Abstract
The impact of caregiver education level on endorsement of attention-deficit hyperactivity disorder (ADHD) symptoms for inattention (IA) and hyperactivity-compulsivity (HA) in a sample of high-risk youths was examined. Participants were 1347 caregivers of varying educational backgrounds who completed the ADHD module of the Diagnostic Interview Schedule for Children IV. The relationship of caregiver education to ADHD symptom endorsement was examined in three sets of analyses in which IA and HA symptoms were simultaneously regressed on caregiver years of education. Both multivariate analysis of covariance and logistic regression analyses revealed significantly lower rates of IA symptom endorsement by caregivers with less education, while there was no effect for HA symptoms. A multiple indicator multiple cause (MIMIC) model analysis also revealed that caregiver years of education was significantly positively associated with IA but not with HA symptoms, even when other demographic factors were controlled. There is a clear effect of caregiver education on ADHD symptom endorsement patterns, raising concerns that demographic factors related to symptom measurement may contribute to discrepancies in the assessment and treatment of ADHD.
Accuracy in the measurement of psychiatric symptoms is usually considered in terms of the reliability and validity of a specific measure. There has been less attention focused on how endorsement of specific types of symptoms and instrument characteristics can vary as a function of respondent characteristics. Furthermore, it is assumed that the set of symptoms that comprise a diagnostic category should be endorsed in a similar way across populations.
Attention-deficit hyperactivity disorder (ADHD) provides an excellent context in which to consider the question of differential symptom endorsement as a function of demographic variables. Factor analytic studies have demonstrated that there are two factors that underlie ADHD, inattention (IA) and hyperactivity/impulsivity (HA),1-4 and there may be differential endorsement of symptoms that comprise these factors. Although most structured interviews and rating scales attempt to phrase questions in a manner that will be understandable to a range of respondents, the validity of an instrument designed to measure symptoms may nevertheless be influenced by a respondent's ability to conceptualize and identify a range of behaviors.
In the case of ADHD, it is possible that caregivers more readily understand and detect hyperactive or impulsive symptoms of ADHD, while it may be more difficult for many caregivers to conceptualize and recognize behaviors that index attention problems. For example, it may be easier to recognize that a child has a symptom such as “often fidgets with hands or feet,” while it may be more problematic to detect and report if a child is “distracted by extraneous stimuli.” This report examines how caregiver educational attainment affects the endorsement of symptoms of IA and HA in the Diagnostic Interview Schedule for Children Version IV (DISC-IV) in a large sample of caregivers of high-risk youths. This issue is important, as typical measures of validity associated with diagnostic categories and diagnostic instruments may not capture “bias” in the sense of differential symptom endorsement according to racial/ethnic or sociodemographic characteristics of the respondent.
To gauge whether differences in symptom profile or clinical presentation might exist as a function of factors such as socioeconomic status (SES) or parental educational attainment, we considered the results of previous studies that report on prevalence differences in ADHD. To our knowledge, parent education in relation to the report of ADHD symptoms of their children has been studied only indirectly as a part of SES. Studies on the effects of SES have found higher rates of ADHD in children from lower SES backgrounds.5,6 It is not clear whether this link is part of a larger hypothesized causal pathway between lower SES and the ensuing stressful climate of families and individuals. Stress has been associated with higher levels of psychopathology, including ADHD.7,8 Barkley9 explains the higher incidence of ADHD in low SES populations in terms of a theory of “social drift” in which individuals with ADHD are considered less likely to benefit from education than those without ADHD and therefore tend to inhabit lower SES brackets. Furthermore, high rates of heritability of ADHD and the relative stability of SES across generations10 may also contribute to the higher incidence of ADHD in lower SES groups. However, differential endorsement of IA versus HA symptoms or the prevalence of ADHD subtypes has not been examined.
Broad studies of the relationship between parental education and child psychopathology symptom endorsement suggest an inverse relationship. Based on the relatively few studies examining the relationship between ADHD and SES and the more general relationships found between parent educational attainment and problem behaviors in children, a higher rate of endorsement of ADHD symptoms would be expected in samples of caregivers with less education. That is, caregiver education would be expected to relate to IA and HA symptoms in the same way and would predict a minimal association between the endorsement of ADHD symptoms and caregiver education. However, if the IA symptoms of ADHD are more difficult to understand or report, parental educational attainment may differentially affect rates of endorsement of IA symptoms, while the relationship between caregiver education and endorsement of HA symptoms may be weaker or nonexistent when controlling for other factors.
