Abstract
Synovial sarcoma occurs predominantly in the soft tissues of the extremities, but is exceedingly rare in the mediastinum. It has overlapping histological and immunophenotypic features with other tumours in the differential diagnosis. We report a case of a patient who had an incidental finding of such a tumour. Because of the rarity of this tumour in the mediastinum, optimal therapy is unknown and the prognosis remains guarded.
Keywords: mediastinal tumour, sarcoma
INTRODUCTION
Synovial sarcoma is a malignant neoplasm predominantly affecting soft tissues of the extremities of adolescents and young adults1. It occurs in less than 10% of patients over 60 years old, in which this diagnosis is often not considered2. Its' occurrence as a primary tumour in the mediastinum is rare and was first described in the medical literature in the mid 1990's3. Herein, we report a further case of a mediastinal sarcoma that required a pneumonectomy to excise completely. We utilised positron emission tomography and computed tomography (PET-CT) to aid in the staging.
CASE HISTORY
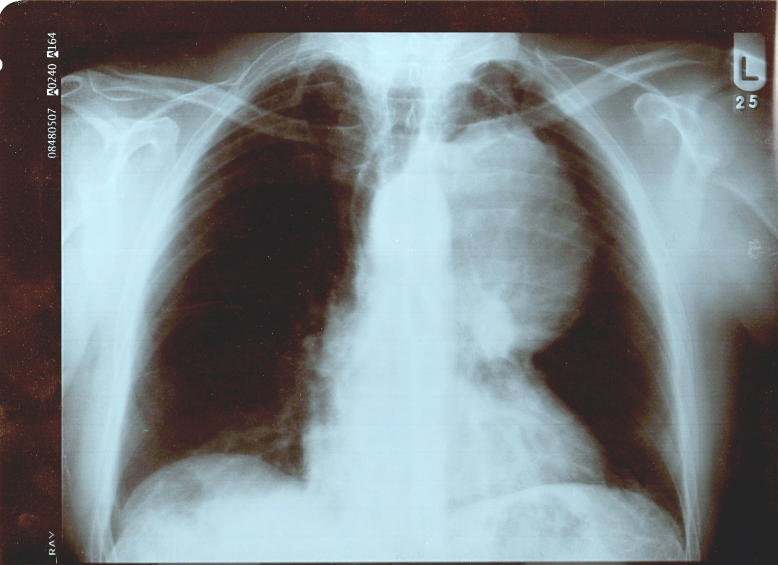
A 59 year old male smoker presented to his local casualty department with non specific abdominal pain. During his workup, a chest X-ray was performed which revealed a large mass in the left thoracic cavity, adjacent to the mediastinum (Fig 1). Computed tomography (CT) scan revealed a 12.4cm mass within the left upper zone of the chest. It was closely related to the brachio-cephalic vein and aortic arch, but there was a clear plane of cleavage. However as the mass progressed inferiorly, it appeared to be in close contact with the main pulmonary artery and the left pulmonary artery.
Fig 1.
Chest radiograph demonstrating a mass abutting the mediastinum within the left hemithorax.
A flexible bronchoscopy was subsequently performed which demonstrated extrinsic compression of the left upper lobe bronchus. However, bronchial washings were negative for malignant cells. To gain a tissue diagnosis, we performed a left anterior thoracotomy which also allowed us to examine the mediastinum for resectability. This revealed the tumour to be free from the visible lung but adherent to the mediastinum. Histopathological analysis found it to be a poorly differentiated sarcoma. PET-CT scan was performed to exclude any metastatic disease. This demonstrated an 18F-Fluorodeoxyglucose (18F-FDG) avid mass with a standardised uptake value (SUV) of 16 with no other foci that may represent metastatic disease (Fig 2).
Fig 2.
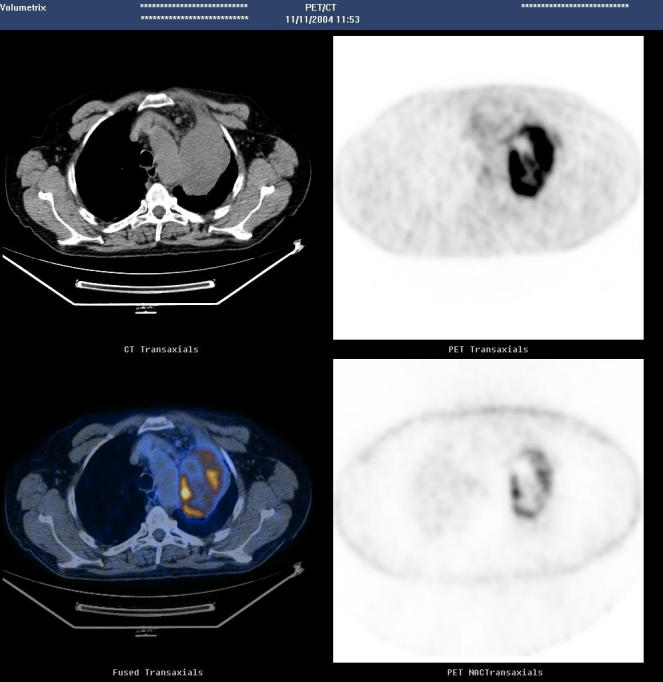
Transaxial image showing tumour with plane of cleavage from arch of aorta. Small volume of pre-vascular/superior mediastinal nodes on CT are not FDG avid.
