Abstract
Pulsatile growth hormone (GH) secretion differs between males and females and regulates the sex-specific expression of cytochrome P450s in liver. Sex steroids influence the secretory dynamics of GH, but the neuroendocrine mechanisms have not been conclusively established. Because periventricular hypothalamic somatostatin (SST) expression is greater in males than in females, we generated knockout (Smst–/–) mice to investigate whether SST peptides are necessary for sexually differentiated GH secretion and action. Despite marked increases in nadir and median plasma GH levels in both sexes of Smst–/– compared with Smst+/+ mice, the mutant mice had growth curves identical to their sibling controls and retained a normal sexual dimorphism in weight and length. In contrast, the liver of male Smst–/– mice was feminized, resulting in an identical profile of GH-regulated hepatic mRNAs between male and female mutants. Male Smst-/- mice show higher expression of two SST receptors in the hypothalamus and pituitary than do females. These data indicate that SST is required to masculinize the ultradian GH rhythm by suppressing interpulse GH levels. In the absence of SST, male and female mice exhibit similarly altered plasma GH profiles that eliminate sexually dimorphic liver function but do not affect dimorphic growth.
Introduction
The episodic release of growth hormone (GH) from pituitary somatotrophs results from a complex interplay primarily between two hypothalamic peptides, the stimulatory GH-releasing hormone (GHRH) and the inhibitory somatostatin (SST) (1). Activation of the GH secretagogue receptor (GHS-R) in hypothalamus and pituitary further modulates the actions of the two classically defined regulators of GH secretion (2). Direct measurement of GHRH and SST in hypophyseal-portal blood of male rats indicates a rhythmic pattern of release of these two neuropeptides at regular 3- to 4-hour intervals about 180° out of phase (3). In contrast, female rats appear to have a different release pattern of the two peptides characterized by continuous secretion of SST and episodic, rather than rhythmic bursts of GHRH. As a result, GH secretory profiles in females are distinct from males and may account for the striking sex difference in somatic growth (4). Male rats exhibit narrow GH pulses with a frequency of about one pulse every 3–4 hours and prolonged nadir values below 1–2 ng/ml. Female rats exhibit relatively broader pulses with an irregular frequency and nadir values of 5–20 ng/ml (4). In humans, a similar sexual diergism (functional dimorphism) of GH secretion exists between men and women, indicating phylogenetic conservation of neuroendocrine hormone rhythms (5).
The underlying mechanisms for such a sharp sex-specific difference in GH secretion remain unclear. Periventricular hypothalamic SST peptide and mRNA levels are higher in male compared with female rats and mice (6, 7), leading to the suggestion that sex differences in hypothalamic SST signaling to pituitary somatotrophs play a key role in the sexually diergic GH responses (1). Ontogenic studies have demonstrated that these differences are first evident at postnatal day 5 and continue to develop in an orderly cascade through puberty into adulthood (8, 9). There are five known SST receptors (SSTRs) with distinct cellular distributions and subtle differences in intracellular signaling that mediate the actions of SST peptides (10). Furthermore, sexual diergism has been noted for expression of SSTR1, 2, 3, and 5 in the anterior pituitary and for SSTR1 but not SSTR2 in the rat hypothalamus (11–13). Although estrogen and testosterone both influence hypothalamic Smst gene expression and play a major developmental role in organizing the sexual diergism of GH secretion, the effect of gonadal steroids is not limited to the critical perinatal period of imprinting. Treatment of adults with either 17-β-estradiol or testosterone feminizes or masculinizes the GH secretory profile of male and female rats, respectively (14, 15).
Sex differences in GH pulsatility are ultimately responsible for sexual differentiation of the liver, a major target organ of GH (4). In particular, many members of the cytochrome P450 (CYP) and the major urinary protein (MUP) gene families are differentially regulated by the sex-specific pattern of GH secretion (16, 17). A key determinant of hepatic gene regulation in males is the long interpulse nadir of GH levels, which permits the resensitization of GH receptor signaling by Janus kinase/signal transducer and activation of transcription (JAK-STAT) cascades (18) specifically involving STAT 5a and 5b proteins (19–23). The hepatic microsomal enzymes regulated by GH have important physiological roles in the hydroxylation and metabolism of both endogenous steroid hormones and xenotoxins, thereby providing a possible link between sexual differentiation of the brain and sex differences in susceptibility to chemical toxicity and carcinogenicity (24).
The goal of our present studies was to test directly the hypothesis that SST is a physiological determinant of masculinized GH secretory dynamics and sexually dimorphic patterns of somatic growth. Immunological, antisense, and pharmacological approaches to the abrogation of SST function all have important limitations in their selectivity, specificity, and extent of action. Although both the SSTR2 and SSTR1 genes have been knocked out in mice (25, 26), there have been no reports on the consequences of these mutations for sexually dimorphic GH release in vivo. Therefore, we chose to address this problem by the generation of gene-knockout mice lacking all forms of proSST-derived peptide ligands. We then analyzed growth, expression of SSTR1-5 in hypothalamus and pituitary gland, and GH secretion by a combination of direct and indirect assays in both sexes of somatostatin-deficient mice.
Methods
Gene targeting.
Mouse genomic DNA fragments used for construction of the Smst targeting vector were isolated from a 129S6 cosmid library, generated by standard techniques in our laboratory, by hybridization to a rat SST cDNA probe (27). E14TG2A embryonic stem (ES) cells derived from 129P2/OlaHsd mice were electroporated and selected in G418 as described previously (28). Homologous recombination of both long and short arms was confirmed by Southern blot analysis of genomic DNA, and correctly targeted ES cells were microinjected into C57BL/6J (The Jackson Laboratory, Bar Harbor, Maine, USA) blastocysts to generate the founder chimeric mice. Chimeric males were mated with C57BL/6J females, and the resulting F1 offspring were crossed to produce F2 hybrid mice (129P2/OlaHsd, C57BL/6J). F1 heterozygotes (Smst+/–) were also backcrossed for five successive generations to produce N5 incipient congenic C57BL/6J mice. Genotyping was performed by touchdown PCR using three primers: R460 (SST sense) 5′-AGTTTCTGCAGAAGTCTCTGGC-3′; S229 (PGK-neo sense) 5′-CTAAAGCGCATGCTCCAGAC-3′; and R465 (SST antisense) 5′-CAGGATGTGAATGTCTTCCAG-3′.
DNA fragments of 950 and 450 bp were amplified from the wild-type (+) and mutant (–) alleles, respectively. Phenotypic analyses were first performed using sibling offspring from Smst+/– F1 mating pairs and were then confirmed and extended using sibling offspring from Smst+/– N5 mating pairs. All procedures involving mice were approved by the Institutional Animal Care and Use Committee and followed the Public Health Service’s guidelines.
Histology and immunocytochemistry.