The present study examined the effect of caregiver education on endorsement of IA and HA symptoms in a representative sample of youths in public service sectors. Based on clinical observation, we hypothesized that caregivers with higher educational attainment would be more likely to endorse IA symptoms in a structured diagnostic assessment. Specifically, we predicted that (1) higher caregiver education would be associated with the number of IA symptoms endorsed while being unrelated to the number of HA symptoms endorsed, (2) higher caregiver education would be associated with endorsement of individual IA but not HA symptoms, and (3) in a comprehensive model simultaneously controlling for demographics and multiple comparisons, higher caregiver education would be associated with a latent IA factor but not a latent HA factor. We predicted that all these relationships would be found when controlling for caregiver ethnicity and youth age and gender.
METHODS
Participants
Participants were from the Patterns of Youth Mental Health Care in Public Service Systems (POC) study that included a random sample of 1715 children and adolescents ages 6 to 17 years from open cases of youths active in one or more of five San Diego County public sectors of care during the second half of fiscal year 1996–1997 (see Aarons et al11 and Garland et al12 for detailed descriptions). All children and youths ages 6–17 years of age who had received services in alcohol and drug, mental health, school SED (i.e., severely emotionally disturbed), child welfare, and juvenile justice services were included in the eligible sampling frame. In juvenile justice and child welfare, only children whose placement was under court jurisdiction were included. Between October 1997 and January 1999, interviews were completed for 1715 youths. Participants did not differ significantly from nonparticipants in regard to age, gender, sector affiliation, or race/ethnic distribution except that slightly fewer Asians participated relative to the eligible sample. The sample was stratified by service sector affiliation, race/ethnicity, and level of restrictiveness of treatment setting (i.e., home versus aggregate care setting).
The subsample for the present study included 1347 caregivers of youths in the POC study who completed the DISC-IV (described below). Table 1 displays relevant demographic data for both youths and caregivers. The majority of the youths were male (65.3%). The majority of the parent/caregiver informants were biological parents (80%). Others included close relatives, foster caregivers, adoptive/stepparents, and professional caregivers. The mean caregiver age was 43.1 years, with a majority of female participants (90.1%), and the racial/ethnic distribution of caregivers was as follows: white, 48.8%; Latino, 17.2%; African-American, 20.8%; Asian-American/Pacific Islander, 4.0%; mixed ethnicity, 3.4%; and other, 4.3% (missing 1.5%). The mean of caregiver education was 12.6 years; percentages of caregivers in each educational category are shown in Table 1.
Table 1.
Demographic Characteristics of the POC Study Subsample
| (N = 1347) | |
|---|---|
| Youth gender (% male) | 65% |
| Youth age (yr), mean (SD) | 13.68 (3.29) |
| 6–12 | 36% |
| 13–15 | 23% |
| 16–18 | 41% |
| Youth past year diagnosis of ADHD (DISC-IV) | 28% |
| Caregiver race/ethnicity (% white) | 49% |
| Caregiver age (yr) mean (SD) | 43.1 (0.27) |
| Caregiver education (yr) mean (SD) | 12.60 (2.17) |
| No degree | 19% |
| GED or high school | 34% |
| Vocational, technical, or A.A. degree | 34% |
| B.A. degree or advanced | 12% |
| Caregiver relationship to youth | |
| Biological parent | 7% |
| Adoptive or step parent | 6% |
| Close relative | 12% |
| Other (foster parent, professional caregiver) | 12% |
POC, Patterns of Youth Mental Health Care in Public Service Systems; ADHD, attention-deficit hyperactivity disorder; DISC-IV, Diagnostic Interview Schedule for Children Version IV; GED, General Education Diploma.
Measures
Demographics were assessed as part of our structured assessment of need for services and service use. Caregiver education was collected by self-report and categorized into eight categories, ranging from less than eighth grade to completion of an advanced degree.
