Abstract
The study investigated the routine introduction of a new surgical consent form containing a tissue consent section to investigate patient attitudes to the use of surplus tissue for research (after the Alder Hey inquiry) and also the differing approaches by consent takers. All surgical consent forms received in histopathology for the same 2‐month period in 2 consecutive years were analysed, recording available information about the specimen, the tissue consent section and, for the second year, the consent taker. The findings showed that <5% of patients whose views were recorded disagreed with the use of their tissue for research. They also showed that the number of completed forms sent to histopathology had increased but the pattern of completion had changed very little. A wide variation between departments and also between clinicians was apparent in the levels of completion of the tissue consent section, suggesting wide variability in the quality of the consenting process. When asked, patients rarely object (<5%) but if the highest standards of consent for surgical tissue are to be achieved and the wishes of patients to donate tissue are to be effectively recorded then new resources or approaches will be needed for this process.
The study of diseased human tissues has underpinned many significant medical advances. Its use in research is fundamental to scientific progress and the relief of human suffering, as well as possibly reducing the need for animal models. The debate surrounding the retention of autopsy tissues has led to the issuing of numerous guidelines by a number of bodies (eg, Department of Health,1 Royal College of Pathologists,2 British Medical Association,3 General Medical Council4 and so on) as well as new legislation in the form of the Human Tissue Act 2004.5 This study examines the practicality of one of the key features of these recommendations: the feasibility of obtaining informed consent in a teaching hospital in the absence of specific resources from the National Health Service (NHS).
In November 2001, the Department of Health published Good practice in consent implementation guide: consent to examination or treatment.6 In this, trusts were instructed that “patients should be given the opportunity to refuse permission for tissue taken during surgery or other purposes to be used for education or research purposes”. The policy also stated that the system for doing this “must be well‐publicised and transparent, making provision for patients to record their consent or objection to the use of such tissue and for this to be notified to the laboratory”. Likewise, for public health monitoring, although explicit consent is not deemed necessary, trusts are to apply “a well publicised opt‐out policy”.
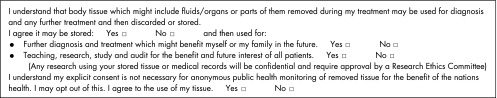
The Leeds Teaching Hospitals NHS Trust is the largest in the UK and has a histopathology department with a high volume turnover, approximately 46 000 histology requests per annum. The Trust received over 900 organ retention enquiries from 1999 to 2004, and adverse publicity from the fall‐out of the Alder Hey7 and Bristol8 enquiries. As a major regional cancer centre, Cancer Research UK Clinical Research centre and a National Translational Cancer Research Network centre, it has considerable cancer research interests requiring access to human tissue. The Trust was also aware that the proposed Human Tissue Bill might make written tissue consent mandatory. It was decided the most effective way to adhere strictly to the new policy, and to ensure that consented tissue was available, was to incorporate a specific tissue consent section into the standard consent forms (fig 1).
Figure 1 Incorporation of specific tissue consent into standard consent forms.
Apart from the reprinting of consent forms, this has not been resourced by the Trust. The attitude of patients to the use of their surgically removed tissues has not been widely investigated. One study9 comparing patients' opinions with those in the 1996 Nuffield Council on Bioethics report10 on ownership of tissue showed that 85% of patients were happy for their tissue to be used in research and related activities. The Leeds Study provided the opportunity to explore further the altruism of patients undergoing operations in the NHS.
The new consent forms came into use in the Trust in September 2002. The Trust policy states “that one copy of the completed consent form should be attached to the Histology request form and accompany the specimen to the laboratory”.9
The feasibility of this policy has been controversial so we have evaluated this in routine practice in a major teaching hospital. Furthermore, where appropriate, the differing approaches to consent have been explored.
Methods
Two audits of surgical consent forms were performed on all forms received in the Trust's histopathology department, with corresponding histology request forms for the period October–November 2002 and October–November 2003. The latter was undertaken to gauge whether compliance had improved with familiarity and to set a baseline before interventions by the tissue bank nurse (employed within histopathology to assist with collection of tissue for research).
The original audit recorded laboratory site, specimen and department, and the wishes of the patient were documented. In the 2003 audit, the status of the consent taker was also included to allow more detailed analysis and the possibility for further targeted education.
Results
In October–November 2002, 6707 histology requests were received, 3405 (51%) accompanied by consent forms (table 1). In the same period in 2003, 6744 requests arrived, 4770 (71%) of them with consent forms. This was an increase of 20%.