Histological analyses were performed on tissue fixed in 4% paraformaldehyde, and 50-μm sections of brain were collected with a vibratome. Sections were incubated with 5% normal goat serum followed by incubation with one of the following primary antisera at the indicated dilutions: anti–SST-14 (1:2,000) (29); anti-SST prohormone cryptic peptide (1:1,000) (29); anti-mouse GHRH (1:5,000) (30); or one of a panel of anti-peptide SSTR1-5 antisera 1:400 (31) at 4°C overnight. With intervening washes in Tris-buffered saline, the sections were incubated with biotinylated goat anti-rabbit secondary antibody at room temperature for 30 minutes, followed by exposure to avidin-biotin horseradish peroxidase complex (Vectastain Elite ABC Kit; Vector Laboratories, Burlingame, California, USA) in PBS at room temperature for 30 minutes. The reaction was revealed by chromagen diaminobenzidine containing 0.1% hydrogen peroxide and yielded a brown reaction product. Controls used to validate the specificity of the SSTR immunoreactivity included preimmune serum in place of primary antibody and primary antibody adsorbed with excess antigen.
Hormone assays.
Hormone levels were measured in tissue extracts or plasma (27) using an SST RIA (Peninsula Laboratories Inc., San Carlos, California, USA) and rat IGF-1 RIA (Diagnostic Systems Laboratories Inc., Webster, Texas, USA) according to the manufacturers’ instructions. For mouse GH RIA, a double-antibody method was employed, using highly purified mouse GH (AFP10873B) as the iodinated ligand, anti-rat GH (NIDDK–anti-rat GH-S5) as the primary antibody, and mouse GH (AFP10873B) as the “cold standard,” or reference preparation. These immunoreagents were developed by A.F. Parlow (National Hormone and Peptide Program). The assay has a minimum sensitivity of 0.5 ng/ml using 10 μl plasma. Inter- and intra-assay variations were 9% and 5%, respectively. Estradiol, testosterone, and thyroxine were quantified by core RIA laboratories using standard methodologies.
Semiquantitative RT-PCR analysis.
mRNAs for SSTR1-5, SST, and cortistatin (CST) were analyzed by semiquantitative RT-PCR using modifications of methods described elsewhere (32). Total RNA was isolated from pools of hypothalamic blocks or whole pituitary glands obtained from 16 each of male and female Smst+/+ and Smst–/– mice using the guanidine-isothiocyanate phenolchloroform extraction method. The RNA was reverse transcribed, and the resulting cDNA samples were amplified by PCR using rat SSTR1-5 and mouse SST and CST primers. The sequences for SSTR1-5 primers have been published previously (32). The primers used for SSTR2 only amplify the mouse SSTR2A isoform. The following primers were used for PCR amplification of SST and CST: SST (sense) 5′-GCTCCCTCGGACCCCAGACTG-3′ (nucleotides [nt] 73–93); SST (antisense) 5′-ACAGGATGTGAATGTCTTCCAG-3′ (nt 992–1013); CST (sense) 5′-TGGCCGAGGCACAGGAGGCAAG-3′ (nt 9–30); and CST (antisense) 5′-TCAGGTCTCGTTGGCATCTCACA-3′ (nt 1413–1435). The SSTRs and SST and CST cDNAs were coamplified with β-actin. PCR products were separated by electrophoresis, and Southern blots were probed with [32P]-labeled cDNA probes followed by autoradiography and densitometric quantitation. Values of SSTR1-5 mRNA expression were normalized to those of β-actin mRNA on the same gels. All experiments were performed four times, and each mRNA quantification represents the average of at least three measurements.
Northern blots of liver mRNA.
Total RNA was prepared from 100 mg of liver homogenized in 3 ml of 4 M guanidinium and electrophoresed on 1.5% agarose formaldehyde gels. After RNA transfer, the Duralon nylon membranes (Stratagene, La Jolla, California, USA) were sequentially hybridized with [32P]-radiolabeled probes, imaged on a Molecular Dynamics phosphorimager (Molecular Dynamics, Sunnyvale, California, USA), stripped, and rehybridized. Antisense oligodeoxynucleotide sequences used for end labeling with T4 DNA kinase were (MUPs I/II) 5′-GAGCACTCTTCATCTCTTACAGT-3′; (MUPs III) 5′-TCGCAGTCATTTCGGTGC-3′; (albumin) 5′-TCTACAGCAGGGCTGCCTCG-3′ (18S RNA) 5′-ACGGTATCTGATCGTCTT-CGAACC-3′. Mouse cDNA sequences used for random-primer labeling were a 500-bp NcoI-BamHI prolactin receptor (33) and a 550-bp BamHI-EcoRI Cyp450-15α2A4 (34) cloned fragments.
Statistics.
Data were analyzed by multifactor ANOVA using StatView Power PC version for Macintosh (version 5.1; SAS Institute Inc., Cary, North Carolina, USA) except where otherwise stated. Post hoc comparisons between groups were performed by Fisher’s protected least significant difference (PSLD), and P values < 0.05 were considered significant. GH data sets with different means were compared by χ2 analyses after calculating Z scores [Z = (x – μ)/σ] for each data point. The Z transformation permits an approximation of the probabilities for each x using the probabilities derived from a standard normal distribution (μ = 0; σ = 1).
Results
Generation of an Smst null allele by homologous recombination.
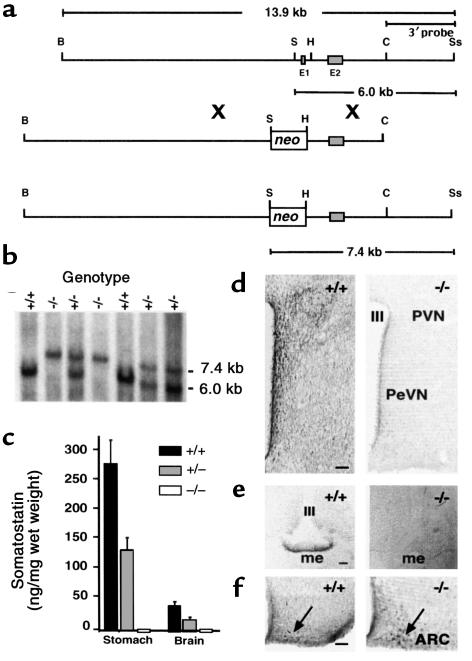
The gene targeting strategy replaced critical Smst promoter elements and exon 1, which contains the translational start site for preproSST, with a neo selection cassette (Figure 1a). One correctly targeted ES cell clone produced germline-transmitting chimeras that were the founders for a colony of F2 hybrid mice (129P2/OlaHsd, C57BL/6J) and, subsequently, N5 incipient congenic C57BL/6J mice. The Smst null allele was transmitted from mating pairs of Smst+/– mice in a Mendelian ratio of 1:2:1 for Smst+/+:Smst+/–:Smst–/– genotypes (Figure 1b). Smst–/– mice of both genetic backgrounds were healthy and fertile and raised normal litters. To verify that the gene mutation resulted in the loss of SST peptides, we analyzed tissue extracts by a RIA that detects both the 14 and 28 amino acid forms of SST. SST-like immunoreactivity was reduced by 50% in stomach and brain from Smst+/– mice and was below the RIA sensitivity in Smst–/– mice (Figure 1c).
