Abstract
What is already known about this subject
Previous cross-sectional studies have demonstrated underuse of cardiovascular medicines in the population with diabetes.
What this study adds
Trends are changing over 5 years with increasing use of medicines affecting the angiotensin–renin system, lipid-lowering medicines and antiplatelets in the Australian veteran population, in line with recommended practice.
Aim
To determine trends over 5 years in cardiovascular medicine use in the Australian veteran population with diabetes
Methods
An observational study. All veterans dispensed medicines indicative of diabetes between 2000 and 2005 were identified from the Veterans Affairs pharmacy claims dataset. Concurrent dispensings of angiotensin-converting enzyme inhibitor (ACEI), lipid-lowering medicines and antiplatelets were assessed.
Results
ACEI/angiotensin II receptor blocker use has risen from 46% to 67% in the veteran population dispensed medicines indicative of diabetes. Lipid-lowering medicines have increased from 33% to 58% and antiplatelets from 28% to 50%.
Conclusion
The increasing use of cardiovascular medicines in the diabetes population is suggestive of improved treatment practices over time, consistent with guidelines and quality use of medicines initiatives.
Keywords: ACE inhibitors, antiplatelet, cardiovascular, diabetes, drug utilisation, lipid lowering therapy
Introduction
Cardiovascular disease is the leading cause of morbidity and mortality in patients with diabetes. Good glycaemic control, dietary and lifestyle interventions and modification of cardiovascular risk factors for people with Type 2 diabetes and microalbuminuria can reduce the risk ofcardiovascular events by about 50% [1]. Angiotensin-converting enzyme inhibitors (ACEIs) are advocated as first-line therapy in diabetes because of coexisting conditions, including microalbuminuria or proteinuria, previous myocardial infarction, left ventricular dysfunction and heart failure [2]. Low-dose aspirin is recommended for all patients with diabetes and established cardiovascular disease, or those aged ≥50 years, unless contraindicated [3]. Evidence also supports use of lipid-lowering medicines for both primary and secondary prevention of cardiovascular events [3].
Despite the evidence for efficacy of cardiovascular medicines in diabetes, this does not necessarily translate into clinical practice. The Australian Diabetes, Obesity and Lifestyle Study (AusDiab) has revealed that 36% of people with diabetes had lipids levels above target ranges and were not receiving treatment [4]. Further, 22.5% of people with diabetes had elevated blood pressure and were not receiving treatment [4]. Similar findings have been reported in other countries. A UK study reported 29% of diabetes patients required lipid-lowering medicines and nearly all of these were not on treatment, while only 47% of those considered hypertensive were on treatment [5]. A Canadian study has demonstrated that 17% of 392 persons with diabetes did not receive pharmacotherapy for hypertension, despite blood pressure above targets [6]. In addition, only 23% were regularly taking aspirin [7]. A US study reported that just over 50% of 54 855 veterans with diabetes with cholesterol above recommended treatment levels were not prescribed lipid-lowering medicines [8]. Another US study found 92% of diabetes patients had indications for ACEI/angiotensin II receptor blockers (A2RBs), yet only 43% received these medicines [9].
The AusDiab study was undertaken in 1999–2000. This study reports subsequent trends in cardiovascular medicine use in Australian veterans with diabetes.
Research design and methods
The Department of Veterans Affairs (DVA) Pharmacy Claims database contains details of all prescription medicines dispensed to veterans for which DVA pay a subsidy. The data file contains 75 million records for a treatment population of 320 000 veterans. The majority of the population is elderly, with 76% aged ≥70 years. The DVA maintain a client file, which includes data on gender, date of birth, date of death and family status. Medicines are coded in the dataset according to the World Health Organization anatomical and therapeutic chemical (ATC) classification [10].
The prevalent population with diabetes during 2000–2005 was defined each month as those people dispensed an oral diabetes medicine within the previous 35 days or insulin within 122 days. The time periods were calculated from the dataset and represent the number of days in which 75% of prescriptions are refilled for each respective drug group. No distinction between type of diabetes (type 1 or type 2) was made, as diagnostic data were not present in the dataset.
Having defined the diabetes prevalent population, the proportion using an ACEI or A2RB agent was defined each month, as those dispensed ACEI or A2RB in the previous 39 days. ACEI and A2RB medicines included all those in the ATC classification C09 [10] and the time period again represents the period in which 75% of prescriptions were refilled. The proportion using lipid-lowering medicines included those dispensed any medicine in the ATC classification C10 in the previous 44 days [10]. The proportion using antiplatelet medicines or warfarin included those with a dispensing of an antiplatelet in the previous 100 days or warfarin in the previous 42 days. The ATC classification B01AC was used for antiplatelets and B01AA for warfarin [10].
