Abstract
Women may now have another effective, safe, and minimally invasive treatment option for treating fibroids
The patient
A 34 year old woman presented to her gynaecologist with menorrhagia associated with dysmenorrhoea and urinary frequency. She was nulliparous but had been trying to become pregnant for several years.
Learning points
Uterine artery embolisation is a safe and effective minimally invasive technique for treating symptomatic uterine fibroids
Recent NICE guidelines support its use as an alternative to myomectomy or hysterectomy in women with symptomatic fibroids larger than 3 cm who wish to preserve fertility
The risk of hysterectomy or repeat uterine artery embolisation for treatment failure is around 10% at one year and 20-25% within five years
The risk of hysterectomy for complications is 2.9% at 12 months
The risk of premature ovarian failure is around 1-2% in most series but increases with age; it can approach 25% in women over 45
What is the next investigation?
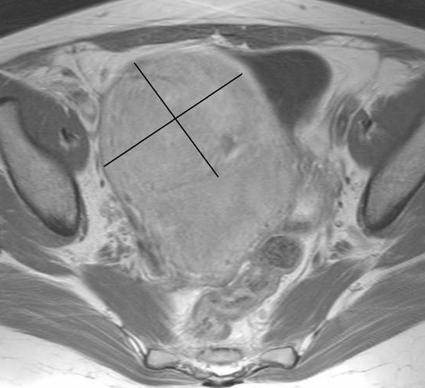
Transabdominal or transvaginal ultrasound is the most commonly performed imaging test for investigating menorrhagia with dysmenorrhoea or pressure related symptoms. If the results suggest uterine fibroids and uterine artery embolisation is a treatment option, we recommend magnetic resonance imaging with gadolinium (dimeglumine gadopentetate) enhancement (fig 1) because it has advantages before and after treatment (table).1 2 3
Fig 1 Gadolinium enhanced axial T1 weighted magnetic resonance imaging of the pelvis before embolisation. The uterus is enlarged, mainly as a result of a 14.2 cm intramural vascular fibroid, which shows pronounced enhancement
Comparison of pelvic ultrasound and magnetic resonance imaging (MRI) for uterine pathology
| Factor | Ultrasound | MRI |
|---|---|---|
| Cost | Relatively cheap | More expensive |
| Availability | Widely available | Limited resource |
| First line investigation | Yes1 | Problem solving1 |
| Uses ionising radiation | No | No |
| Sensitivity for all uterine pathologies | 48-100%1 | — |
| Specificity for all uterine pathologies | 12-100%1 | — |
| Diagnosis of pelvic pathologies other than fibroids | 89% sensitivity and specificity1 | 89% sensitivity and specificity1 |
| Fibroid size, position, and vascularity as a predictor of success | Poor2 | Excellent2 |
| For assessing complications (such as abscess or sloughed fibroid within endometrial cavity) | Poor2 3 | Excellent2 3 |
Outcome
Imaging confirmed the presence of an enlarged multilobulated fibroid uterus—the largest fibroid was intramural and measured 14.2 cm. Treatment options included:
Medical treatment (tranexemic acid with or without gonadotrophin analogue)
Mirena coil
Endometrial ablation techniques
Myomectomy
Hysterectomy
Uterine artery embolisation
Magnetic resonance guided focused ultrasound surgery.
Medical management had been tried unsuccessfully and endometrial ablative techniques were not considered appropriate because the fibroids were intramural. Magnetic resonance guided focused ultrasound surgery shows promise,1 but it is still a research tool with limited availability. The referring gynaecologist thought that the morphology of the fibroids made them unsuitable for myomectomy, and the patient was keen to avoid hysterectomy as she wanted to conceive in the future. Although current advice is that embolisation should be offered only to women who have completed their families,4 successful pregnancies have been reported after this procedure.2 The patient's concentrations of follicle stimulating hormone were at the upper limit of normal (7.5 IU/l).
After discussing all options with her gynaecologist and an interventional radiologist, the patient chose to undergo uterine artery embolisation, a treatment recommended in current National Institute for Health and Clinical Excellence (NICE) guidelines on heavy menstrual bleeding.3 She gave fully informed consent, and she accepted the risk of complications, including hysterectomy and fetal growth restriction.
We performed the procedure in the radiology vascular theatre using high quality imaging facilities, under antibiotic cover, and using oral diclofenac and intravenous morphine sulphate via a patient controlled analgesia pump.