Figure 1.
Generation of SST-deficient mice by homologous recombination. (a) Restriction maps of the mouse Smst gene locus (top), targeting vector (middle), and predicted Smst null allele after homologous recombination (bottom) indicate the replacement of exon 1 (E1) and the Smst promoter by a PGK-neomycin selection cassette (neo). B, BamHI; S, SalI; H, HindIII; C, ClaI; Ss, SspI. (b) A Southern blot of genomic DNA digested with SalI and SspI was hybridized with the 3′ probe indicated in a. The 6.0-kb band represents the wild-type allele and the 7.4-kb band represents the Smst null allele in the offspring of an Smst+/– mating pair. (c) RIA of SST in extracts of stomach and total brain (n = 3) demonstrates a 50% reduction in Smst+/– mice and levels below the assay sensitivity in Smst–/– mice. (d) Hemicoronal hypothalamic sections at the level of the periventricular nucleus (PeVN) and anterior paraventricular nucleus (PVN) of an Smst+/+ and an Smst–/– male mouse were immunostained for SST. There is a dense network of immunopositive perikarya and fibers adjacent to the third ventricle (III) only in the Smst+/+ mouse. These signals were also absent after preadsorption of the antiserum with synthetic SST (data not shown). Bars = 100 μm. (e) The median eminence (me) of an Smst+/+ and an Smst –/– mouse were immunostained for SST prohormone. There is no detectable immunoreactivity in the external zone of the me in the Smst–/– mouse. (f) The arcuate nucleus (Arc) of an Smst+/+ and an Smst–/– male mouse immunostained for GHRH. Immunoreactive neuronal perikarya are indicated by the arrows. No difference is apparent between genotypes.
Because SST-containing neurons within the hypothalamus are most directly involved in neuroendocrine regulation, we examined this brain area for evidence of compensatory changes secondary to the loss of SST. Immunohistochemistry utilizing an SST-14–directed antiserum revealed a dense plexus of SST immunoreactive fibers and cell bodies within the periventricular (PeVN), paraventricular (PVN), arcuate (Arc), and ventromedial (VMH) nuclei of Smst+/+ mice. No specific reaction product was observed in the hypothalami of Smst–/– mice (Figure 1d), which appeared structurally normal based on Nissl and acetylcholinesterase stains (data not shown). A second antiserum raised against an epitope in the prohormone region of proSST (29) strongly labeled fibers in the external zone of the median eminence in Smst+/+ but not in Smst–/– mice (Figure 1e). Using a mouse GHRH antiserum, no apparent differences in either the number of GHRH-positive neuronal perikarya or density of fibers in the Arc (Figure 1f) were observed between Smst+/+ or Smst–/– mice (30).
Effects of sex and genotype on SST and SSTR expression.
Semiquantitative RT-PCR was used to determine whether SST and SSTR1-5 exhibited baseline sexual diergism in the mouse as reported previously for SSTR1 and 2 in rat (11), and whether the complete absence of SST would alter expression of the structurally related peptide CST or SSTRs in a sex-dependent pattern. There was a clear sexual diergism in SST gene expression in wild-type hypothalamus and pituitary gland; male mice had SST mRNA levels more than twofold those of female mice in both tissues, and no expression was detected in the Smst–/– mice (Table 1). In contrast, CST expression was similar between males and females in hypothalamus, undetectable in pituitary, and unchanged in the absence of SST (data not shown).
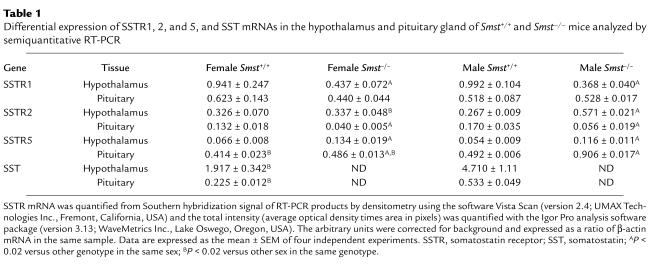
Table 1.
Differential expression of SSTR1, 2, and 5, and SST mRNAs in the hypothalamus and pituitary gland of Smst+/+ and Smst–/– mice analyzed by semiquantitative RT-PCR
A complex pattern of altered SSTR expression was detected in both tissues of Smst–/– mice (Table 1). SSTR1 expression decreased by more than 50% in the hypothalamus of both male and female Smst–/– mice but was unchanged in the pituitaries of these same mice. In contrast to the absence of sexual diergism in SSTR1 expression, there was a significant interaction between sex and genotype on the expression profiles of SSTR2 and 5. SSTR2 mRNA was increased more than twofold in the hypothalamus of Smst–/– males compared with Smst+/+ males but was decreased by about 70% in the pituitary of both sexes of Smst–/– mice. SSTR5 mRNA levels increased twofold in the hypothalamus of both sexes of Smst–/– mice in contrast to the twofold increase in pituitary SSTR5 expression that occurred only in Smst–/– males compared with Smst+/+ males. There were no differences between sexes or genotypes in SSTR3 and 4 mRNA quantitation (data not shown). An immunocytochemical analysis of SSTR expression showed no qualitative differences in receptor localization between genotypes (Figure 2, a–c). The intensity of immunostaining closely paralleled the relative mRNA levels, indicating that the semiquantitative RT-PCR accurately predicted the changes in SSTR abundance in the hypothalamus.
Figure 2.
SST receptor expression is altered in the hypothalamus of SST-deficient mice. (a) SSTRs were analyzed by peroxidase immunohistochemistry and the reaction product developed with diaminobenzidine. The hemicoronal hypothalamic sections are at the level of the median eminence (me). Immunoreactive SSTR1 is expressed in the arcuate nucleus (Arc), ventromedial nucleus (VMH), and dorsomedial nucleus (DMH) of both sexes of Smst+/+ mice and similarly decreased in both sexes of Smst–/– mice. Bar = 100 μm. (b) Immunoreactive SSTR2 is expressed in both sexes of Smst+/+ mice and clearly increased in the Arc, VMH, and DMH of Smst–/– male mice. (c) Immunoreactive SSTR5 is very sparse in both sexes of Smst+/+ mice but moderately expressed, particularly in the DMH, of Smst–/– male mice. III, third ventricle.
