|---|---|---|
| Decremental AUC(0,3 h) (mmol l−1 h) | 3.11 ± 1.57 | 2.41 ± 1.47 | 2.08 ± 1.57 |
| Mean difference from control phase (95% CI) | −0.70 (−2.31, 0.92) | −1.03 (−2.78, 0.73) | |
| Decremental AUC(0,7 h) (mmol l−1 h) | 5.28 ± 3.25 | 3.79 ± 2.32 | 3.38 ± 4.07 |
| Mean difference from control phase (95% CI) | −1.48 (−4.72, 1.76) | −1.89 (−6.33, 2.54) | |
| Maximum increase (mmol l−1) | 0.80 ± 0.70 | 1.29 ± 0.89 | 1.07 ± 0.75 |
| Mean difference from control phase (95% CI) | 0.49 (−0.41, 1.39) | 0.27 (−0.47, 1.00) | |
| Maximum decrease (mmol l−1) | 2.47 ± 0.70 | 2.49 ± 0.47 | 2.18 ± 0.71 |
| Mean difference from control phase (95% CI) | 0.03 (−0.76, 0.81) | −0.28 (−1.18, 0.61) |
Data are mean values ± SD unless otherwise shown. AUC(0,3 h), area under curve from time zero to 3 h; AUC(0,7 h), area under curve from time zero to 7 h.
Discussion
The present study was conducted to investigate the effects of clarithromycin and grapefruit juice on the pharmacokinetics of glibenclamide. Clarithromycin moderately increased the AUC and Cmax of glibenclamide, but grapefruit juice had no significant effect on its pharmacokinetics. During the clarithromycin phase, the increase in glibenclamide AUC caused by clarithromycin varied from 10% to 68%. There were no significant differences in the pharmacodynamics of glibenclamide between the phases, probably partly due to the repeated food intake (for safety reasons) during the study days, which probably contributed to the increased variation in the blood glucose concentrations.
Glibenclamide is metabolized by CYP2C9 mainly to two hydroxylated metabolites (4-hydroxy and 3-hydroxy) that are excreted into bile and urine [2, 4, 28]. The hydroxyglibenclamide measured in the present study probably is the major metabolite, 4-hydroxyglibenclamide, which represents about 80% of glibeclamide metabolites excreted into urine. However, no attempt was made to identify the position of the hydroxyl group in the metabolite, i.e. to verify the specificity of analysis of hydroxyglibenclamide. Glibenclamide is both a substrate and inhibitor of P-glycoprotein in vitro [9]. In previous in vivo studies rifampicin has reduced and verapamil increased the plasma concentrations of glibenclamide [6, 29]. A recent study with human embryonic kidney cells, stably expressing OATP2B1, suggested that glibenclamide was also a substrate for this transporter expressed, for example, in the intestine and liver [7].
The increased Cmax and AUC(0,∞) and an unaltered elimination t1/2 of glibenclamide during the clarithromycin phase suggest that clarithromycin affected the pharmacokinetics of glibenclamide mainly during its absorption. Because clarithromycin inhibits P-glycoprotein, the present findings can be explained by a reduced activity of this efflux transporter in the intestinal wall. Furthermore, P-glycoprotein is also expressed in the biliary tract [30], and therefore, the clarithromycin-glibenclamide interaction may occur both in the intestinal wall and liver. However, it seems unlikely that clarithromycin would affect transport of glibenclamide or its metabolite in the kidney, because there were no significant changes in the t1/2 of glibenclamide or in the renal excretion of its metabolite. Because glibenclamide is metabolized mainly by CYP2C9 and clarithromycin does not inhibit CYP2C9 significantly in vivo [31], inhibition of CYP2C9 by clarithromycin seems an unlikely explanation for the observed interaction. However, CYP3A4 may play a minor role in the metabolism of glibenclamide [28] and therefore, inhibition of CYP3A4 could partly contribute to the present findings. For comparison, the same dose of 250 mg clarithromycin twice a day as used in the present study increased the AUC value of the CYP3A4 substrate midazolam by about three-fold [32].
