Abstract
Objective
To design and test a miniature ambulatory hot flash recorder which uses neither electrodes nor gel.
Design
In the first study, putative hot flashes recorded using a relative humidity (RH) sensor were compared to patient event marks. In the second study, RH recorded using a complete prototype recorder was compared to sternal skin conductance (SCL) recordings made on a Biolog recorder, as well as to event marks.
Setting
University medical center.
Patients
Ten healthy postmenopausal women reporting frequent hot flashes and using no medication.
Interventions
Body heating in laboratory.
Main Outcome Measures
Positive Predictive Value (PPV), sensitivity, specificity.
Results
In both laboratory studies, the PPV, sensitivity, and specificity among all 3 measures (RH, SCL, event) was 100%. In the field, an RH increase of 3%/min compared to SCL-detected hot flashes yielded a PPV of 95.6%, a specificity of 95.2%, and a sensitivity of 90.9%.
Conclusions
This device should be useful as an endpoint in clinical trials of treatments for hot flashes.
Keywords: hot flash, skin conductance, relative humidity, ambulatory monitoring
Introduction
Much research is currently underway on new treatments for menopausal hot flashes. However, this research is hindered by the lack of suitable outcome measures. Patient-reported outcome measures, such as diaries, have not been standardized and suffer from lack of compliance, recall bias, and lost data, among other factors.(1, 2)
Research over the past several years has identified sternal skin conductance level (SCL) as the best objective indicator of hot flashes. (3–6) However, existing ambulatory recording devices are cumbersome and difficult to use. Moreover, they require the use of gel-filled electrodes which must be changed every 24 hours due to drying of the gel and accumulation of sweat. Since most patients are not capable of doing this successfully nor of stopping and restarting the recorders, frequent clinic visits are necessary for extended recording periods. This is inconvenient and expensive.
Here we describe a miniature, hygrometric (humidity) hot flash recorder which uses neither electrodes nor gel. It can be easily removed and reattached by patients, has no controls, and will record for 31 days on a single hearing aid battery.
We performed 2 experiments. In the first, we demonstrated the feasibility of using a miniature hygrometric sensor to detect hot flashes. In the second, we tested the accuracy of a fully-functioning recorder against hot flashes recorded on a Biolog recorder (Morro Bay, CA) and a patient-activated event marker.
Methods
Subjects
Subjects were 10 postmenopausal women reporting frequent (> 6/day) hot flashes. They were healthy and free of all medication including hormone therapy and dietary supplements for hot flashes. They were recruited from newspaper ads requesting volunteers for participation for research on hot flashes and were paid for their participation. All gave written informed consent and all procedures were approved by the Wayne State University IRB.
Procedure
Study 1
A miniature hygrometric sensor was mounted within a 2.5 cm diameter plexiglass disc (Fig. 1). The sensor was attached over the sternum with standard, double-sided, adhesive collars. The output of the sensor was recorded using an A/D converter and PC computer. Two 2.5 cm Ag/AgCl electrodes (Graphic Controls, Buffalo, NY) filled with 0.05 M KCl gel were attached on either side of the sensor, 4 cm apart. SCL was recorded using a 0.5 volt constant-voltage circuit, A/D converter, and PC computer, as previously published.(7) An event marker button was connected to the computer.
Fig. 1.
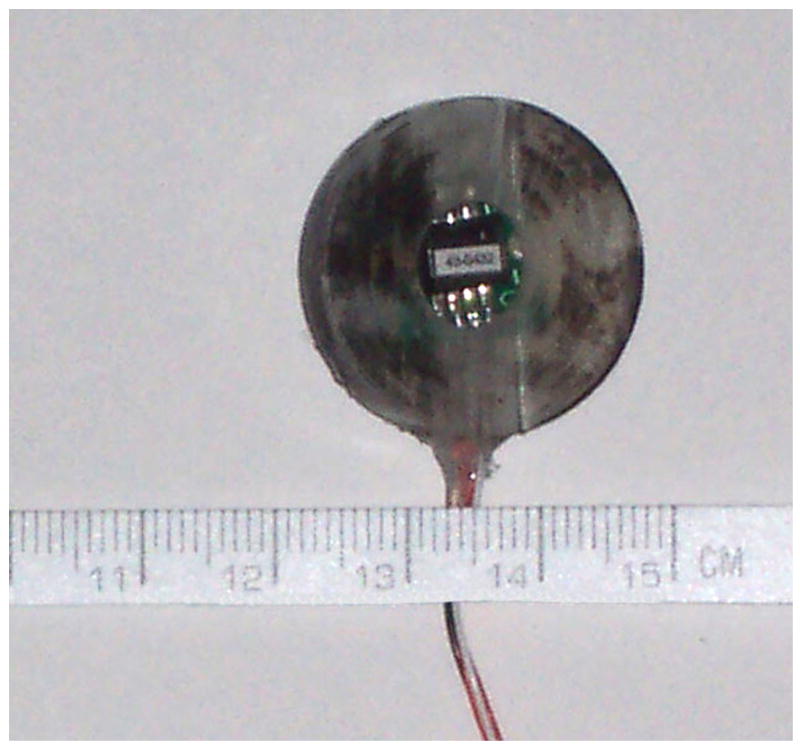
Prototype humidity sensor.