Table 1 Histology requests accompanied by consent forms .
| Year | Histology requests | Consent forms received | Requests with consent forms (%) |
|---|---|---|---|
| 2002 | 6707 | 3405 | 51 |
| 2003 | 6744 | 4770 | 71 |
In 2002, 1878 (55%) of forms received had fully completed tissue sections, and 1239 (36%) of tissue sections were blank (table 2). The figures in 2003 were little changed, with 2710 (57%) fully complete and 1631 (34%) blank, and the remaining forms were partially completed.
Table 2 Number of forms received in 2002 compared with 2003.
| Year | Total number of forms | Completed forms, n (%) | Blank forms, n (%) | Partially completed forms, n (%) |
|---|---|---|---|---|
| 2002 (Oct–Nov) | 3405 | 1878 (55) | 1239 (36) | 288 (9) |
| 2003 (Oct–Nov) | 4770 | 2710 (57) | 1631 (34) | 429 (9) |
The views of the patients about the use of tissue for research and education varied little between the two audits. In 2002, 5% of patients declined (103/2058 forms in which the patients' wishes were recorded) and in 2003, 4% declined (133/3013 likewise); table 3). The figures for public health monitoring improved from 10% opt‐out in 2002 to 4% in 2003.
Table 3 Percentage of patients declined in years 2002 and 2003.
| Year | Oct–Nov2002 | Oct–Nov 2003 |
|---|---|---|
| Total number of consent forms received | 3405 | 4770 |
| Teaching/research sections completed | 2058 | 3013 |
| Teaching/research agree | 1955 | 2880 |
| Teaching/research disagree | 103 | 133 |
| Public health monitoring sections completed | 1921 | 2798 |
| Public health monitoring agree | 1728 | 2696 |
| Public health monitoring disagree | 193 | 102 |
Completion
A wide variation in the standards of completion of the tissue consent sections was found, both between departments and between consent takers (table 4).
Table 4 Wide variation in the standards of completion of the tissue consent sections found both between departments and between consent takers.
| Department | Consent forms received | Forms fully completed (%) |
|---|---|---|
| Anaesthetics | 37 | 100 |
| Cardiothoracic surgery | 56 | 9 |
| Dermatology | 606 | 81 |
| Ear, nose and throat | 124 | 60 |
| Gastroenterology | 1449 | 60 |
| General surgery | 787 | 44 |
| Genitourinary Medicine | 22 | 95 |
| MaxFac/dental | 125 | 34 |
| Neurology/neurosurgery | 54 | 78 |
| Obs and gynae | 677 | 67 |
| Oncology | 19 | 68 |
| Ophthalmology | 20 | 45 |
| Orthopaedics | 25 | 4 |
| Paediatrics | 150 | 67 |
| Plastic surgery | 250 | 32 |
| Radiology | 46 | 35 |
| Respiratory medicine | 45 | 20 |
| Rheumatology | 2 | 0 |
| Urology | 269 | 35 |
| Vascular surgery | 7 | 0 |
MaxFac, maxillofacial; Obs and Gynae, obstetrics and gynaecology.
There did not seem to be any relationship between the number of forms and the standard of completion. The fully completed tissue sections varied between 44% and 81% in the high‐volume departments. In the smaller‐volume areas, completion varied between 20% and 100%, the latter being anaesthetics. In this department, many of the forms relate to malignant hyperthermia biopsies, and consent is taken by the pathologists performing the biopsies.
The variations between consent takers were marked, (table 5). The variations were analysed in the three departments within the Trust where nurse practitioners take consent for the procedures they perform.
Table 5 Analysis of completed forms in 2003 where consent taker recorded.
| Consent taker | Fully completed forms, n (%) | Blank forms, n (%) | Partially completed forms, n (%) | Total |
|---|---|---|---|---|
| Consultant | 508 (60) | 241 (29) | 95 (11) | 844 |
| Specialist registrar | 688 (55) | 465 (37) | 107 (8) | 1260 |
| Senior house officer | 374 (41) | 458 (51) | 73 (8) | 905 |
| Other clinician | 480 (61) | 249 (32) | 61 (8) | 790 |
| Nurse | 421 (89) | 21 (4) | 29 (6) | 471 |
| Grand total | 2471 (58) | 1434 (34) | 365 (8) | 4270 |
The poorest performers were senior house officers, with 458 (51%) blank tissue sections and only 374 of 905 (41%) completely filled forms. The nurses performed the best, with 421 of 471 (89%) fully complete and only 21(4%) blank tissue sections. Consultants and other clinicians such as research registrars, staff grades or general practitioners performed about the same, with approximately 60% fully complete and 30% blank.