Some in vitro studies suggest that grapefruit juice can inhibit P-glycoprotein, in addition to CYP3A4 [33, 34]. In one in vivo study grapefruit juice increased only slightly plasma concentrations of the P-glycoprotein substrate digoxin [35]. On the other hand, grapefruit juice, and also orange juice, can considerably reduce plasma concentrations of fexofenadine and celiprolol [17, 18, 36]; both of these drugs are P-glycoprotein substrates with negligible metabolism. The effect of fruit juices on fexofenadine has been explained by inhibition of the intestinal OATP1A2 resulting in a reduced absorption [15]. In the present study, grapefruit juice had no significant effect on the pharmacokinetics of the P-glycoprotein substrate glibenclamide, and a substrate for another uptake transporter, OATP2B1, which is ubiquitously expressed, for example, in the intestine [8]. To our knowledge this is the first study to evaluate the effect of grapefruit juice on the activity of OATP2B1 in vivo. The finding that grapefruit juice did not decrease the plasma concentrations of glibenclamide, suggests that either OATP2B1 plays only a minor role in the intestinal absorption of this sulphonylurea or that grapefruit juice is not a significant inhibitor of OATP2B1 in vivo.
In the present study, clarithromycin 250 mg twice daily did not significantly change the blood glucose-lowering effect of glibenclamide in healthy volunteers. Considering the elimination half-life of 3.3–4.9 h of clarithromycin, its plasma concentrations were at steady state by day 3 of its administration. In case reports, co-administration of clarithromycin 1000 mg day−1 with glibenclamide has caused severe hypoglycaemia in some patients [22, 23]. Although no controlled in vivo studies on the relationship between the clarithromycin dose and P-glycoprotein inhibition are available, it is possible that the ingestion of 1000 mg clarithromycin with glibenclamide results in a pharmacokinetic interaction, the magnitude of which is greater than that observed in this study [32, 37]. Furthermore, during repeated co-administration of clarithromycin and glibenclamide, the risk of hypoglycaemia caused by elevated glibenclamide concentrations will increase. Thus, an increase in glibenclamide concentrations caused by clarithromycin is the likely explanation for the reported severe hypoglycaemia. However, unlike under our controlled study conditions, the increased drug exposure is not necessarily counterbalanced by additional carbohydrate loading in patient drug use. Patients using a high dose of glibenclamide might be particularly susceptible to the clarithromycin-glibenclamide interaction with its clinical consequencies. Furthermore, in many diabetics and elderly patients, compromised renal function may impair the excretion of glibenclamide and its metabolites and increase the risk of hypoglycaemia.
In conclusion, clarithromycin moderately increased plasma concentrations of glibenclamide, but grapefruit juice did not have any significant effect on its pharmacokinetics. The mechanism of the clarithromycin-glibenclamide interaction may be inhibition of P-glycoprotein in the intestinal wall, with the possible contribution of inhibition of CYP3A4. This interaction could be of clinical significance, because elevated glibenclamide concentrations may increase the risk of hypoglycaemia. Concomitant use of clarithromycin with glibenclamide warrants close monitoring of blood glucose.
Acknowledgments
This study was supported by grants from the Helsinki University Central Hospital Research Fund and the Sigrid Juselius Foundation.
We thank Mrs Kerttu Mårtensson, Mrs Eija Mäkinen-Pulli, Mrs Lisbet Partanen, Mr Jouko Laitila, and Mr Mikko Neuvonen, MSc, for technical assistance and skilful determination of drug concentrations.
