Abstract
Angiomyolipoma (AML) is a rare benign neoplasm that usually arises in the kidneys, but may rarely originate in sites such as the retroperitoneum, liver and bone. It is characterised by an intimate admixture of blood vessels, smooth muscle and fat. This multiphasic composition allows for its recognition on ultrasound and CT scan examination. Metastases are exceedingly uncommon, and only one other case of metastatic extrarenal AML exists in the literature. Histological variants of AML such as epithelioid angiomyolipoma (EAML) are considered to be locally aggressive. A unique case of an EAML of the retroperitoneum that metastasised to the liver and bone in an 80‐year‐old woman is described.
Angiomyolipoma (AML) is a rare, complex mesenchymal tumour, characterised by proliferation of blood vessels, smooth muscle and adipose tissue elements. It is considered a benign neoplasm, even though it may exhibit atypical histological features, involve regional lymph nodes and be multifocal.1,2,3,4,5 Recently, an epithelioid variant of AML (EAML) has been described, and is thought to be more aggressive. We describe an EAML of the retroperitoneum that metastasised to the liver and bone, and present a literature review.
Case report
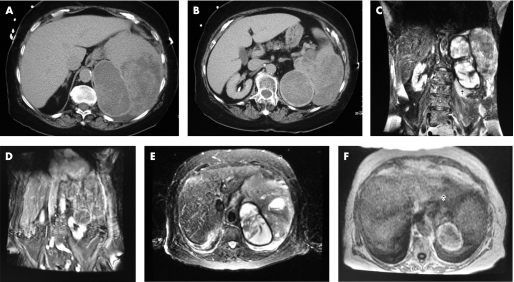
An 80‐year‐old Caucasian woman presented with progressively increasing abdominal pain. She was taking coumadin for a remote history of deep vein thrombosis. Physical examination was only significant for low‐grade fever (98.8°F). Laboratory investigations were significant for anaemia (haemoglobin 9.2 g/l), increased prothrombin time (24.1 s), increased international normalised ratio (3.9) and creatinine of 1.6 mg/dl. A CT scan of the abdomen showed a 16 cm, irregularly enhancing and hypodense mass located in the retroperitoneum, abutting the kidney (fig 1A,B). There was no significant adenopathy and no invasion of the renal artery or vein. These findings were suspicious for a renal cell carcinoma with haemorrhage in the tumour mass. An MRI scan showed a 15 cm complex mass with peripheral enhancement, depressing the left kidney inferiorly and medially (fig 1C,D). The marked inhomogenity within the mass suggested necrosis and cystic degeneration (fig 1C–F). The patient underwent en bloc resection of the large cystic mass, left kidney, spleen and portion of the left adrenal gland, diaphragm and perirenal fat.
Figure 1 Radiographic evaluation revealed a complex, irregular mass with cystic degeneration and haemorrhage, closely approximating the left kidney and adrenal. (A, B) CT scan of the abdomen showing a 16 cm, irregularly enhancing and hypodence mass located in the retroperitoneum, abutting the kidney; (C, D) MR showing a 15 cm complex mass with peripheral enhancement, depressing the left kidney inferiorly and medially. (C–F) Marked inhomogeneity within the mass suggests necrosis and cystic degeneration.
Pathology
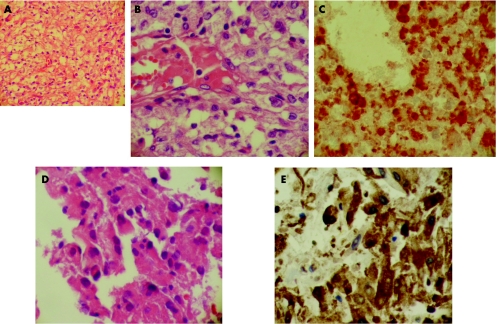
Grossly and microscopically, there was no evidence of malignancy involving the kidney, spleen and adrenals. A perirenal mass was identified, with cystic areas containing dilated vascular spaces intermingled with necrotic tissue, alternating with more solid, better‐preserved areas in which the cells were spindled with elongated and hyperchromatic nuclei (fig 2A,B). The cells were positive for human melanoma black (HMB)‐45 (fig 2C) and focally for smooth muscle actin. Chromogranin, synaptophysin, epithelial membrane antigen, vimentin, carcinoembryonic antigen, S100, desmin, CD45, CD20 and cytokeratin were all negative. A provisional diagnosis of EAML with atypical features arising in the retroperitoneum was made. Since the patient did not have tuberous sclerosis and a primary retroperitoneal AML is rare, the case was sent in for consultation to a soft‐tissue expert who concurred with our diagnosis.