Poisson regression models were used to test for linear trend over time in monthly prescription rates. All analyses were undertaken using SAS v9.1 (SAS Inc., Cary, NC, USA).
Results
Just under 17 300 veterans (4.9%) were dispensed medicines indicated for diabetes in January 2000. This had risen to just over 23 500 (7.2%) by December 2005. During this time the overall eligible veteran population decreased from 350 000 to 325 000. The mean age at the beginning of the time period 1 January 2000 was 73.5 years (SD 8.4) and 67% were male and 33% female. At the end of the time period 1 December 2005, the mean age was higher at 77.6 years (SD 9.6) and 64% were male and 36% female.
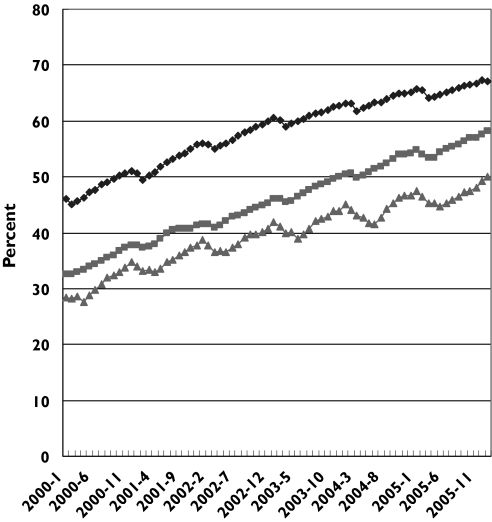
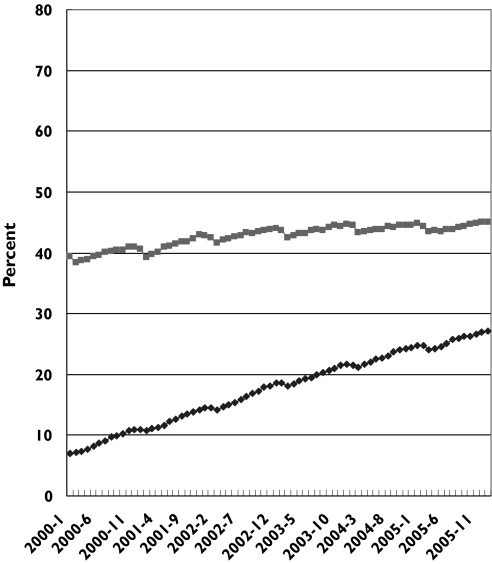
Trends in utilization of ACEI/A2RB show use has risen from 46% to 67% over the study period [slope of trend line = 0.0052; 95% confidence interval (CI) 0.0051, 0.0052, P < 0.0001] (Figure 1). Lipid-lowering medicines increased from 33% to 58% of the population (slope of trend line = 0.0080; 95% CI 0.0080, 0.0081, P < 0.0001) and antiplatelet use increased from 28% to 50% (slope of trend line = 0.0075; 95% CI 0.0074, 0.0076, P < 0.0001). The A2RBs accounted for the majority of the rise in angiotensin–renin system medicines (slope of trend line = 0.0087; 95% CI 0.0086, 0.0088, P < 0.0001) (Figure 2). The increase in lipid-lowering medicines was all attributable to statin use. Dispensing of other medicines in this class remained constant at just under 4% (slope of trend line = −0.0002; 95% CI −0.0005, 0.0001, P = 0.1337) (data not shown).
Figure 1.
Rate of veterans dispensed medicines indicative of diabetes who are concurrently dispensed cardiovascular medicines; 2000–2005. ACE/A2RB therapy (♦), lipid lowering therapy ( ), antiplatelet therapy (
), antiplatelet therapy ( )
)
Figure 2.
Rate of veterans dispensed medicines indicative of diabetes who are concurrently dispensed angiotensin-converting enzyme inhibitor (ACEI) ( ) or angiotensin II receptor blocker (A2RB) (♦) medicines; 2000–2005.
) or angiotensin II receptor blocker (A2RB) (♦) medicines; 2000–2005.