References
- 1.Neuvonen PJ, Kivistö KT. The effects of magnesium hydroxide on the absorption and efficacy of two glibenclamide preparations. Br J Clin Pharmacol. 1991;32:215–20. doi: 10.1111/j.1365-2125.1991.tb03884.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dollery C. Therapeutic drugs. 2. Edinburgh, UK: Churchill Livingstone; 1999. pp. G64–G69. [Google Scholar]
- 3.Niemi M, Cascorbi I, Timm R, Kroemer HK, Neuvonen PJ, Kivistö KT. Glyburide and glimepiride pharmacokinetics in subjects with different CYP2C9 genotypes. Clin Pharmacol Ther. 2002;72:326–32. doi: 10.1067/mcp.2002.127495. [DOI] [PubMed] [Google Scholar]
- 4.Kirchheiner J, Brockmöller J, Meineke I, Bauer S, Rohde W, Meisel C, Roots I. Impact of CYP2C9 amino acid polymorphisms on glyburide kinetics and on the insulin and glucose response in healthy volunteers. Clin Pharmacol Ther. 2002;71:286–96. doi: 10.1067/mcp.2002.122476. [DOI] [PubMed] [Google Scholar]
- 5.Stockley IH. Stockley's Drug Interactions. 6. United Kingdom: Pharmaceutical Press; 2002. p. 580. [Google Scholar]
- 6.Niemi M, Backman JT, Neuvonen M, Neuvonen PJ, Kivistö KT. Effects of rifampin on the pharmacokinetics and pharmacodynamics of glyburide and glipizide. Clin Pharmacol Ther. 2001;69:400–6. doi: 10.1067/mcp.2001.115822. [DOI] [PubMed] [Google Scholar]
- 7.Satoh H, Yamashita F, Tsujimoto M, Murakami H, Koyabu N, Ohtani H, Sawada Y. Citrus juices inhibit the function of human organic anion-transporting polypeptide OATP-B. Drug Metab Dispos. 2005;33:518–23. doi: 10.1124/dmd.104.002337. [DOI] [PubMed] [Google Scholar]
- 8.Kobayashi D, Nozawa T, Imai K, Nezu J, Tsuji A, Tamai I. Involvement of human organic anion transporting polypeptide OATP-B (SLC21A9) in pH-dependent transport across intestinal apical membrane. J Pharmacol Exp Ther. 2003;306:703–8. doi: 10.1124/jpet.103.051300. [DOI] [PubMed] [Google Scholar]
- 9.Goldstein PE, Boom A, van Geffel J, Jacobs P, Masereel B, Beauwens R. P-glycoprotein inhibition by glibenclamide and related compounds. Pflugers Arch. 1999;437:652–60. doi: 10.1007/s004240050829. [DOI] [PubMed] [Google Scholar]
- 10.Bailey DG, Spence JD, Munoz C, Arnold JMO. Interaction of citrus juices with felodipine and nifedipine. Lancet. 1991;337:268–9. doi: 10.1016/0140-6736(91)90872-m. [DOI] [PubMed] [Google Scholar]
- 11.Hukkinen SK, Varhe A, Olkkola KT, Neuvonen PJ. Plasma concentrations of triazolam are increased by concomitant ingestion of grapefruit juice. Clin Pharmacol Ther. 1995;58:127–31. doi: 10.1016/0009-9236(95)90188-4. [DOI] [PubMed] [Google Scholar]
- 12.Yee GC, Stanley DL, Pessa LJ, Dalla Costa T, Beltz SE, Ruiz J, Lowenthal DT. Effect of grapefruit juice on blood cyclosporin concentration. Lancet. 1995;345:955–6. doi: 10.1016/s0140-6736(95)90700-9. [DOI] [PubMed] [Google Scholar]
- 13.Kupferschmidt HHT, Fattinger KE, Ha HR, Follath F, Krahenbühl S. Interaction between grapefruit juice and midazolam in humans. Clin Pharmacol Ther. 1995;58:20–8. doi: 10.1016/0009-9236(95)90068-3. [DOI] [PubMed] [Google Scholar]