Normal growth despite altered GH secretion in SST-deficient mice.
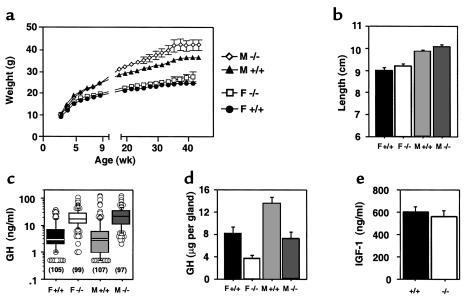
It was apparent from observation of the first litters of F2 mice that the absence of SST did not result in either gigantism or a loss of sexual dimorphism in body size. Growth curves obtained from both F2 (data not shown) and N5 mice (Figure 3a) confirmed this impression, although a gradual increase in body weight due to mild obesity did emerge for male Smst–/– mice after age 18 weeks [repeated measures ANOVA; F(1, 14) = 6.1, P < 0.05 main effect of genotype; F(10, 140) = 3.5, P < 0.001 genotype × time interaction]. Smst–/– mice exhibited the normal sexual dimorphism in body length that becomes evident during puberty, and there was no significant increase in body length for either sex of Smst–/– mice compared with their sibling controls (Figure 3b). Organ weights of liver and kidney were also normal in Smst–/– mice (data not shown).
Figure 3.
SST-deficient mice retain a normal sexual dimorphism in body size but exhibit altered pituitary GH secretion. (a) Serial body weights of sibling Smst+/+ and Smst–/– mice (n = 16) generated from N5 B6 congenic Smst+/– parents demonstrate normal growth patterns. The small increase in weight of male Smst–/– mice after 18 weeks of age is due to increased white adipose tissue without organomegaly (n = 8) (data not shown). (b) Nose-to-anus body lengths of the mice in a at age 24 weeks are significantly different between sexes but not between genotypes. (c) Box plots of randomly obtained serum GH levels from N5 B6 congenic mice of each sex and genotype (n = 97–107) demonstrate significant differences among the median values of the four groups (P < 0.0001, Kruskal-Wallis test). Individual values in the upper and lower 10% of the population distributions are plotted as open circles. Data are expressed as nanograms per milliliter in terms of the mouse GH AFP10783B reference preparation. (d) Pituitary GH content at age 20 weeks (n = 4–7) of sibling Smst+/+ and Smst–/– mice generated from F2 hybrid Smst+/– parents is decreased by 50% in both sexes of Smst–/– mice. (e) Serum IGF-1 levels of the mice in d show no difference between genotypes when the data are collapsed across sex.
Direct measurement of pulsatile GH in the mouse, unlike the rat, has been hampered by technical difficulties of chronic blood sampling in unrestrained animals. In a single reported study, male and female mice showed equivalent pulse amplitudes, but approximately 1.5-fold greater pulse frequency in females (35). Therefore to determine whether SST deficiency was associated with altered GH secretion, we obtained randomly timed blood samples by rapid tail bleeds between the hours of 0500 and 2300 from adult male and female mice of both genotypes over the course of 6 days. A total of 408 plasma samples from 107 mice (26–28 per group) were assayed for GH (Figure 3c). The box plots demonstrate that male and female Smst+/+ mice had identical median GH levels of 3 ng/ml. Furthermore, the overall distribution of values was similar, with the exception that no female value was greater than 36 ng/ml whereas five of 107 male values ranged from 50 to 122 ng/ml. In marked contrast, the distribution of GH values was shifted higher for both male and female Smst–/– mice, which had medians of 21 and 17 ng/ml, respectively (P < 0.0001, Mann-Whitney U test for each paired comparison between Smst+/+ and Smst–/– groups). Less than 10% of the random GH values from Smst–/– mice were below 6 ng/ml compared with 75% for both sexes of Smst+/+ mice (χ2 = 166.1, P < 0.0001).
Pituitary size was unchanged between the Smst+/+ and Smst–/– male and female mice. However, pituitary GH content was reduced by 50% in both sexes of Smst–/– mice compared with sex-matched controls (F(3, 14) = 9.12, P ≤ 0.01 for each comparison) (Figure 3d), possibly reflecting an altered balance between GH synthesis and release. Despite the changes in plasma and pituitary GH, there was no difference for IGF-1 between Smst+/+ and Smst–/– mice [F(1, 21) = 0.25, P = 0.6] (Figure 3e).
To facilitate a comparison between the present data and that of MacLeod et al. (35), who directly measured pulsatile GH secretion in cannulated mice at 15-minute intervals over 8-hour periods, we performed Z transformations of our GH data sets and the values from MacLeod’s representative pulsatile GH profiles (three male and three female outbred CD-1 [ICR] mice; n = 99 data points for each sex; see original data in ref. 35). The Z transformation approximates a normal distribution for a data set and then calculates a Z score for each data point that is equivalent to the number of normalized SDs relative to the group mean. Each of the six Z-score histograms is skewed to the left (median < mean) and has a tail extending to the right by as much as 6 SDs (Figure 4). By visual inspection, the four Z-score histograms of male and female Smst+/+ mice and male and female ICR mice are most similar to each other, whereas the male and female Smst–/– mice appear to constitute a distinct set because of a greater proportion of 0 < Z < 1. The small percentages of extreme GH values constituting the positive tails (Z ≥ 1) represent the peak amplitudes of individual GH pulses in the MacLeod data sets. Even though the female ICR mice were directly shown to have a greater GH pulse frequency than male ICR mice (35), resulting in nominally larger fractions of Z scores ≥ 1 of 14/99 and 9/99, respectively (Figure 4, lower panels), a χ2 test of this comparison failed to indicate a significant difference (Fisher’s Exact P = 0.38) for the group sizes of n = 99.
Figure 4.
Z-score histograms demonstrate similar distributions of GH values in data sets obtained from randomly timed blood sampling (F+/+, M+/+, F–/–, and M–/–) or from serial blood sampling in cannulated mice (F [ICR] and M [ICR]). The GH profiles (n = 97–107 independent measurements per group) were approximated as standard normal distributions using a Z-transformation. The top four panels are the Z scores calculated for the GH data in Figure 3c. The bottom two panels are the Z scores calculated from the pulsatile GH profiles of wild-type ICR mice in Figure 1 by MacLeod et al. (35). The Z scores are grouped into bin sizes equal to 1 SD of the normalized mean for each group. The bell curve in each panel illustrates the probability of the standard normal distribution in comparison to the Z scores calculated from the experimental data.
Hepatic feminization in male SST-deficient mice.