DISC-IV
The DISC-IV (Shaffer et al13) is considered a reliable and valid measure for research purposes, and the ADHD module also has demonstrated good validity and reliability.14,15 The DISC-IV is a highly structured diagnostic interview designed to yield DSM-IV–based diagnoses through computer algorithm scoring. The DISC-IV has demonstrated reliability and validity comparable to that of other diagnostic measures.15
Procedures
Comprehensive computer-assisted interviews of the caregivers about their need for and use of mental health services were conducted by nonclinician interviewers with at least an undergraduate college degree. Interviewers completed approximately 100 hours of training on the specific instruments, standardized interviewing practices, and cultural competence. Bimonthly quality assurance checks were conducted, and interviewers were observed in the field quarterly by study investigators who provided feedback and remediation if needed. Most interviews were conducted in the participants' homes (87%), and different interviewers conducted caregiver and youth interviews to ensure confidentiality and increase the likelihood of accurate self-disclosure. Caregivers received $40 for participation and youths received between $10 and $40 depending on age (related to length of interview). Informed consent was obtained from parents and assent from youths, each being assured of confidentiality verbally and through consent/assent procedures and with a federal Certificate of Confidentiality for any information volunteered in the interview.
Analyses
A three-phase data analytic approach was taken in the present study. First, to test Hypothesis 1, we conducted a multivariate analysis of variance including important covariates to determine whether there was an effect of caregiver education on the number of IA and HA symptoms endorsed. Second, to test Hypothesis 2, we conducted a series of logistic regressions regressing each of the IA and HA symptoms separately on caregiver education while controlling for covariates. Third, to assess our hypotheses in a more comprehensive fashion and specifically to test Hypothesis 3, we developed and tested a multiple indicator multiple cause (MIMIC) model using estimation procedures appropriate for the dichotomous nature of the dependent variables. This analysis allowed a more comprehensive test of our theoretical model with all variables simultaneously in the model along with covariates.16,17 Results reported in this article are based on data that have been weighted to adjust for variation in sample selection as well as survey nonresponse and other potential sources of survey error.
RESULTS
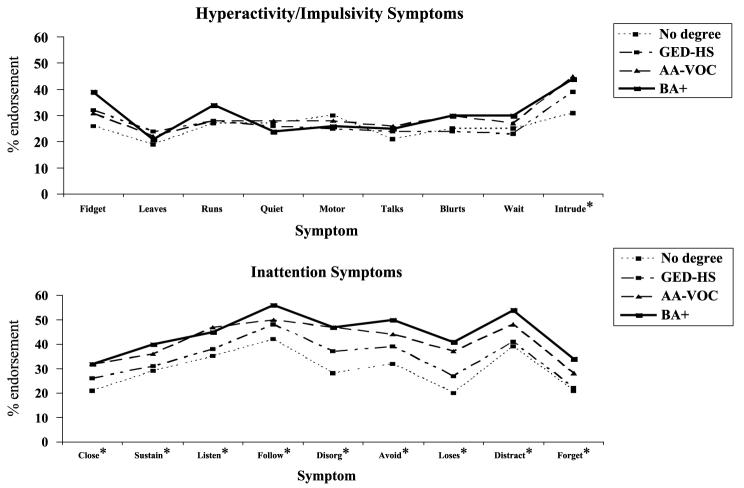
For the total sample, an average of 3.32 (SD = 3.11) hyperactivity (HA) symptoms and 2.52 (SD = 2.81) inattention (IA) symptoms were endorsed. Figure 1 illustrates rates of symptom endorsement as the percentage of caregivers at each of four levels of education (no degree; GED [General Education Diploma] or high school; A.A. degree/vocational; B.A. degree or above), endorsing each item of the HA and IA symptom categories.
FIGURE 1.
Logistic regression results for attention-deficit hyperactivity symptom endorsement by caregiver education level. GED, General Education Diploma; HS, high school; AA, A.A. degree; VOC, vocational; BA, B.A. degree.
Multivariate Analysis of Covariance
The mean number of IA and HA items endorsed served as the dependent measure for this analysis. The independent variable was caregiver education and covariates included youth age, youth gender, and caregiver race/ethnicity.
The number of IA but not HA symptoms endorsed differed by caregiver education [F(1, 1380) = 3.19, p < .001]. That is, caregiver education influenced endorsement of IA but not HA symptoms. Covariate effects were found for youth gender (HA: F1, 1380 = 19.97, p < .001; IA: F1, 1380 = 13.53, p < .001) and caregiver race/ethnicity (HA: F1, 1380 = 12.05, p < .001; IA: F1, 1380 = 73.64, p < .001). The number of HA but not IA symptoms endorsed differed by youth age (F1, 1380 = 59.29, p < .001).