As the audit was undertaken certain anomalies emerged. Forms completed by one particular clinician always had “no” ticked to each tissue consent box.
The same operations consented by other clinicians in this area rarely showed any patients declining. If these outliers are removed from the audit, the tissue rejection rate for that department drops from 31% to 4%.
In another department, one clinician's patients always seemed to decline the use of tissue for everything except public health monitoring. This was true for 27 of 30 forms completed by this clinician. Again, if these outliers are removed, the research rejection for that department falls from 5% to 1%.
A wide variation was seen between departments in terms of patients' wishes regarding the use of tissue for research (table 6). The average rate of agreement for tissue use in research was 95%.
Table 6 Wide variation between departments in terms of patients' wishes regarding the use of tissue for research.
| Department | Completed forms | % agree |
|---|---|---|
| Anaesthetics | 37 | 100 |
| Cardiothoracic surgery | 11 | 100 |
| Dermatology | 556 | 95 |
| Ear, nose and throat | 79 | 100 |
| Gastroenterology | 937 | 98 |
| General surgery | 394 | 98 |
| Genitourinary medicine | 21 | 100 |
| MaxFac/dental | 43 | 98 |
| Neurology/neurosurgery | 47 | 98 |
| Obs and gynae | 485 | 95 |
| Oncology | 14 | 100 |
| Ophthalmology | 9 | 100 |
| Orthopaedics | 2 | 50 |
| Paediatrics | 115 | 88 |
| Plastic Surgery | 119 | 100 |
| Radiology | 19 | 100 |
| Respiratory Medicine | 22 | 86 |
| Rheumatology | — | — |
| Urology | 103 | 69 |
| Vascular Surgery | — | — |
MaxFac, maxillofacial; Obs and Gynae, obstetrics and gynaecology.
That a higher rate of disagreement was found in paediatrics was not unexpected in view of the volume of organ retention enquiries in Leeds, which had received much publicity. Interestingly, however, obstetrics and gynaecology rejection was very close to the average. However, the high rates in two areas, dermatology and urology, were unexpected, and these seem to have been caused by the outliers referred to previously. If they are removed from the calculations, the overall rejection rate drops further to 3%.
Discussion
It is very encouraging to see that when patients are approached by interested staff, the vast majority altruistically agree to donate tissues. Less than 4% of them declined the storage and use of tissue for further use, including research. The widespread concern of relatives to the non‐consented removal and retention of autopsy tissues does not seem to apply to surgically removed tissues. Interestingly, the level of consent in routine practice is at the same level as that experienced in clinical trials such as the Medical Research Council FOCUS10 Trial of chemotherapy in advanced metastatic colorectal cancer where 95% of patients consented to tissue research on entering the trial. A similar level of tissue consent was also reported in Peterborough11 among patients undergoing surgery, who were asked to donate surplus tissue for use in pharmaceutical company research.
This model seems to work well for those patients who were asked by an interested member of the clinical staff. The nurses outperformed the medical staff and any model should aim to maximise the use of such practitioners. The model fails in practice because many of the consent forms may not be filled in, are not forwarded to their intended destination, or the tissue sections of the form are left blank. The tissue from these patients cannot be used for research because we do not know the status of consent. This seems perverse as we know that over 97% of patients whose preferences were known wished us to use the material, but owing to factors outside the control of the histopathology department, their wishes were not made aware of.
The level of consent changed little between the two audits, but the level of receipt of completed forms rose by 20% with familiarity alone. If this method of consent is to be used more widely, then we envisage that investment is required for education and audits. Each district general hospital will have to employ a tissue nurse and major teaching hospitals may require more than one.
Although the Human Tissue Act 2004 stipulates that consent is not essential for the use of anonymised surgical tissue for research, the Human Tissue Authority draft code of conduct14 states, “In general obtaining consent is preferable to developing complex systems for keeping samples unlinked. It represents best practice and has the added benefit of facilitating approval by a REC [Research Ethics Committee]”.
The model of consent at admission by properly trained clerks or admission nurses to obtain a generic consent, similar to that proposed by the Royal College of Pathologists in 2001,15 would seem to be optimal and we believe that research is worthy of funding. Unfortunately as Professor Furness pointed out in his letter of March 2006,16 no initiative has been taken up in this direction from either the Department of Health or the Human Tissue Authority. The funding for the Tissue Bank Nurse who carried out this audit was a generous donation from a pharmaceutical company, Genentech (San Francisco, California, USA).