To analyze further the alterations in GH secretory dynamics of the Smst–/– mice, we took advantage of the firmly established role of pulsatile GH in regulating sexual differentiation of the liver (17, 18). Northern blots were used to quantify mRNA levels of several GH-regulated genes, and the data were normalized to 18S RNA content (Figure 5). The male-predominant gene transcripts for both MUPs group I/II and III exhibited levels that were approximately fivefold higher in Smst+/+ male compared with Smst+/+ female mice [F(3, 20) = 48.40, P < 0.001]. However, there was a dramatic reduction in MUPs expression in Smst–/– male mice to levels indistinguishable from females. Identical results were found in a separate cohort of F2 hybrid mice (data not shown). A similar pattern of gene expression across the four groups was found for albumin, although the increase in Smst+/+ male compared to Smst+/+ female mice was less than twofold [F(3, 20) = 6.04, P < 0.01]. In contrast, prolactin receptor mRNA levels were more than threefold higher in Smst+/+ females compared with Smst+/+ males (P < 0.02, one-tailed t test), consistent with previously published results in mice for this typical female-predominant gene (36). The absence of SST resulted in an increase of prolactin receptor expression in Smst–/– male compared with Smst+/+ male mice [F(3, 20) = 4.91, P < 0.05] but no significant change in Smst–/– female mice. Finally, we analyzed expression of the female predominant Cyp450-15α2A4 mRNA in liver (34). Both Smst–/– male and female mice exhibited a significant increase in hybridization signal compared with Smst+/+ male mice [F(3, 20) = 6.13, P < 0.05 and < 0.01, respectively].
Figure 5.
GH-dependent hepatic gene expression is feminized in male SST-deficient mice. The phosphorimager scans of Northern blots below the graphs show three representative samples from each group. Volumetric quantitation of each hybridization signal is expressed as a ratio to the corresponding 18S RNA signal in arbitrary units (N5 B6 congenic mice, n = 6). MUPs I, II, and III and albumin mRNA levels are depressed in male Smst–/– mice to levels equivalent with all females. In contrast, levels of the female predominant transcripts for PrlR and CYP2A4 are significantly increased in male Smst–/– mice to levels equal or greater than female Smst+/+ mice. Although the cDNA probe used to hybridize with Cyp450-15α2A4 mRNA also detects a related, but not sexually diergic, Cyp450-15α2A5 transcript of identical size (34), the increased hybridization signal is presumably due only to a rise in the GH regulated 2A4 transcript. Prolactin receptor, PrlR; Cyp450-15α2A4/5, CYP2A4.
When all five of the sexually diergic hepatic mRNAs are considered together, there is a compelling pattern of feminization in the liver of Smst–/– male mice compared to wild types, without reciprocal changes in the Smst–/– female mice. These differences are not due to alterations in circulating sex steroids in the male mutants because we found no significant differences between genotypes for either serum testosterone [Smst+/+ males, 4.6 ± 1.7 ng/ml vs. Smst–/–males, 7.4 ± 2.0 ng/ml; F(1, 30)=1.19, P = 0.28] or estradiol [Smst+/+ males, 2.0 ± 0.6 pg/ml vs. Smst–/–males, 9.1 ± 4.5 pg/ml; F(1, 30)=2.48, P = 0.13]. SST receptors are also localized on pituitary thyrotrophs and SST can inhibit thyroid-stimulating hormone secretion, however serum thyroxine levels did not differ between sexes or genotypes (Smst+/+ mice, 3.4 ± 0.4 μg/dl vs. Smst–/– mice, 3.7 ± 0.4 μg/dl).
Discussion
SST is synthesized in neural, endocrine and inflammatory cells in the brain and periphery and acts on multiple targets through a family of five receptors, SSTR1-5, to produce a broad spectrum of biologic effects (reviewed in ref. 10). However, many questions still remain concerning the physiological function of SST especially in the brain. Our present studies were undertaken to create a mouse model of complete SST deficiency from which we could infer the functions of the peptide by an analysis of the phenotype resulting from its absence. A primary aim was to determine the effects of chronic SST deficiency on GH secretion and test the hypothesis that male SST-deficient mice would exhibit a more altered phenotype than females because of the normally greater SST expression in male hypothalamus. Smst–/– mice were investigated on both an F2 hybrid and incipient congenic C57BL/6J genetic background, and equivalent results were obtained in both strains, indicating that our results are unlikely to have been biased by selective epistatic interactions of the Smst gene mutation with other gene alleles from either of the genetic backgrounds.
The direct measurement of GH pulsatility in mice represents a formidable challenge and has been reported by only one laboratory (35) to our knowledge. Our approach to this problem relied on obtaining sufficiently large data sets (n ≅ 100 per group) of randomly timed plasma GH levels to approximate the true distribution of values that might be obtained by serial measurement of GH from cannulated animals in a formal pulse-analysis study. The approach was validated by a comparison of our data from Smst+/+ mice with those of the representative GH secretory profiles in wild-type mice published by MacLeod et al. (35) following Z-transformations to normalize each data set (Figure 4). It is apparent that the bona fide pulsatile GH data represented in the bottom two panels have positively skewed (median < mean), non-Gaussian probability distributions. The peak values from GH pulses in both the male and female ICR mice are represented by Z scores ≥ 1 in the histogram tails. The highly similar distributions of Z scores between the C57BL/6 Smst+/+ and MacLeod’s ICR mice suggest that the C57BL/6 Smst+/+ mice secrete GH in a pulsatile rhythm that is similar to the ICR mice and characterized by large amplitude pulses and low interpulse nadir levels in both sexes.
In contrast to the Smst+/+ mice, male and female Smst–/– mice had very few random GH levels < 3 ng/ml and clearly elevated median GH levels, but the maximal amplitude of GH was not changed. The Z-score distributions were similar to the Smst+/+ and wild-type ICR mice based on positive skew and the presence of tails ≥ 1, but differed in their larger fraction of scores between 0 and 1. These data suggest that Smst–/– mice continue to secrete GH in a pulsatile rhythm, although SST is apparently required to inhibit GH secretion between GHRH pulses and thereby maintain low nadir interpulse GH levels. The decreased pituitary content of GH is also consistent with increased secretion of GH into the circulation. However, the Z-transformed data sets do not have sufficient statistical power to conclude whether the frequency of GH pulses is altered in the Smst–/– mice.
Experiments in rats and mice have demonstrated that there are at least two groups of hepatic genes whose sexually diergic expression is GH dependent, but which differ in the mechanism of GH regulation. Male-predominant genes, including MUPs and the cytochrome P450 Cyp2d9, are directly activated by pulses of GH secretion separated by relatively long intervals during which GH levels are below 1–2 ng/ml (18, 19). This activation of male-predominant genes is prevented by either the absence of circulating GH, or conversely, continuous infusion of GH and subsequent desensitization of the GH receptor-JAK2/STAT5 signaling complex. Interestingly, even a subtle increase in GH pulse frequency from six to seven per day, delivered by cannula to hypophysectomized rats, does not support the activation of male-predominant genes presumably because of the shortened interpulse interval and suboptimal GH receptor resensitization (18). In male mice, the intermittent GH pulses also directly repress expression of female-specific genes including the cytochrome P450 Cyp2a4 by an unknown mechanism (19). Transcriptional regulation of these same genes differs in female liver in which there is a constitutive activation of female-specific genes (Cyp2a4) and repression of male-specific genes (Cyp2d9) that is independent of pituitary GH (37). An important factor contributing to the female pattern is normal expression of estrogen receptor-α, presumably because of its importance in establishing the sexually dimorphic patterns of GH secretion (34).