Logistic Regressions
The same variables (caregiver education, youth age, youth gender, caregiver race/ethnicity) were then entered into 18 separate logistic regression models with endorsement (yes/no) of each of the HA and IA criteria as the dependent measure. Symptoms for which caregiver education was a significant predictor of endorsement are shown with asterisks in Figure 1. Supporting our hypothesis, caregiver education level was a significant predictor of all IA symptoms but only one HA symptom (i.e., “intrudes on others”).
Multiple Indicator Multiple Cause Model
To more comprehensively test our hypothesis, we conducted multiple indicator multiple cause (MIMIC) analysis estimated with the Mplus statistical analysis program.18 This type of modeling allows us to address concerns raised by the problem of multiple comparisons in the logistic regressions described above while controlling for important covariates. As shown in Figure 2, we developed a theoretical model based on clinical observation and consonant with our analytic strategy. Specifically, our goal was to simultaneously estimate the effect of caregiver education level on the endorsement of IA and HA latent variables while simultaneously controlling for caregiver race, youth gender, and youth age. In this model, the nine IA symptoms serve as indicators for the IA latent variable and the nine HA symptoms serve as indicators for the HA latent variable. This a priori factor structure has been supported in previous studies of attention-deficit hyperactivity disorder (ADHD) symptoms.3
FIGURE 2.
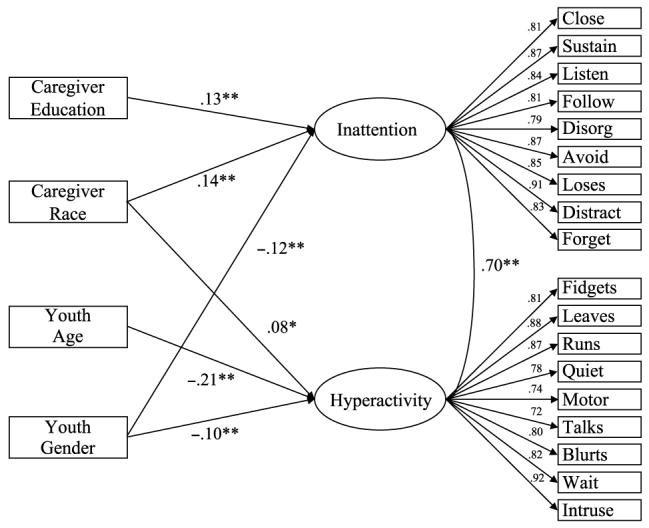
Multiple indicator multiple cause model of differential effect of caregiver education on endorsement of attention-deficit hyperactivity inattention and hyperactivity symptoms. χ2 (77, N = 1347) = 730.60, p < .001; Tucker-Lewis Index = 0.98, root mean square error of approximation = 0.08. Nonsignificant paths (i.e., p > .05) are not included in the figure. Item loadings of symptoms on inattention and hyperactivity factors are all significant at p < .01. *p < .01; **p < .001.
Because symptoms were in dichotomous form (coded as either absent or present), we estimated the model using weighted least-square parameter estimates with robust SEs and variance-adjusted χ2 test statistic. This estimation procedure allows proper estimation of models that include dichotomous, ordered categorical, and continuous variables.19 To assess model fit, we followed the recommendation of Hu and Bentler20 using a combination of fit indicators including the Tucker-Lewis Index (TLI) and the root mean square error of approximation (RMSEA). For these indicators, TLI values greater than 0.95 and RMSEA near 0.08 or less indicate good model fit. Latent variables were simultaneously regressed on caregiver years of education along with covariates of caregiver race, youth gender, and youth age.
As hypothesized, we found that caregiver years of education was significantly positively associated with IA (γ = 0.13, t = 5.40, p < .05) but not significantly associated with HA. As shown in Figure 2, the model demonstrated good fit according to the criteria of Hu and Bentler20 (χ2[77, N = 1347] = 730.61, p <.001; TLI = 0.98, RMSEA = 0.08). Item loadings on the latent variables were all high (range = 0.72 to 0.92) and significant (p < .05). With regard to covariates, youth gender was significantly associated with both IA (γ = −0.12, t = −4.58, p < .05) and HA (γ = −.10, t = 3.72, p < .05) and youth age was negatively associated with HA (γ = −0.21, t = −7.91, p < .05) but not IA. The latent variables IA and HA had a significantly positively correlated (r = .70, t = 27.11, p < .05). Caregiver race was significantly associated with both IA (γ = 0.14, t = 5.66, p < .05) and HA (γ = 0.08, t = 2.85, p < .05).