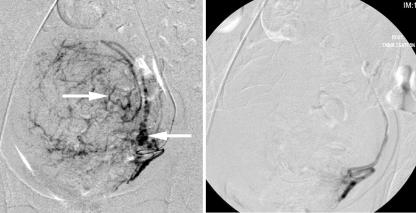
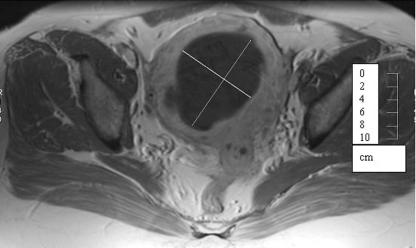
We used a unilateral femoral artery approach, and both uterine arteries were selectively catheterised (fig 2). The arteries were then embolised using three vials of 355-500 µm particle polyvinyl alcohol until stasis of contrast occurred (fig 2). The patient was sent home 24 hours after the procedure with oral diclofenac and tramadol as analgesia. Her symptoms improved (fig 3), and at one year follow-up her periods were normal and not painful.
Fig 2 Left: pre-embolisation angiography performed from the right groin via a selective catheter in the left uterine artery shows the typical vascular appearances of the hypertrophied arteries supplying the uterine fibroid (arrows). Right: angiography after embolisation with polyvinyl alcohol shows contrast stasis, with no distal flow to the fibroid
Fig 3 Gadolinium enhanced axial T1 weighted magnetic resonance imaging of the pelvis two months after the procedure. The fibroid is greatly reduced in size and is not contrast enhanced, as it is avascular
The patient became pregnant about 30 months after the procedure. At 34 weeks she had a lower segment caesarean section because of hypertension and intrauterine growth retardation secondary to oligohydramnios. A 2.1 kg baby boy was born; he had respiratory distress syndrome in the first week, but this quickly resolved.
Currently, the boy is 12 months old, in good health and developmentally normal apart from sensorineural deafness of uncertain cause. The mother is asymptomatic with normal light periods.
Uterine artery embolisation
Uterine artery embolisation is an image guided technique that reduces the blood supply to uterine fibroids, which makes them shrink and become asymptomatic. A small catheter is introduced, usually via the common femoral artery under local anaesthesia. The catheter is manipulated into the uterine arteries on both sides using x ray guidance, and an embolic agent is injected to occlude them. This technique has been performed more than 100 000 times worldwide since it was first described in 1995.5 Operator experience is important, and most major centres in the United Kingdom have trained radiologists who provide this service. Recently published guidelines support the use of this technique as an alternative to myomectomy and hysterectomy in women with symptomatic fibroids greater than 3 cm in size (box).3
Indications and contraindications for uterine artery embolisation3 5 6 7 8 9 10 11
Accepted indications (strong evidence base)
Menorrhagia
Dysmenorrhoea
Pressure symptoms including abdominal bloating, frequency, nocturia, and constipation
Controversial indications (weak evidence base)
Asymptomatic patients
Failure to conceive and all other treatments for fibroids have failed or are not indicated
Adenomyosis
Contraindications
Subserosal and submucosal fibroids on a narrow stalk are a relative contraindication because they could detach after infarction and lie free in the retroperitoneum or uterine cavity, where they might become infected. Although no evidence exists to support this hypothesis, it seems sensible to avoid the procedure for such fibroids
The desire to avoid hysterectomy under any circumstances is an absolute contraindication as there is a small risk of hysterectomy as a result of uterine sepsis or uncontrolled pain after the procedure (2.9% at 12 months)7 10
Benefits
Around 80-90% of patients will be asymptomatic or have significantly improved symptoms at one year, with an associated 40-75% reduction in fibroid volume. Recent studies support good outcomes at five years. However, 20-25% of patients will need further treatment, including repeat embolisation or surgery (myomectomy or hysterectomy) within five years.7 8 10
Patients usually have a shorter stay in hospital (24 hours), faster recovery and return to work (seven to 10 days), and lower rate of major morbidity (such as damage to the bowel or bladder) than those who have a hysterectomy or myomectomy; minor complication rates are similar.7 8 10 In addition, patients who want to conceive in the future or who have no other conservative treatment option can retain their uterus.
Economic modelling indicates that uterine artery embolisation is a cost effective treatment with significant savings over open surgery at one year.8 Quality adjusted life year scores increase with the desire for pregnancy and the age of the patient, and older patients are less likely to need reintervention.2
Adverse effects
Most patients have pain of varying severity, which can usually be controlled by analgesia. Postembolisation syndrome occurs in up to 52% of patients.8 This constitutes a general malaise, with mild pyrexia and flu-like symptoms, which is self limiting and usually lasts for seven to 10 days.