Importantly, this study shows that even without education of staff or patients there is consistently very low rejection of the use of tissue for research. It also shows that to obtain universal consent, a major programme of education and audit would be required. Using our model, we know that 56% of patients' material has been lost to research, because the Trust's policy is only to use tissue where the patients' wishes are known. When less than 1 in 25 of these patients would have objected to their tissue being used for research have we got the process wrong for surgical tissues? Is it ethical to deny 24 patients their wish to be altruistic for the one who does not wish to contribute their tissues, because they have not been correctly asked? Is it in the public interest?
A further loss of material has arisen from the outliers in the consenting practice where nearly all the no‐consent boxes were ticked. There has to be a large question mark over the validity of such forms and how “informed” the consenting process was as consensus on this scale is seen nowhere else in the 4770 forms audited in 2003. It also raises issues of either medical staff acting to minimise their exposure to risk of misuse of research tissues by failing to discuss the facts in a balanced way or deliberately filling in the no box without discussion with the patient.
In this study, we have not explored the reasons for rejecting further use of tissue. These may derive from a deeply held religious belief, apathy, lack of trust in doctors or researchers, side effects of illness or a failure of the treating clinician to explain the benefits to others and society of that donation. Further studies are needed to understand the reasons for research rejection, allowing medical researchers to further improve consent rates.
If we are to meet the highest standards of research governance, which we would wish to, and to live up to the best practice advocated by the Human Tissue Authority, then resources must be made available to trusts who understandably find it hard to fund tissue nurses when faced with competing demands on their funds.
Take‐home messages
Less than 5% of patients whose views were recorded disagreed with the use of their tissue for research.
After 2 years, the second audit revealed compliance of 71% of forms received with a histology request, but of these only 57% were fully completed.
Wide variation in the effectiveness of consenting was seen with nurses obtaining better rates of form completion than medical staff. The more junior the medical staff, the worse they performed.
There was evidence of variation in performance between departments, and of individual clinicians biasing the results of the consent.
Patients seem to be very altruistic about the use of their tissues but recording this fact requires resourcing if it is to be performed effectively in the National Health Service.
Abbreviations
NHS - National Health Service
Footnotes
Funding: Genentech (San Francisco, California, USA) provided funding for JW's salary.
Competing interests: None.
Ethical approval was not required as this study was an audit of the consent process.
This study was performed independently of the funding source and the employer organisations.
References
- 1.Department of Health Reference guide to consent for examination or treatment. London, UK: DH, 2001
- 2.Royal College of Pathologists Transitional guidelines to facilitate changes in procedures for handling ‘surplus' and archival material from human biological supplies. London, UK: Royal College of Pathologists, 2001
- 3.British Medical Association Report of consent working party (including tool kit). London, UK: BMA, 2001
- 4.General Medical Council Research: the role and responsibilities of doctors. London, UK: General Medical Council, 2002
- 5.Her Majesty's Stationery Office The Human Tissue Act 2004. London, UK: HMSO, 2004
- 6.Department of Health Good practice in consent implementation guide. London, UK: DH, 200123
- 7.House of Commons The Royal Liverpool Children's Inquiry Report (Chairman: Michael Redfern QC). UK: HC, 2001
- 8.Bristol Royal Infirmary Learning from Bristol: the report of the public inquiry into children's heart surgery at the Bristol Royal Infirmary. (Chairman: Sir Ian Kennedy) Cm 5207, UK, BRI 2001
- 9.Start R D, Brown W, Bryant R J.et al Ownership and uses of human tissue: does the Nuffield bioethics report accord with opinion of surgical inpatients? BMJ 19963131366–1368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nuffield Council on Bioethics Human tissue: ethical and legal issues. London: Nuffield Council on Bioethics, 1995
- 11.Policy for consent to examination or treatment. Leeds, UK: Leeds Teaching Hospitals NHS Trust, 200214
- 12.Adlard J W, Richman S D, Stephens R.et al The MRC CR08 (FOCUS) Trial molecular pathology project. Br J Cancer 200286s77 [Google Scholar]
- 13.Jack A L, Womack C. Why surgical patients do not donate tissue for commercial research: a review of the records. BMJ 2003327262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Human Tissue Authority Code of Practice Conduct V1.0. Human Tissue Authority 16 January 2006: 11, (para 29),
- 15.Royal College of Pathologists Transitional guidelines to facilitate changes in procedures for handling ‘surplus' and archival material from human biological samples. London, UK: RCP, 2001
- 16.Furness P. One‐time general consent for research on biological samples. BMJ 2006332665. [DOI] [PMC free article] [PubMed] [Google Scholar]