Male SST-deficient mice exhibit a striking reduction in expression of the male-specific genes encoding MUPs to levels equivalent with normal females. This is clearly not due to the absence of GH, testosterone, or thyroxine and, therefore, is strong confirmatory evidence that the normal male pattern of pulsatile GH secretion is altered in the male Smst–/– mice. The transformation could be due solely to elevated interpulse levels of GH, consistent with the measured random GH levels. However, it is also possible that GH pulse frequency is increased according to the model of Tannenbaum that predicts an intrinsic once-per-hour pulsatility of GHRH in the absence of a SST-mediated short-loop feedback inhibition from GH (1). Further studies using cannulated mice will be necessary to definitively demonstrate altered GH pulse frequency in the SST-deficient mice. That IGF-1 levels are not elevated in SST-deficient mice suggests that an increase in time-integrated GH secretion may be counteracted by a decrease in GH responsiveness. A loss of the normal male-like pattern of GH pulsatility is also sufficient to explain the increased expression of Cyp2a4 and prolactin receptor genes in the male SST-deficient mice because these gene promoters would no longer be subject to the transcriptional repression associated with high-amplitude pulses separated by long interpulse nadirs. However, the supranormal levels of both Cyp2a4 and prolactin receptor mRNAs in female Smst–/– compared with Smst+/+ mice further suggests the increased activation of these genes by an unidentified mechanism in addition to derepression.
STAT5b-knockout mice exhibit a similar change in GH-dependent sexually diergic gene expression compared with the SST-deficient mice, but differ importantly in their somatic growth (19, 20). Unlike STAT5b knockouts, both sexes of SST-deficient mice have normal pubertal growth and retain their sexual dimorphism in body weight and length. There are several possibilities to resolve this apparent discrepancy including a reduction in circulating IGF-1 in the STAT5b-deficient males. Decreased IGF-1 was also reported in female STAT5b-deficient mice in one study (19, 20), but normal levels were demonstrated in an independently generated strain, possibly because of STAT5b-independent ovarian IGF-1 production (19, 20). Both male and female SST-deficient mice had normal levels of IGF-1, suggesting that the altered secretion of GH that caused feminization of the liver was still sufficient for normal IGF-1 production in both sexes. Second, we measured a fraction of the genes known to be regulated by GH in liver, so it is possible that the change in GH secretion of SST-deficient mice feminized the expression of fewer genes than did the absence of STAT5b. Additionally, there may be other nonhepatic effects of GH important for sexual dimorphism in body mass that are sensitive to the absence of STAT5b but not to changes in GH pulsatility. Finally, the deletion of STAT5b has polymorphic effects because it is a component of the signaling complex for several tyrosine kinase receptors (20).
Our results also contrast with the dichotomy between GH-dependent liver gene expression and somatic growth reported by Waxman et al. (18) using cannulated rats. They demonstrated that seven GH pulses per day resulted in increased body weight gain over 1 week in both sexes of hypophysectomized rats that was indistinguishable from normal male rats. As noted above, this GH profile was not recognized by the liver as masculine because it failed to induce expression of the male-specific CYP2C11, nor was it recognized as feminine because it did not stimulate the female predominant steroid 5α-reductase or suppress the male-specific CYP3A2-dependent testosterone 6β-hydroxylase. Continuous infusion of GH was required to fully feminize liver gene expression in male rats, but this latter GH profile resulted in body weight gain of the males that was reduced to the normal female level. Therefore, although these data also indicate disassociations among GH secretory profiles, patterns of GH-dependent liver gene expression, and somatic growth, none of the experimentally produced GH profiles in hypophysectomized rats preserved a sexually dimorphic growth response while simultaneously altering liver gene expression as we observed in the SST-deficient mice. These differences might be attributed to true species-specific idiosyncrasies between rat and mouse in their respective GH-hepatic axes or to experimental differences including the length of time that body weight was recorded or the combined actions of pituitary hormones other than GH and their effects on gonadal and adrenal steroid hormones.
Despite the well-established role of SST as the inhibitory regulator of GH secretion and an important therapeutic role of SST-analogues in the treatment of GH-secreting pituitary tumors, SST-deficient mice up to 2 years of age did not exhibit a clinical syndrome of GH excess or develop somatotroph hyperplasia or adenoma. In contrast, overexpression of the stimulatory peptide GHRH in either mice or humans (38, 39) leads to significantly increased numbers of pituitary somatotrophs and a syndrome of gigantism or acromegaly. Taken together, these findings suggest that SST does not play a critical physiological role to tonically inhibit somatotroph mitogenesis in response to stimulatory growth factors. This situation is unlike the marked proliferation of lactotrophs that occurs after genetic disinhibition from the analogous dopamine and D2 receptor signaling pathway (40, 41). Alternatively, the absence of SST may be accompanied by a compensatory decrease in the mitogenic signal from GHRH that was not detected at the level of immunohistochemical detection of GHRH neurons in the hypothalamus.
In summary, we have examined the physiological role of SST in the regulation of GH secretion by a gene-knockout approach. The absence of SST results in elevated nadir and median GH levels in both sexes and a feminized pattern of GH-dependent gene expression in the liver of male mice. Despite the magnitude of these changes, Smst–/– mice do not exhibit increased IGF-1 levels or gigantism, and they retain a normal sexual dimorphism in postnatal somatic growth. Within the hypothalamus and pituitary, the loss of SST had pleiotropic effects on the expression of different SSTR subtypes. Only SSTR2 and SSTR5 exhibited a male-specific increase in mRNA levels in SST-deficient mice, consistent with a higher functional SST tone in the hypothalamus of male compared with male mice. We conclude that SST is required to determine the normal secretory profile of GH in both sexes of mice and specifically to masculinize GH secretion. However, our data indicate that typical masculinized profiles of GH pulsatility and GH-dependent hepatic gene expression are not necessary for the greater somatic growth characteristics of male compared with female animals after puberty.