A persistent non-offensive discharge (negative on bacterial culture) occurs in 7-14% of cases. It may be more common with submucosal fibroids.6 7 8 10
The risk of hysterectomy and or repeat uterine artery embolisation for treatment failure is around 10% at one year and rises to 20-25% within five years.7 8 There is also a 2.9% risk of hysterectomy within 12 months as a result of uterine sepsis or uncontrolled pain.3 7
The risk of premature ovarian failure is around 1-2% in most series. However, this risk increases with age, and it can be as high as 25% in women over 45.7 If the patient becomes pregnant, there is a theoretical risk of uterine rupture or intrauterine growth retardation. The miscarriage rate is also 40-70% higher than in an age matched population.2 7 Late expulsion of a fibroid can also occur in 2.2-7.7% of cases.6 7 8
The risk related to radiation is small. Operators are encouraged to use pulsed fluoroscopy and minimise angiographic runs to keep the dose of radiation low. Studies have shown that skin injuries are unlikely, ovarian doses are below the threshold for permanent or temporary sterility, and that the stochastic risk for radiation induced cancer and genetic injury to future children is not substantial.11
Questions for further research
Despite the successful pregnancy in this case, it is unclear what advice to give patients about future pregnancy. Many successful pregnancies have been reported, but rates of miscarriage, caesarean section, and preterm delivery are higher than in age matched women without fibroids. A randomised trial comparing uterine artery embolisation and myomectomy with pregnancy outcome as the primary endpoint would be valuable, as would more research into the effect of uterine artery embolisation on ovarian function and long term fertility.
Many technical problems are yet to be resolved, including the ideal embolic agent, the efficacy of single dose antibiotics, and patient selection as an indicator of success. In addition, NICE has called for further research into the psychosexual impact of uterine artery embolisation and myomectomy, the effect of uterine artery embolisation on uterine blood flow, and how uterine artery embolisation reduces heavy menstrual bleeding.
Contributors: AW and AN wrote the article jointly. AW is guarantor.
Funding: None.
Competing interests: AW is a clinical adviser to Biocompatibles Ltd.
Provenance and peer review: Commissioned; externally peer reviewed.
This series provides an update on the best use of different imaging methods for common or important clinical presentations. The series editors are Fergus Gleeson, consultant radiologist, Churchill Hospital, Oxford, and Kamini Patel, consultant radiologist, Homerton University Hospital, London
References
- 1.Stewart EA, Rabinovici J, Tempany CM, Inbar Y, Regan L, Gostout B, et al. Clinical outcomes of focused ultrasound surgery for the treatment of uterine fibroids. Fertil Steril 2006;85:22-9. [DOI] [PubMed] [Google Scholar]
- 2.Mara M, Fucikova Z, Maskova J, Kuzel D, Haakova L. Uterine fibroid embolization versus myomectomy in women wishing to preserve fertility: preliminary results of a randomized controlled trial. Eur J Obstet Gynecol Reprod Biol 2006;126:226-33. [DOI] [PubMed] [Google Scholar]
- 3.National Institute for Health and Clinical Excellence. Heavy menstrual bleeding. NICE guideline CG44. London: NICE, 2007. http://guidance.nice.org.uk/CG44/guidance/pdf/English
- 4.Royal College of Obstetricians and Gynaecologists/Royal College of Radiologists. Clinical recommendations on the use of uterine artery embolisation in the management of fibroids. Report of a joint working party, 2000. www.rcr.ac.uk/docs/radiology/pdf/embolisation.pdf
- 5.Ravina JH, Merland JJ, Ciraru-Vigneron N, Bouret JM, Herbreteau D, Houdart E, et al. Arterial embolization: a new treatment of menorrhagia in uterine fibroma. Presse Med 1995;24:1754. [PubMed] [Google Scholar]
- 6.Walker WJ, Pelage JP. Uterine artery embolisation for symptomatic fibroids: clinical results in 400 women with imaging follow up. BJOG 2003;110:1139. [DOI] [PubMed] [Google Scholar]
- 7.Spies JB, Myers ER, Worthington-Kirsch R, Mulgund J, Goodwin S, Mauro M; Fibroid Registry Investigators. The FIBROID registry: symptom and quality-of-life status 1 year after therapy. Obstet Gynecol 2005;106:1309-18. [DOI] [PubMed] [Google Scholar]
- 8.Edwards RD, Moss JG, Lumsden MA, Wu O, Murray LS, Twaddle S, et al; Committee of the Randomised Trial of Embolisation versus Surgical Treatment of Fibroids. Uterine artery embolisation versus surgery for symptomatic fibroids. N Engl J Med 2007;356:360-70. [DOI] [PubMed] [Google Scholar]
- 9.Gupta JK, Sinha AS, Lumsden MA, Hickey M. Uterine artery embolisation for symptomatic fibroids. Cochrane Database Syst Rev 2006;(1):CD005073. [DOI] [PubMed]
- 10.Hehenkamp WJ, Volkers NA, Donderwinkel PF, de Blok S, Birnie E, Ankum WM, et al. Uterine artery embolisation versus hysterectomy in the treatment of symptomatic fibroids (EMMY trial): peri- and post-procedural results from a randomised controlled trial. Am J Obstet Gynecol 2005;193:1618-29. [DOI] [PubMed] [Google Scholar]
- 11.Glomset O, Hellesnes J, Heimland N, Hafsahl G, Smith HJ. Assessment of organ radiation dose associated with uterine artery embolisation. Acta Radiol 2006;47:179-85. [DOI] [PubMed] [Google Scholar]