Patients wore cotton scrub suits and reclined in a large arm chair, in a temperature and humidity-controlled (26ºC, 50% relative humidity-RH) room. They were heated with two 40 x 60 cm circulating water pads at 42ºC. Subjects were recorded for 2 h between 1000 and 1700 h. They were instructed to press the event marker button each time a hot flash occurred. After the 2 h recording period the SCL electrodes were removed. The sensor was connected to a Biolog SCL recorder which had been modified to record signals from the sensor. Subjects were then sent home for 24 h after being instructed not to get the recorder wet and to press the event marker each time they had a hot flash.
Study 2
A fully-functioning prototype recorder was designed and constructed by Kolar Engineering (Royal Oak, MI). It consists of a miniature hygrometric sensor, a microcontroller, flash memory, and a hearing aid battery (Fig. 2). The recorder is 3.8 cm in diameter, 1 cm thick, and weighs 14 gm including the battery.
Fig. 2.
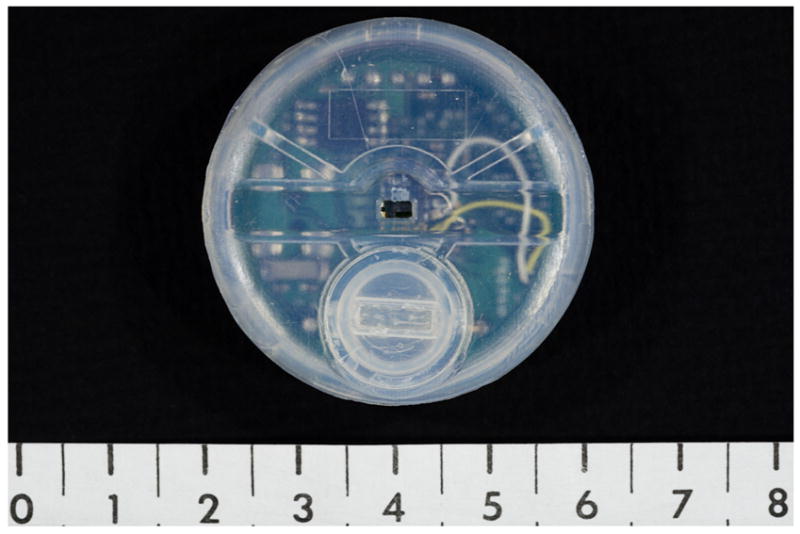
Prototype hot flash recorder. Weight = 14 gm.
Scale in cm.
Patients were instrumented with this recorder, 2 SCL electrodes, and the event marker and received the heat test procedures described in Study 1. At the end of the 2 h period, the SCL electrodes were attached to a Biolog SCL recorder. They were instructed not to get the devices wet and to press the event marker each time a hot flash occurred. Nine women were then recorded for 24 h and one for 60 h.
Data Analysis
For Study 1, the RH, SCL signals and event marks were downloaded from the laboratory PC. The amplitude and duration of each putative hot flash were scored using Excel (Microsoft, Redmond, WA). Then, to determine the criterion RH change for a hot flash, these data were analyzed with a receiver operating characteristic (ROC) analysis using an SCL change of 2 μmho/30 sec as the gold standard. Then, the ambulatory RH data were downloaded from the Biolog and analyzed with an ROC analysis using the event marks as the gold standard.
For Study 2, the RH data from our recorder were downloaded using software written by Kolar Engineering. The amplitude and duration of putative hot flashes were scored using software written by one of us (SLW). SCL signals from the Biolog were downloaded and scored using Biolog software and the 2 μmho/30 sec criterion.
An ROC analysis was used to compare the Biolog and RH detected hot flash counts using the Biolog as the gold standard. Percent RH changes from 2% – 6% in .5% steps over 1 min and 2 min intervals were examined. A second such analysis was performed using the event marks as the gold standard.
Results
Twenty hot flashes meeting the 2 μmho/30 sec SCL criterion were recorded during the laboratory session of Study 1. All were accompanied by an event mark and by an RH increase of 3%/min. There were no false positive or false negative events. Thus the PPV, the sensitivity and the specificity for the 3%/min RH change vs. the SCL criterion and the event marks are 100%.
The ROC analysis of the ambulatory data showed that an RH increase of 3%/min produced the best PPV. There were an average of 12.6 ± 2.6 SD event marks/patient and 17.6 ± 2.2 RH increases (3%/min) per patient during these recordings. Using this criterion RH change against the event marks as the gold standard, the PPV was 71.6%, the specificity was 60.3%, and the sensitivity was 99%.
Eighteen hot flashes meeting the 2 μmho/30 sec SCL criterion were recorded during the laboratory session of Study 2. All were accompanied by an event mark and by an RH increase of 3%/min. There were no false positive or false negative events. Thus the PPV, the sensitivity and the specificity for the 3%/min RH change vs. the SCL criterion and the event marks are 100%.