At thoracotomy, the mass was seen arising from the left hilum, adherent to the left pulmonary artery, left superior pulmonary vein, phrenic nerve and adjacent pericardium and required an intrapericardial pneumonectomy and resection of the latter two structures to achieve complete resection. Histopathological analysis revealed a biphasic synovial sarcoma. The primary site for this tumour was uncertain as the tumour was located in the lateral portion of the mediastinum, close to both the pleura and pericardium. The patient made an uneventful recovery and at 18 months post-operative follow-up was disease free and his quality of life had returned to normal.
PATHOLOGY
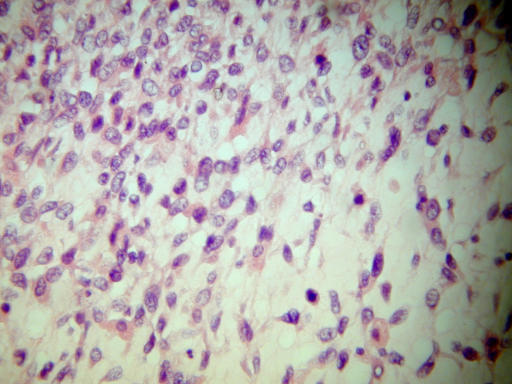
The tumour measured 13 × 9 × 6cm and was adherent to the hilar surface of the left lung. Sectioning revealed a uniform consistency and it was sharply demarcated from the lung parenchyma. Histologically the tumour was composed of spindle cells and epithelioid cells (Fig 3) although the spindle cells were predominant. Numerous mitotic figures (more than 4 per 10 high power field) were seen and there were focal areas of necrosis. Immunohistochemistry demonstrated strong positivity for Vimentin, Cytokeratins, and focal positivity for EMA. Mesothelial markers (CK5/6, Calretinin) and primary pulmonary tumour marker (TTF-1) were negative. These findings would be consistent with a biphasic synovial sarcoma.
Fig 3.
Histology demonstrating spindle and epithelioid cells.
DISCUSSION
The mediastinum is host to a vast array of both primary and metastatic neoplasms, the differential diagnosis of which is extensive and depends upon the mediastinal compartment involved, clinical history, presentation, and age of the patient. The case illustrated demonstrates the diagnostic difficulty encountered when the patient's age and tumour location are taken into account, as synovial sarcomas are rare mesenchymal neoplasms that primarily affect the deep soft tissues of the extremities and predominates in adolescents and young adults1. Although synovial sarcoma has been reported to metastasise to the mediastinum, its occurrence as a primary neoplasm in this location is rare and has only recently been recognised3. Patients have presented with dyspnoea4, chest pain1, cardiac tamponade5 and as an incidental finding1.
Classically, synovial sarcoma is a biphasic tumour composed of spindle shaped fibroblast-like cells and epithelioid cells, but the majority are actually monophasic spindle cell in type. A poorly differentiated variant composed of small round cells has also been described.
The differential diagnosis for thoracic synovial sarcomas includes mesothelioma, fibrosarcoma, malignant peripheral nerve sheath tumour, smooth muscle tumours, thymoma, blastoma, and sarcomatoid carcinoma6. However, the diagnosis can be difficult to achieve in an unusual location, overlapping histological and immunohistological features, or if a small sample size is present6. Immunohistochemistry can be very helpful. Synovial sarcomas are positive for Vimentin, EMA, Cytokeratins, CD99 (∼60%) and S100 (∼30%)7. The availability of molecular genetic identification (fluorescent in situ hybridization or polymerase chain reaction) of the t(X;18) has improved diagnostic specificity as this translocation is found in over 90% of synovial sarcomas1. This translocation involves the SYT gene on chromosome 18 and either the SSX1 or SSX2 gene on the X chromosome1.
Accurate staging of the disease is important for appropriate patient management and requires the evaluation of the primary tumour and assessment for distant disease. Magnetic resonance imaging (MRI) has been the traditional imaging tool for assessment of soft tissue masses, but more recently soft tissue sarcomas are well recognised as showing increased 18F-FDG uptake in Positron Emission Tomography (PET)8.