Figure 2 (A) The primary retroperitoneal tumour contains a monotonous proliferation of epithelioid cells (100×). (B) The cells have atypical morphology (400×). (C) They stain positively for human melanoma black (HMB)‐45 immunohistochemical stain. (D) Liver metastasis contains cells with similar morphology (400×) and the cells are again positive for HMB‐45 (E).
Clinical course
The tumour was completely removed at surgery. The patient was followed at regular intervals on an outpatient basis. An ultrasound examination 1 year later revealed a 5.3 cm liver lesion (fig 3A). The liver also had two additional nodules, 2.6 and 2.3 cm, respectively. A CT scan showed similar findings (fig 3B,C). A CT‐guided biopsy of the liver lesion was performed that contained a neoplasm with extensive areas of necrosis, and focally consisted of epithelioid to spindle cells with pleomorphic, hyperchromatic nuclei, similar in appearance to the original retroperitoneal tumour (fig 2D). HMB‐45 was again positive (fig 2E). This was consistent with liver metastasis of the retroperitoneal EAML. The case was again sent in for consultation to a soft‐tissue expert who concurred with our diagnosis. A nuclear bone scan was performed to evaluate the extent of disease and demonstrated increased uptake in the anterior portion of the ribs on the left side (fig 3D).
Figure 3 Abdominal ultrasound (A) and CT scan (B,C) demonstrate liver mass. A positron emission tomography scan shows increased uptake in the ribs on the left side (D).
Discussion
AML may occur sporadically or in those affected by tuberous sclerosis. In all, 40% of patients with AML have tuberous sclerosis and up to 80% of patients with tuberous sclerosis have AMLs. They occur most commonly in the kidney. Even in this location, they are rare, comprising 0.3% of all renal neoplasms.1 Before a diagnosis of extrarenal AML is rendered, a renal primary with capsular rupture should be excluded. Both renal and extrarenal AMLs have a tendency to bleed owing to the rich vascular network. Most extrarenal AMLs reported in the literature presented with haemorrhage and shock, requiring blood transfusions and emergency intervention.
Although AMLs may demonstrate the primary involvement of multiple organs, malignant behaviour characterised by metastasis to distant organs is a rare occurrence. Only a single case of metastasis of extrarenal AML has been reported, whereas metastasis from renal AMLs has been described from both monotypic and conventional types.1,3,6 The age range of these patients was wide, from 21 to 72 years. The lungs and liver were the common sites of metastasis. Survival is reported to range from 3 months to 10 years. The only reported case of metastatic retroperitoneal AML is that of a 29‐year‐old man with tuberous sclerosis complex. It metastasised to the liver after 9 years of initial diagnosis, and to the mediastinum after 17 years. The patient is reported to be disease free 20 months after the last surgery (approximately 19 years after the first diagnosis). Our patient is the second reported case of metastatic retroperitoneal AML, and with metastasis to the bone and liver.
EAML is characterised by the predominance of epithelioid cells, with eosinophilic cytoplasm and prominent nucleoli. Fat, smooth muscle and vascular elements are generally inconspicuous, and such tumours may be referred to as monotypic EAML.1,3,4,5 The diagnosis is supported by positive immunostaining with HMB‐45. Like typical AMLs, the epithelioid variant generally exhibits benign clinical behaviour, even in the presence of atypical morphology.1,5,7,8 Monotypic variants have been described in the kidney,7,9 liver8 and bone.10
Take‐home messages
Angiomyolipoma (AML) is generally a benign tumour that usually arises in or around the kidneys.
The epithelioid variant may not be diagnosed on imaging studies, leading to an erroneous diagnosis of malignancy and undesirable aggressive surgical intervention.
Although this is only the second reported case of malignant retroperitoneal epithelioid AML, it does highlight the variable clinical course of these tumours. There are no reported histological features that predict the aggressive behaviour of these tumours.