Discussion
Trends in dispensing of cardiovascular medicines among the veteran population dispensed medicines indicative of diabetes have increased by approximately 21% for ACEI/A2RBs, 25% for those on lipid-lowering medicines and 22% for those on antiplatelets. These trends are consistent with guidelines for practice [3] and earlier evidence of undertreatment in this population group [4]. The lower rate of utilization of antiplatelets needs to be interpreted cautiously as it is possible that veterans are buying aspirin over the counter rather than as a prescription medicine, so these medicines may be under-represented in the dataset.
Diabetes has been a national health priority area in Australia since 1996 and there is also a national strategy for quality use of medicines. Initiatives implemented under both programmes may have contributed to the observed effect. Australia's National Prescribing Service (NPS), an independent not-for-profit company, has run diabetes programmes in 2001 and 2005 [11]. There were also initiatives targeting hypertension in 1999, 2001 and 2003, dyslipidaemia in 2002 and antithrombotics in 2002, which all included diabetes as a consideration. The NPS programmes include mailed newsletters and prescriber feedback to all general practitioners (GPs) (∼ 20 000). In addition, 6600 GPs participated in the diabetes programme and approximately 4100 educational visits, 1500 clinical audits, 2900 case studies and 1400 group discussions were undertaken. Similar results were seen with hypertension, in which 6500 GPs participated, with approximately 5000 educational visits, 5100 clinical audits, 1600 case studies and 1350 small group discussions. Further, 1700 GPs participated in the dyslipidaemia programme [11]. The Department of Veterans Affairs also ran a patient-specific prescriber feedback programme which targeted ACE inhibitor use in diabetes in 2002 and 2005 [12].
National guidelines in Endocrinology were first released in 1997, with subsequent editions in 2001 and 2004 [3]. The National Health and Medical Research Council has also produced guidelines covering blood pressure, lipid management and macrovascular complications in diabetes in 2004 [13].
Finally, the Australian government committed funding of $43 million over 4 years to the National Integrated Diabetes Program [14]. This included funds for GPs to undertake annual diabetes care plans, of which 68 000 were undertaken in 2001/2002, rising to 140 850 in 2005/2006 [15]. Funding was also provided to divisions of general practice to establish diabetes registers.
The lack of clinical information within the dataset limits any conclusions about the appropriateness of therapy in the diabetes population. While the increasing rates of medication use are encouraging, treatment alone does not necessarily translate into outcomes. A previous Australian study (AusDiab) demonstrated that 30% of those with diabetes and on lipid-lowering medicines had lipid levels above target range [4] and 64% of those with diabetes and on antihypertensives had blood pressure readings above target range [4]. The percentage of people with diabetes currently untreated who may benefit from these therapies is also unknown. The AusDiab study, however, revealed that 69.3% of people with diabetes were hypertensive [16] and 71.8% were either on lipid-lowering medicines or had lipid levels above target ranges [4]. This suggests that the current level of use of cardiovascular medicine does not represent over-utilization. The data are likely to be representative of prescribing data. All medicines included were available as pharmaceutical benefits throughout the study and no major changes in access arrangements occurred.
The seasonal trend observed in the data is due to the safety net system which operates in Australia. Patient copayments are required, but there is a maximal contribution per calendar year after which medicines are provided free. As more patients reach the safety net, dispensing increases are observed, particularly in December, as copayments take effect again in the following January [17].
This study has demonstrated increased use of cardiovascular medicines in the veteran population with diabetes. These findings are in keeping with national guidelines and may indicate more appropriate therapy, as previous data had indicated underuse of these therapies in the diabetes population.
Acknowledgments
The Veterans' Medicines Advice and Therapeutics Education Service (Veterans' MATES) project team and this study were supported with funding from the Australian Government, Department of Veterans' Affairs, for the establishment of the Veterans' MATES.
References
- 1.Gaede P, Vedel P, Larsen N, Jensen GV, Parving HH, Pedersen O. Multifactorial intervention and cardiovascular disease in patients with type 2 diabetes. N Engl J Med. 2003;348:383–93. doi: 10.1056/NEJMoa021778. [DOI] [PubMed] [Google Scholar]
- 2.Australian Medicines Handbook Pty Ltd. Australian Medicines Handbook. Adelaide: Australian Medicines Handbook Pty Ltd; 2005. Available at http://www.amh.net.au/ (last accessed: 17 January 2007). [Google Scholar]
- 3.Therapeutic Guidelines Ltd. e-TG complete: North Melbourne: Therapeutic Guidelines Ltd. Available at http://www.tg.com.au/ (last accessed: 17 January 2007).