Acknowledgments
We thank E.C. Chan for culture of embryonic stem cells, R. Juarez for blastocyst injections and preliminary experiments, D. Robins for advice and the generous gift of MUP oligonucleotides, K. Nusser and S. Lapostelle for technical assistance, R. Lechan and F. Talamantes for antisera, M. Negishi for a Cyp 450-15α4A cDNA, P. Kelly for a PrlR cDNA, D. Hess for steroid hormone RIAs, C. Emerson for the T4 RIA, and R. Cone for a critical reading of the manuscript. This work was supported by grants to M.J. Low from the Lucille P. Markey Charitable Trust, the Medical Research Foundation of Oregon, and the Robert Wood Johnson Foundation, and to Y.C. Patel from the NIH (NS32160) and the Canadian Institutes of Health Research. Requests for mouse GH RIA immunoreagents should be addressed to A.F. Parlow (e-mail: parlow@humc.edu; website: http://www.humc.edu/hormones).
Footnotes
Malcolm J. Low and Veronica Otero-Corchon contributed equally to this work.
References
- 1.Wagner C, Caplan SR, Tannenbaum GS. Genesis of the ultradian rhythm of GH secretion: a new model unifying experimental observations in rats. Am J Physiol. 1998;275:E1046–E1054. doi: 10.1152/ajpendo.1998.275.6.E1046. [DOI] [PubMed] [Google Scholar]
- 2.Smith RG, Feighner S, Prendergast K, Guan X, Howard A. A new orphan receptor involved in pulsatile growth hormone release. Trends Endocrinol Metab. 1999;10:128–135. doi: 10.1016/s1043-2760(98)00132-5. [DOI] [PubMed] [Google Scholar]
- 3.Plotsky PM, Vale W. Patterns of growth hormone-releasing factor and somatostatin secretion into the hypophysial-portal circulation of the rat. Science. 1985;230:461–463. doi: 10.1126/science.2864742. [DOI] [PubMed] [Google Scholar]
- 4.Jansson JO, Eden S, Isaksson O. Sexual dimorphism in the control of growth hormone secretion. Endocr Rev. 1985;6:128–150. doi: 10.1210/edrv-6-2-128. [DOI] [PubMed] [Google Scholar]
- 5.Jaffe CA, et al. Regulatory mechanisms of growth hormone secretion are sexually dimorphic. J Clin Invest. 1998;102:153–164. doi: 10.1172/JCI2908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chowen-Breed JA, Steiner RA, Clifton DK. Sexual dimorphism and testosterone-dependent regulation of somatostatin gene expression in the periventricular nucleus of the rat brain. Endocrinology. 1989;125:357–362. doi: 10.1210/endo-125-1-357. [DOI] [PubMed] [Google Scholar]
- 7.Murray HE, Simonian SX, Herbison AE, Gillies GE. Correlation of hypothalamic somatostatin mRNA expression and peptide content with secretion: sexual dimorphism and differential regulation by gonadal factors. J Neuroendocrinol. 1999;11:27–33. doi: 10.1046/j.1365-2826.1999.00286.x. [DOI] [PubMed] [Google Scholar]
- 8.Nurhidayat Tsukamoto Y, Sigit K, Sasaki F. Sex differentiation of growth hormone-releasing hormone and somatostatin neurons in the mouse hypothalamus: an immunohistochemical and morphological study. Brain Res. 1999;821:309–321. doi: 10.1016/s0006-8993(99)01081-1. [DOI] [PubMed] [Google Scholar]
- 9.Murray HE, Simonian SX, Herbison AE, Gillies GE. Ontogeny and sexual differentiation of somatostatin biosynthesis and secretion in the hypothalamic periventricular-median eminence pathway. J Neuroendocrinol. 1999;11:35–42. doi: 10.1046/j.1365-2826.1999.00287.x. [DOI] [PubMed] [Google Scholar]
- 10.Patel YC. Somatostatin and its receptor family. Front Neuroendocrinol. 1999;20:157–198. doi: 10.1006/frne.1999.0183. [DOI] [PubMed] [Google Scholar]
- 11.Zhang WH, Beaudet A, Tannenbaum GS. Sexually dimorphic expression of sst1 and sst2 somatostatin receptor subtypes in the arcuate nucleus and anterior pituitary of adult rats. J Neuroendocrinol. 1999;11:129–136. doi: 10.1046/j.1365-2826.1999.00295.x. [DOI] [PubMed] [Google Scholar]
- 12.Kimura N, Tomizawa S, Arai KN. Chronic treatment with estrogen up-regulates expression of sst2 messenger ribonucleic acid (mRNA) but down-regulates expression of sst5 mRNA in rat pituitaries. Endocrinology. 1998;139:1573–1580. doi: 10.1210/endo.139.4.5952. [DOI] [PubMed] [Google Scholar]
- 13.Senaris RM, Lago F, Dieguez C. Gonadal regulation of somatostatin receptor 1, 2 and 3 mRNA levels in the rat anterior pituitary. Brain Res Mol Brain Res. 1996;38:171–175. doi: 10.1016/0169-328x(96)00042-3. [DOI] [PubMed] [Google Scholar]
- 14.Painson JC, Thorner MO, Krieg RJ, Tannenbaum GS. Short-term adult exposure to estradiol feminizes the male pattern of spontaneous and growth hormone-releasing factor-stimulated growth hormone secretion in the rat. Endocrinology. 1992;130:511–519. doi: 10.1210/endo.130.1.1345780. [DOI] [PubMed] [Google Scholar]
- 15.Painson JC, Veldhuis JD, Tannenbaum GS. Single exposure to testosterone in adulthood rapidly induces regularity in the growth hormone release process. Am J Physiol Endocrinol Metab. 2000;278:E933–E940. doi: 10.1152/ajpendo.2000.278.5.E933. [DOI] [PubMed] [Google Scholar]
- 16.McIntosh I, Bishop JO. Differential expression in male and female mouse liver of very similar mRNAs specified by two group 1 major urinary protein genes. Mol Cell Biol. 1989;9:2202–2207. doi: 10.1128/mcb.9.5.2202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sundseth SS, Alberta JA, Waxman DJ. Sex-specific, growth hormone-regulated transcription of the cytochrome P450 2C11 and 2C12 genes. J Biol Chem. 1992;267:3907–3914. [PubMed] [Google Scholar]
- 18.Waxman DJ, Pampori NA, Ram PA, Agrawal AK, Shapiro BH. Interpulse interval in circulating growth hormone patterns regulates sexually dimorphic expression of hepatic cytochrome P450. Proc Natl Acad Sci USA. 1991;88:6868–6872. doi: 10.1073/pnas.88.15.6868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Udy GB, et al. Requirement of STAT5b for sexual dimorphism of body growth rates and liver gene expression. Proc Natl Acad Sci USA. 1997;94:7239–7244. doi: 10.1073/pnas.94.14.7239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Teglund S, et al. Stat5a and Stat5b proteins have essential and nonessential, or redundant, roles in cytokine responses. Cell. 1998;93:841–850. doi: 10.1016/s0092-8674(00)81444-0. [DOI] [PubMed] [Google Scholar]
- 21.Davey HW, Park SH, Grattan DR, McLachlan MJ, Waxman DJ. STAT5b-deficient mice are growth hormone pulse-resistant. Role of STAT5b in sex-specific liver p450 expression. J Biol Chem. 1999;274:35331–35336. doi: 10.1074/jbc.274.50.35331. [DOI] [PubMed] [Google Scholar]
- 22.Davey HW, Wilkins RJ, Waxman DJ. STAT5 signaling in sexually dimorphic gene expression and growth patterns. Am J Hum Genet. 1999;65:959–965. doi: 10.1086/302599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Park SH, Liu X, Hennighausen L, Davey HW, Waxman DJ. Distinctive roles of STAT5a and STAT5b in sexual dimorphism of hepatic P450 gene expression. Impact of STAT5a gene disruption. J Biol Chem. 1999;274:7421–7430. doi: 10.1074/jbc.274.11.7421. [DOI] [PubMed] [Google Scholar]
- 24.Waxman, D.J., and Chang, T.K.H. 1995. Hormonal regulation of liver cytochrome P450 enzymes. In Cytochrome P450: structure, mechanism, and biochemistry. 2nd edition. P.R. Oritiz de Montellano, editor. Plenum Press. New York, New York, USA/London, United Kingdom. 391–417.