The cell of origin of EAML is considered to be a perivascular epithelioid cell (PEC), which is characterised by immunoreactivity for HMB‐45.1 Other tumours derived from PECs include lymphangiomyomatosis, clear cell tumours of various organs, clear cell myomelanocytic tumours and abdominal pelvic sarcomas of PECs.1 There does not seem to be any histological finding that predicts malignant behaviour in AMLs. The presence of mitotic activity in the epithelioid areas is a feature common to many of the reported cases of metastatic AML6; however, it is often observed in otherwise benign EAMLs.5 The clinical course remains variable and cannot be predicted based on histology.
The presence of fat density and aneurysm‐like vascular markings of renal AML are characteristic findings that allow its diagnosis by ultrasonography and CT scan.4 Extrarenal AMLs, especially epithelioid types, may not be diagnosed on imaging, as they often lack fat densities. Enhancement of the mass on contrast CT scans may erroneously be interpreted as metastasis or locally advanced renal carcinoma.4,5 Extrarenal tumours are often found adjacent to the kidneys and this proximity may also lead to a diagnosis of a primary kidney neoplasm. The high incidence of haemorrhage into these tumours may be misinterpreted as perinephric haematoma. Another radiological differential in larger retroperitoneal tumours is liposarcoma. The latter usually arises outside Gerota's fascia, whereas the former are mostly found within the perinephric adipose tissue.4
In conclusion, a high index of suspicion for AML in tumours arising in the perinephric fat may help prevent unnecessary nephrectomies. Percutaneous CT‐guided biopsy in tumours without excess haemorrhage may help in diagnosis. In those with extensive haemorrhage, cautious exploration may result in renal‐sparing surgery. Intraoperative frozen section is unlikely to be helpful, especially in EAMLs.
Abbreviations
AML - angiomyolipoma
EAML - epithelioid angiomyolipoma
HMB - human meloma black
PEC - perivascular epithelioid cell
Footnotes
Competing interests: None declared.
References
- 1.Lau S K, Marchevsky A M, Mckenna R J., Jret al Malignant monotypic epitheloid angiomyolipoma of the retoperitoneum. Int J Surg Pathol 200311223–228. [DOI] [PubMed] [Google Scholar]
- 2.Hruban R H, Bhagavan B S, Epstein J L. Massive retroperitoneal angiomyolipoma: a lesion that may be confused with well differentiated liposarcoma. Am J Clin Pathol 198992805–808. [DOI] [PubMed] [Google Scholar]
- 3.Yokoo H, Isoda K, Nakazato Y.et al Retroperitoneal epitheloid angiomyolipoma leading to fatal outcome. Pathol Int 200050649–654. [DOI] [PubMed] [Google Scholar]
- 4.Mansi M K, Al‐Khudair W K, Al‐bqami N M.et al Extrarenal retroperitoneal angiomyolipoma. Saudi Med J 2002231124–1126. [PubMed] [Google Scholar]
- 5.Fegan J E, Shah H R, Mukunyadzi P.et al Extrarenal retroperitoneal angiomyolipoma. South Med J 19979059–62. [DOI] [PubMed] [Google Scholar]
- 6.Al‐Saleem T, Wessner L L, Scheithauer B W.et al Malignant tumors of the kidney, brain and soft tissues in children and young adults with tuberous sclerosis complex. Cancer 1998832208–2216. [PubMed] [Google Scholar]
- 7.Martignoni G, Pea M, Bonetti F.et al Carcinoma‐like monotypic epitheloid angiomyolipoma in patients without evidence tuberous sclerosis: a clinicopathologic and genetic study. Am J Surg Pathol 199822663–672. [DOI] [PubMed] [Google Scholar]
- 8.Yamasaki S, Tanaka S, Fujii H.et al Monotypic epitheloid angiomyolipoma of the liver. Histopathology 200036451–456. [DOI] [PubMed] [Google Scholar]
- 9.Pea M, Bonetti F, Martignoni G. Apparent renal cell carcinomas in tuberous sclerosis are heterogenous: the identification of malignant epitheloid angiomyolipoma. Am J Surg Pathol 199822180–187. [DOI] [PubMed] [Google Scholar]
- 10.Insabato L, DeRosa G, Terraciano L M.et al Primary monotypic epithelioid angiomyolipoma of the bone. Histopathology 200240286–290. [DOI] [PubMed] [Google Scholar]