PET-CT combines the strengths of two imaging modalities, exploiting the recognised greater sensitivity of CT in demonstration of small volume lung metastases (sensitivity, specificity 100%, 96.4% vs. 86.7%, 100%) and enhancing 18F-FDG PET imaging by allowing precise anatomical localisation of functional abnormalities8. MRI frequently struggles to differentiate the inflammatory and fibrotic changes which occur following surgery and adjuvant therapy from recurrent disease, whilst 18F-FDG PET allows accurate differentiation of locally recurrent disease from healing/post-surgical change8. Combined PET-CT imaging is likely to become the imaging modality of choice for follow-up of patients with these rare tumours.
Broad surgical resection is the cornerstone of therapy. Complete resection of the tumour was the overwhelming factor in determining survival in a review of primary mediastinal sarcomas9. Radiotherapy is recommended with positive margins10. The place for chemotherapy of this tumour is not well defined, and in none of the other case reports was preoperative chemotherapy given5. Combination of adriamycine and ifosfamide has been used as an adjuvant therapy and for recurrences5. Prognosis used to be poor with survival lasting two months4, but with aggressive multimodal therapy, survival up to 14 years has been documented5.
In summary, though mediastinal sarcoma is a rare entity, if aggressively treated with complete resection and or multimodal therapy with intensive follow-up, the survival of such patients can improve.
The authors have no conflict of interest.
REFERENCES
- 1.Trupiano JK, Rice TW, Herzog K, Barr FG, Shipley J, Fisher C, et al. Mediastinal synovial sarcoma: report of two cases with molecular genetic analysis. Ann Thorac Surg. 2002;73(2):628–30. doi: 10.1016/s0003-4975(01)03110-1. [DOI] [PubMed] [Google Scholar]
- 2.Chan JA, McMenamin ME, Fletcher CD. Synovial sarcoma in older patients: clinicopathological analysis of 32 cases with emphasis on unusual histologic features. Histopathology. 2003;43(1):72–83. doi: 10.1046/j.1365-2559.2003.01643.x. [DOI] [PubMed] [Google Scholar]
- 3.Peoc'h M, Le Marc'hardour F, Bost F, Pasquier D, Roux JJ, Pinel N, et al. Primary synovial sarcoma of the mediastinum. A case report with immunohistochemistry, ultrastructural and cytogenetic study. [French] Ann Pathol. 1995;15(3):203–6. [PubMed] [Google Scholar]
- 4.Yano M, Toyooka S, Tsukuda K, Dote H, Morimoto Y, Ohata N, et al. SYT-SSX fusion genes in synovial sarcoma of the thorax. Lung Cancer. 2004;44(3):391–7. doi: 10.1016/j.lungcan.2003.11.011. [DOI] [PubMed] [Google Scholar]
- 5.Van der Mieren G, Williems S, Sciot R, Dumez H, Van Oosterom A, Flameng W, et al. Pericardial synovial sarcoma: 14-year survival with multimodality therapy. Ann Thorac Surg. 2004;78(3):e41–2. doi: 10.1016/j.athoracsur.2004.02.011. [DOI] [PubMed] [Google Scholar]
- 6.Aubry MC, Bridge JA, Wickert R, Tazelaar HD. Primary monophasic synovial sarcoma of the pleura: five cases confirmed by the presence of SYT-SSX fusion transcript. Am J Surg Pathol. 2001;25(6):776–81. doi: 10.1097/00000478-200106000-00009. [DOI] [PubMed] [Google Scholar]
- 7.Suster S, Moran CA. Primary synovial sarcomas of the mediastinum: a clinicopathologic, immunohistochemical and ultrastructural study of 15 cases. Am J Surg Pathol. 2005;29(5):569–78. doi: 10.1097/01.pas.0000157934.50936.3e. [DOI] [PubMed] [Google Scholar]
- 8.Jadvar H, Gamie S, Ramanna L, Conti PS. Musculoskeletal system. Semin Nucl Med. 2004;34(4):254–61. doi: 10.1053/j.semnuclmed.2004.06.002. [DOI] [PubMed] [Google Scholar]
- 9.Burt M, Ihde JK, Hajdu SI, Smith JW, Bains MS, Downey R, et al. Primary sarcomas of the mediastinum: results of therapy. J Thorac Cardiovasc Surg. 1998;115(3):671–80. doi: 10.1016/S0022-5223(98)70333-2. [DOI] [PubMed] [Google Scholar]
- 10.Al-Rajhi N, Husain S, Coupland R, McNamee C, Jha N. Primary pericardial synovial sarcoma: a case report and literature review. J Surg Oncol. 1999;70(3):194–8. doi: 10.1002/(sici)1096-9098(199903)70:3<194::aid-jso10>3.0.co;2-8. [DOI] [PubMed] [Google Scholar]