- 14.Kantola T, Kivistö KT, Neuvonen PJ. Grapefruit juice greatly increases serum concentrations of lovastatin and lovastatin acid. Clin Pharmacol Ther. 1998;63:397–402. doi: 10.1016/S0009-9236(98)90034-0. [DOI] [PubMed] [Google Scholar]
- 15.Lilja JJ, Kivistö KT, Neuvonen PJ. Grapefruit juice-simvastatin interaction: effect on serum concentrations of simvastatin, simvastatin acid, and HMG-CoA reductase inhibitors. Clin Pharmacol Ther. 1998;64:477–83. doi: 10.1016/S0009-9236(98)90130-8. [DOI] [PubMed] [Google Scholar]
- 16.Lown KS, Bailey DG, Fontana RJ, Janardan SK, Adair CH, Fortlage LA, Brown MB, Guo W, Watkins PB. Grapefruit juice increases felodipine oral availability in humans by decreasing intestinal CYP3A protein expression. J Clin Invest. 1997;99:2545–53. doi: 10.1172/JCI119439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dresser GK, Bailey DG, Leake BF, Schwarz UI, Dawson PA, Freeman DJ, Kim RB. Fruit juices inhibit organic anion transporting polypeptide-mediated drug uptake to decrease the oral availability of fexofenadine. Clin Pharmacol Ther. 2002;71:11–20. doi: 10.1067/mcp.2002.121152. [DOI] [PubMed] [Google Scholar]
- 18.Lilja JJ, Backman JT, Laitila J, Luurila H, Neuvonen PJ. Itraconazole increases but grapefruit juice greatly decreases plasma concentrations of celiprolol. Clin Pharmacol Ther. 2003;73:192–8. doi: 10.1067/mcp.2003.26. [DOI] [PubMed] [Google Scholar]
- 19.Schwarz UI, Seemann D, Oertel R, Miehlke S, Kuhlisch E, Fromm MF, Kim RB, Bailey DG, Kirch W. Grapefruit juice ingestion significantly reduces talinolol bioavailability. Clin Pharmacol Ther. 2005;77:291–301. doi: 10.1016/j.clpt.2004.11.111. [DOI] [PubMed] [Google Scholar]
- 20.Dresser GK, Kim RB, Bailey DG. Effect of grapefruit juice volume on the reduction of fexofenadine bioavailability: possible role of organic anion transporting polypeptides. Clin Pharmacol Ther. 2005;77:170–7. doi: 10.1016/j.clpt.2004.10.005. [DOI] [PubMed] [Google Scholar]
- 21.Rengelshausen J, Göggelmann C, Burhenne J, Riedel K-D, Ludwig J, Weiss J, Mikus G, Walter-Sack I, Haefeli WE. Contribution of increased oral bioavailability and reduced nonglomerular renal clearance of digoxin to the digoxin–clarithromycin interaction. Br J Clin Pharmacol. 2003;56:32–8. doi: 10.1046/j.1365-2125.2003.01824.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bussing R, Gende A. Severe hypoglycemia from clarithromycin–sulfonylurea drug interaction [letter] Diab Care. 2002;25:1659–61. doi: 10.2337/diacare.25.9.1659-a. [DOI] [PubMed] [Google Scholar]
- 23.Leiba A, Leibowitz A, Grossman E. An unusual case of hypoglycemia in a diabetic patient [letter] Ann Emerg Med. 2004;44:427–8. doi: 10.1016/j.annemergmed.2004.04.020. [DOI] [PubMed] [Google Scholar]
- 24.Lehr KH, Damm P. Simultaneous determination of the sulphonylurea glimepiride and its metabolites in human serum and urine by high-performance liquid chromatography after pre-column derivatization. J Chromatogr. 1990;526:497–505. doi: 10.1016/s0378-4347(00)82531-1. [DOI] [PubMed] [Google Scholar]
- 25.Zhang H, Henion J, Yang Y, Spooner N. Application of atmospheric pressure ionization time-of-flight mass spectrometry coupled with liquid chromatography for the characterization of in vitro drug metabolites. Anal Chem. 2000;72:3342–8. doi: 10.1021/ac000089r. [DOI] [PubMed] [Google Scholar]