The ROC analysis of the ambulatory monitoring data again showed that an RH increase of 3%/min produced the best PPV. There were an average of 23.8 (12.7 SD) Biolog-detected hot flashes per patient and 21.4 (11.9) flashes per patient detected by RH. Using the Biolog flashes as the gold standard, the PPV for RH was 95.6%, the specificity was 95.2% and the sensitivity was 90.9%.
There were an average 13.0 (9.9) event marks per patient recorded on the Biolog. Using these as the gold standard, the PPV for RH was 59.7% and the PPV for the Biolog (SCL) was 52.8%.
There were no significant correlations (Pearson r and Spearman rho) between average daily humidity as reported by NOAA (range 60 – 100%) and any of the variables reported above. The ambient RH on the chest was estimated by the basal values shown on the RH recordings and ranged from 40 – 95%. There were no differences in hot flash detection rates across this range and the recordings did not plateau at the upper end.
Discussion
We have developed a miniature hygrometric hot flash recorder which uses neither electrodes nor gel. The recorder was well-tolerated by patients and did not fall off. Patients reported that they did not notice the presence of the recorder and found it vastly preferable to the Biolog.
In the laboratory, the correspondence among an RH increase of 3%/min, SCL-detected hot flashes, and patient event marks was 100%. During 24 – 60 h ambulatory monitoring, using SCL-detected hot flashes as the gold standard, the PPV for the RH criterion was 95.6%, the specificity was 95% and the sensitivity was 90.9%. Thus, the RH-recorded data were very similar to those recorded on the Biolog, but used a simpler, smaller, and less obtrusive device. Using the event marks as the gold standard, the PPV for RH was superior to that of the Biolog.
In the laboratory the PPVs of both devices compared to the event marks was perfect, 100%. In the field the PPVs for both devices compared to the event marks was considerably worse although better than those previously reported for the Biolog.(8) We believe this is due to patient underreporting of the hot flashes, as demonstrated in previous studies.(8) The reasons for this are not clear but may be due to distraction, inconvenience, or failure to perceive the flash during sleep.
The RH recordings were not significantly affected by wide ranges of outdoor humidity or by ambient humidity recorded on the chest. However, the device may not record accurately in locations where the RH is near 100%, such as a steamy bathroom or some tropical climates.
In conclusion, we have invented a miniature hot flash recorder which uses neither electrodes not gel and will operate for 31 days on a single hearing aid battery. The data are comparable to those recorded by SCL but the method is simpler and much easier for patients to utilize. Our recorder should be useful as an endpoint in clinical trials and for research on the determinants of hot flashes.
Acknowledgments
Supported by NIH MERIT Award, R37-AG05233 and Research and Development Funds from Wayne State University.
Footnotes
Disclosure: The authors have patent pending # 60/741,376 on the device described herein.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Takarangi MK, Garry M, Loftus EF. Dear diary, is plastic better than paper? I can’t remember: Comment on Green, Rafaeli, Bolger, Shrout, and Reis. Psychol Methods. 2006;11(1):119–22. doi: 10.1037/1082-989X.11.1.119. [DOI] [PubMed] [Google Scholar]
- 2.Stone AA, Shiffman S, Schwartz JE, Broderick JE, Hufford MR. Patient compliance with paper and electronic diaries. Controlled Clinical Trials. 2003;24:182–199. doi: 10.1016/s0197-2456(02)00320-3. [DOI] [PubMed] [Google Scholar]
- 3.Freedman RR. Laboratory and ambulatory monitoring of menopausal hot flashes. Psychophysiology. 1989;26:573–579. doi: 10.1111/j.1469-8986.1989.tb00712.x. [DOI] [PubMed] [Google Scholar]
- 4.Freedman RR, Woodward S, Norton D. Laboratory and ambulatory monitoring of menopausal hot flushes: comparison of symptomatic and asymptomatic women. J Psychophysiol. 1992;6:162–166. [Google Scholar]
- 5.de Bakker IPM, Everaerd W. Measurement of menopausal hot flushes: validation and cross-validation. Maturitas. 1996;25:87–98. doi: 10.1016/0378-5122(96)01046-8. [DOI] [PubMed] [Google Scholar]
- 6.Carpenter JS, Andrykowski MA, Freedman RR, Munn R. Feasibility and psychometrics of an ambulatory hot flash monitoring device. Menopause. 1999;6:209–215. doi: 10.1097/00042192-199906030-00006. [DOI] [PubMed] [Google Scholar]
- 7.Freedman RR. Biochemical, metabolic, and vascular factors in menopausal hot flashes. Fertil Steril. 1998;70:332–7. doi: 10.1016/s0015-0282(98)00137-x. [DOI] [PubMed] [Google Scholar]
- 8.Carpenter JS, Monahan PO, Azzouz F. Accuracy of subjective hot flash reports compared with continuous sternal skin conductance monitoring. Obstetrics and Gynecology. 2004;104:1322–6. doi: 10.1097/01.AOG.0000143891.79482.ee. [DOI] [PubMed] [Google Scholar]