- 25.Zheng H, et al. Somatostatin receptor subtype 2 knockout mice are refractory to growth hormone-negative feedback on arcuate neurons. Mol Endocrinol. 1997;11:1709–1717. doi: 10.1210/mend.11.11.0016. [DOI] [PubMed] [Google Scholar]
- 26.Kreienkamp HJ, Akgun E, Baumeister H, Meyerhof W, Richter D. Somatostatin receptor subtype 1 modulates basal inhibition of growth hormone release in somatotrophs. FEBS Lett. 1999;462:464–466. doi: 10.1016/s0014-5793(99)01582-3. [DOI] [PubMed] [Google Scholar]
- 27.Low MJ, et al. Tissue-specific posttranslational processing of pre-prosomatostatin encoded by a metallothionein-somatostatin fusion gene in transgenic mice. Cell. 1985;41:211–219. doi: 10.1016/0092-8674(85)90075-3. [DOI] [PubMed] [Google Scholar]
- 28.Rubinstein M, Japon MA, Low MJ. Introduction of a point mutation into the mouse genome by homologous recombination in embryonic stem cells using a replacement type vector with a selectable marker. Nucleic Acids Res. 1993;21:2613–2617. doi: 10.1093/nar/21.11.2613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lechan RM, Goodman RH, Rosenblatt M, Reichlin S, Habener JF. Prosomatostatin-specific antigen in rat brain: localization by immunocytochemical staining with an antiserum to a synthetic sequence of preprosomatostatin. Proc Natl Acad Sci USA. 1983;80:2780–2784. doi: 10.1073/pnas.80.9.2780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Phelps CJ, Dalcik H, Endo H, Talamantes F, Hurley DL. Growth hormone-releasing hormone peptide and mRNA are overexpressed in GH-deficient Ames dwarf mice. Endocrinology. 1993;133:3034–3037. doi: 10.1210/endo.133.6.7694848. [DOI] [PubMed] [Google Scholar]
- 31.Kumar U, Laird D, Srikant CB, Escher E, Patel YC. Expression of the five somatostatin receptor (SSTR1-5) subtypes in rat pituitary somatotrophes: quantitative analysis by double-layer immunofluorescence confocal microscopy. Endocrinology. 1997;138:4473–4476. doi: 10.1210/endo.138.10.5566. [DOI] [PubMed] [Google Scholar]
- 32.Khare S, et al. Differential regulation of somatostatin receptor types 1-5 in rat aorta after angioplasty. FASEB J. 1999;13:387–394. doi: 10.1096/fasebj.13.2.387. [DOI] [PubMed] [Google Scholar]
- 33.Ormandy CJ, et al. Null mutation of the prolactin receptor gene produces multiple reproductive defects in the mouse. Genes Dev. 1997;11:167–178. doi: 10.1101/gad.11.2.167. [DOI] [PubMed] [Google Scholar]
- 34.Sueyoshi T, Yokomori N, Korach KS, Negishi M. Developmental action of estrogen receptor-alpha feminizes the growth hormone-Stat5b pathway and expression of Cyp2a4 and Cyp2d9 genes in mouse liver. Mol Pharmacol. 1999;56:473–477. doi: 10.1124/mol.56.3.473. [DOI] [PubMed] [Google Scholar]
- 35.MacLeod JN, Pampori NA, Shapiro BH. Sex differences in the ultradian pattern of plasma growth hormone concentrations in mice. J Endocrinol. 1991;131:395–399. doi: 10.1677/joe.0.1310395. [DOI] [PubMed] [Google Scholar]
- 36.Norstedt G, Palmiter R. Secretory rhythm of growth hormone regulates sexual differentiation of mouse liver. Cell. 1984;36:805–812. doi: 10.1016/0092-8674(84)90030-8. [DOI] [PubMed] [Google Scholar]
- 37.Yoshioka H, et al. Characterization and regulation of sex-specific mouse steroid hydroxylase genes. Can J Physiol Pharmacol. 1990;68:754–761. doi: 10.1139/y90-116. [DOI] [PubMed] [Google Scholar]
- 38.Kovacs M, et al. Effects of antagonists of growth hormone-releasing hormone (GHRH) on GH and insulin-like growth factor I levels in transgenic mice overexpressing the human GHRH gene, an animal model of acromegaly. Endocrinology. 1997;138:4536–4542. doi: 10.1210/endo.138.11.5498. [DOI] [PubMed] [Google Scholar]
- 39.Thorner MO, et al. Extrahypothalamic growth-hormone-releasing factor (GRF) secretion is a rare cause of acromegaly: plasma GRF levels in 177 acromegalic patients. J Clin Endocrinol Metab. 1984;59:846–849. doi: 10.1210/jcem-59-5-846. [DOI] [PubMed] [Google Scholar]
- 40.Kelly MA, et al. Pituitary lactotroph hyperplasia and chronic hyperprolactinemia in dopamine D2 receptor-deficient mice. Neuron. 1997;19:103–113. doi: 10.1016/s0896-6273(00)80351-7. [DOI] [PubMed] [Google Scholar]
- 41.Asa SL, Kelly MA, Grandy DK, Low MJ. Pituitary lactotroph adenomas develop after prolonged lactotroph hyperplasia in dopamine D2 receptor-deficient mice. Endocrinology. 1999;140:5348–5355. doi: 10.1210/endo.140.11.7118. [DOI] [PubMed] [Google Scholar]