DISCUSSION
The major finding of this study is that caregivers with higher levels of education show a higher rate of endorsement of inattention (IA) symptoms relative to less educated caregivers. This relationship held across three separate sets of analyses in which other important youth and caregiver characteristics were controlled. To our knowledge, this represents the first study of its kind to explicitly test the relationship between caregiver education and differential endorsement of attention-deficit hyperactivity disorder (ADHD) symptoms.
The finding of higher rates of endorsement of IA symptoms as a function of caregiver education (a major component of socioeconomic status [SES]) in the context of no difference in the endorsement of hyperactivity (HA) symptoms is a perplexing finding. It is difficult to separate possible group differences in clinical presentation from those stemming from the effects of potentially education-sensitive symptom measures. Phenomenologically, there is little reason to expect that youths with higher educated caregivers would demonstrate higher rates of IA symptoms than youths from low-education households, as previous studies have shown higher rates of ADHD symptoms in youths from low SES backgrounds.5 While SES is not explicitly tested in the current study, the finding of higher education and higher rate of endorsement of IA symptoms is consistent with the pattern of demographic characteristics of youths described in studies of ADHD subtypes.21,22 Although SES was not a central focus of previous studies, youths diagnosed with ADHD IA subtype appear to come from higher SES backgrounds compared to youths diagnosed with the combined or hyperactive/impulsive subtypes of ADHD. The current findings raise the question as to whether the patterns observed in these studies are a function of demographic factors and the measurement of ADHD symptoms, rather than a true phenomenological finding of greater rates of inattention in youths from higher SES backgrounds. While this sample was older than those found in some other studies of ADHD, the relationship between caregiver education and HA and IA endorsement held when age was controlled in these multiple indicator multiple cause (MIMIC) analyses.
We are then left with the question of how education might mediate the endorsement of IA symptoms. We considered two broad categories of mechanisms by which caregiver educational attainment could affect the endorsement of IA symptoms, while having no effect on HA symptom endorsement: factors related to the measurement of IA and caregiver-related variables.
Measuring Inattention
Perhaps the most immediate characterization of the difference between IA and HA symptoms is that HA symptoms are more readily observable. Studies of the agreement between parent and child reports have generally found that observable behaviors or events, (e.g., bed-wetting, school suspension) elicit higher rates of concordance, while agreement is low on more abstract, less observable behavior or phenomena23,24 (e.g., poor concentration, low self-esteem). These findings suggest that less observable behaviors may be more difficult to measure accurately by virtue of being more vulnerable to respondent characteristics. Studies on interrater reliability of ratings of internalizing and externalizing symptoms have also found that parent-teacher agreement is higher for externalizing compared to internalizing behaviors/disorders.25,26 As children are generally not skilled reporters of their internal experience, internalizing symptoms may inherently require an extra step of inference and interpretation on the part of the third-party reporter, making them harder to recognize and report and thus more sensitive to reporter characteristics.
IA symptoms may also be more difficult to recognize and report because they are more context dependent than HA behaviors. Difficulty sustaining attention is most problematic at school, and it is only after school demands significantly exceed a child's cognitive resources that poor school performance alerts parents to a child's difficulty. Factor-analytic studies have also shown that HA symptoms relate to measures of global impairment, while IA symptoms are associated with academic impairment.3,27 As school requires increasingly longer periods of time in which one must attend to speakers and activities, teachers may be in the best position to detect and recognize when a child has significant trouble paying attention.