- 4.Kemp TM, Barr EL, Zimmet PZ, Cameron AJ, Welborn TA, Colagiuri S, Phillips P, Shaw JE. Glucose, lipid, and blood pressure control in Australian adults with type 2 diabetes: the 1999–2000 AusDiab. Diabetes Care. 2005;28:1490–2. doi: 10.2337/diacare.28.6.1490. [DOI] [PubMed] [Google Scholar]
- 5.Colhoun HM, Dong W, Barakat MT, Mather HM, Poulter NR. The scope for cardiovascular disease risk factor intervention among people with diabetes mellitus in England: a population-based analysis from the Health Surveys for England 1991–94. Diabet Med. 1999;16:35–40. doi: 10.1046/j.1464-5491.1999.00017.x. [DOI] [PubMed] [Google Scholar]
- 6.Supina AL, Guirguis LM, Majumdar SR, Lewanczuk RZ, Lee TK, Toth EL, Johnson JA. Treatment gaps for hypertension management in rural Canadian patients with type 2 diabetes mellitus. Clin Ther. 2004;26:598–606. doi: 10.1016/s0149-2918(04)90062-8. [DOI] [PubMed] [Google Scholar]
- 7.Klinke JA, Johnson JA, Guirguis LM, Toth EL, Lee TK, Lewanczuk RZ, Majumdar SR. Underuse of aspirin in type 2 diabetes mellitus: prevalence and correlates of therapy in rural Canada. Clin Ther. 2004;26:439–46. doi: 10.1016/s0149-2918(04)90040-9. [DOI] [PubMed] [Google Scholar]
- 8.Safford M, Eaton L, Hawley G, Brimacombe M, Rajan M, Li H, Pogach L. Disparities in use of lipid-lowering medications among people with type 2 diabetes mellitus. Arch Intern Med. 2003;163:922–8. doi: 10.1001/archinte.163.8.922. [DOI] [PubMed] [Google Scholar]
- 9.Rosen AB. Indications for and utilization of ACE inhibitors in older individuals with diabetes. Findings from the National Health and Nutrition Examination Survey 1999–2002. J Gen Intern Med. 2006;21:315–9. doi: 10.1111/j.1525-1497.2006.00351.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.World Health Organization Collaborating Centre for Drug Statistics Methodology. Anatomical Therapeutic Chemical Code Classification index with Defined Daily Doses. Oslo: WHO; 2004. Available at http://www.whocc.no/atcddd/ (last accessed: 5 October 2006). [Google Scholar]
- 11.National Prescribing Service. Surry Hills, NSW: National Prescribing Service; 2005. Evaluation Report no. 8. Progress, Achievements and Future Directions. Available at http://www.nps.org.au/resources/evaluation/report_08.pdf (last accessed: 5 October 2006). [Google Scholar]
- 12.Department of Veterans' Affairs. Veterans' MATES. Canberra: Department of Veterans Affairs; 2006. Available at http://www.dva.gov.au/health/veteransmates/index.htm (last accessed: 5 October 2006). [Google Scholar]
- 13.Australian Centre for Diabetes Strategies. National Evidence Based Guidelines for the Management of Type 2 Diabetes Mellitus. Canberra: National Health and Medical Research Council; 2004. Available at http://www.diabetesaustralia.com.au/education_info/nebg.html (last accessed: 5 October 2006). [Google Scholar]
- 14.Australian Government Department of Health and Ageing. Health Priorities. Canberra: Australian Government Department of Health and Ageing; 2006. Available at http://www.health.gov.au/internet/wcms/publishing.nsf/Content/Health+Priorities-1 (last accessed: 5 October 2006). [Google Scholar]
- 15.Medicare Australia. Medicare Benefits Schedule (MBS) Item Statistics Reports. Australian Government Medicare Australia, Canberra; 2006. Available at http://www.medicareaustralia.gov.au/providers/health_statistics/statistical_reporting/medicare.htm (last accessed: 5 October 2006). [Google Scholar]
- 16.Dunstan D, Zimmet P, Welborn T, Sicree R, Armstrong T, Atkins R, Cameron A, Shaw J, Chadban S. Diabesity and Associated Disorders in Australia 2000. Melbourne: International Diabetes Institute; 2001. [Google Scholar]
- 17.Donnelly N, McManus P, Dudley J, Hall W. Impact of increasing the re-supply interval on the seasonality of subsidised prescription use in Australia. Aust NZ J Public Health. 2000;24:603–6. doi: 10.1111/j.1467-842x.2000.tb00524.x. [DOI] [PubMed] [Google Scholar]