- 26.Laakso S, Scheinin M, Anttila M. Determination of erythromycin base and 2′acetylerythromycin in human plasma using high-performance liquid chromatography with electrochemical detection. J Chromatogr. 1990;526:475–86. doi: 10.1016/s0378-4347(00)82529-3. [DOI] [PubMed] [Google Scholar]
- 27.van Rooyen GF, Smit MJ, de Jager AD, Hundt HKL, Swart KJ, Hundt AJ. Sensitive liquid chromatography-tandem mass spectrometry method for the determination of clarithromycin in human plasma. J Chromatogr. 2002;768:223–9. doi: 10.1016/s1570-0232(01)00566-9. [DOI] [PubMed] [Google Scholar]
- 28.Brian WR. Hypoglycemic agents. In: Levy RH, Thummel KE, Trager WF, Hansten PD, Eichelbaum M, editors. Metabolic Interactions. Philadelphia: Lippincott Williams & Wilkins; 2000. pp. 529–43. [Google Scholar]
- 29.Semple CG, Omile C, Buchanan KD, Beastall GH, Paterson KR. Effect of oral verapamil on glibenclamide stimulated insulin secretion. Br J Clin Pharmacol. 1986;22:187–90. doi: 10.1111/j.1365-2125.1986.tb05248.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Thiebaut F, Tsuruo T, Hamada H, Gottesman MM, Pastan I, Willingham MC. Cellular localization of the multidrug-resistance gene product P-glycoprotein in normal human tissues. Proc Natl Acad Sci USA. 1987;84:7735–8. doi: 10.1073/pnas.84.21.7735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bruce MA, Hall SD, Haehner-Daniels BD, Gorski JC. In vivo effect of clarithromycin on multiple cytochrome P450s. Drug Metab Dispos. 2001;29:1023–8. [PubMed] [Google Scholar]
- 32.Yeates RA, Laufen H, Zimmermann T. Interaction between midazolam and clarithromycin: comparison with azithromycin. Int J Clin Pharmacol Ther. 1996;34:400–5. [PubMed] [Google Scholar]
- 33.Eagling VA, Profit L, Back DJ. Inhibition of the CYP3A4-mediated metabolism and P-glycoprotein-mediated transport of the HIV-1 protease inhibitor saquinavir by grapefruit juice components. Br J Clin Pharmacol. 1999;48:543–52. doi: 10.1046/j.1365-2125.1999.00052.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Takanaga H, Ohnishi A, Matsuo H, Sawada Y. Inhibition of vinblastine efflux mediated by P-glycoprotein by grapefruit juice components in caco-2 cells. Biol Pharm Bull. 1998;21:1062–6. doi: 10.1248/bpb.21.1062. [DOI] [PubMed] [Google Scholar]
- 35.Becquemont L, Verstuyft C, Kerb R, Brinkmann U, Lebot M, Jaillon P, Funck-Brentano C. Effect of grapefruit juice on digoxin pharmacokinetics in humans. Clin Pharmacol Ther. 2001;70:311–6. [PubMed] [Google Scholar]
- 36.Lilja JJ, Juntti-Patinen L, Neuvonen PJ. Orange juice substantially reduces the bioavailability of the β-adrenergic-blocking agent celiprolol. Clin Pharmacol Ther. 2004;75:184–90. doi: 10.1016/j.clpt.2003.11.002. [DOI] [PubMed] [Google Scholar]
- 37.Gorski JC, Jones DR, Haehner-Daniels BD, Hamman MA, O'Mara EM, Hall SD. The contribution of intestinal and hepatic CYP3A to the interaction between midazolam and clarithromycin. Clin Pharmacol Ther. 1998;64:133–43. doi: 10.1016/S0009-9236(98)90146-1. [DOI] [PubMed] [Google Scholar]