Caregiver-Related Variables
Considering that IA symptom recognition may be more difficult for all groups, we speculate that the relative difficulty may also render IA symptoms more vulnerable to the influence of demographic characteristics of respondents compared to HA symptoms. There are a number of potential caregiver-related factors that contribute to the effect of educational level on IA symptom endorsement. One possible mechanism might be through less exposure to concepts related to mental health disorders and developmental norms as a function of education. The “knowledge gap hypothesis” predicts that the rate of dissemination of information into a social environment of high SES groups will outpace the rate at which information reaches those in lower SES groups, leading to growing relative gaps in knowledge.28 The threshold at which caregivers consider behaviors or symptoms problematic or excessive depends on a caregiver's knowledge of the adaptive ranges of children's behavior. It might be argued that even general education exposes one to ways of conceptualizing behavior and possibly to mental health disorders specifically. In the absence of alternate explanations or ways to conceptualize a child's behavior, a caregiver might attribute IA symptoms to laziness or lack of effort, consistent with findings that caregivers from lower SES backgrounds may be more likely to attribute a child's actions to bad behavior.29 In terms of ADHD in particular, Bussing et al30 studied cultural differences in knowledge of ADHD in a sample of parents of children receiving special education services in a North Florida school district and found that a significantly lower percentage of parents from low SES backgrounds had ever heard of ADHD or had recently been exposed to the concept within weeks of the interview. Furthermore, self-rated knowledge of ADHD was lower in parents from low SES backgrounds compared to those from high SES backgrounds.
Caregiver education may also affect IA symptom endorsement through a caregiver's awareness of his or her own attentional fluctuations and ability to self-monitor. Success in any structured program from high school, to vocational training, to academic degrees depends on some capacity to plan, organize, evaluate one's progress, and make adjustments where necessary. These may be the same skills that underlie the ability to observe the behavior of others, including that of children, and behaviors related to ADHD specifically. Furthermore, given the heritability of ADHD symptoms31 and more continuous measures of attention,32,33 children with IA symptoms may be more likely to have parents with problems with sustained attention than children without IA symptoms. It may be that some caregivers with less education have attention difficulties of their own that they do not identify in themselves or in their children.
Another potential link between caregiver education and the endorsement of IA behaviors relates to the home contexts in which one might expect to observe attention difficulties. Many clinicians agree that symptoms of inattention are most apparent in structured activities, and in the home setting, such activities might include homework completion or reading with a child. DeGarmo and colleagues34 found that maternal education showed both direct (child academic achievement) and indirect (through skill-building activities) associations with achievement, with skill-building activities at home (reading, word games, help with homework) mediating the relationship between maternal education and a child's school achievement. The identification of IA symptoms may require caregiver engagement with a child in similar situations. However, even in this setting, IA difficulties may be hard to detect, as the one-on-one contact in this type of parent-child interaction is a scenario in which a child with ADHD usually attends best.
Clinical Implications
The results from this study have a number of possible clinical implications with regard to the assessment of ADHD. For clinicians, it is important to clarify maternal reports of IA symptoms by linking them as much as possible to objective events or behaviors. This may require a greater exploration of IA symptoms beyond the wording and exemplars used in ADHD rating scales and/or interviews. A caregiver unfamiliar with the inattentive aspect of ADHD may need more examples of the types of behaviors that indicate attention problems. These findings suggest that an informal assessment of a caregiver's understanding of IA symptoms is important in improving the accuracy of assessment and diagnosis in clinical settings.
These findings further stress the importance of the use of multiple informants of child behavior. A large body of psychometric and epidemiological literature points to the value of multiple measures in improving the psychometric features of classification systems in research and clinical practice.35 DuPaul and Stoner36 argue that teacher ratings should be given more credence and weight than parent ratings because the school is a more problematic setting for children with ADHD. Teachers have greater exposure to age-appropriate behavior and may be best qualified to report on behaviors such as difficulty following directions, inattentiveness, and ability to complete tasks.37 When a clinician finds general parent-teacher agreement on HA ratings in the context of endorsement of inattention by the teacher only, it would be important to consider that a parent may not have sufficient opportunity or ability to observe or detect a child's difficulty with inattention.
Limitations
Some limitations of the current study should be mentioned. First, we did not have a gold standard from which to consider caregiver rating accuracy. Inclusion of third-party ratings in future analyses would strengthen our conclusions. In addition, these data may reflect properties of the Diagnostic Interview Schedule for Children Version IV (DISC-IV) in assessing symptoms of ADHD, and similar analyses examining other measures or patterns of rating scale endorsements will be crucial in understanding the extent of caregiver education effects on the reporting of ADHD symptoms. These data were derived from a survey of a service using a population rather than a community sample. This population has a higher base rate of ADHD relative to community samples.12 As such, symptoms may be more readily observed, possibly highlighting differences between observers based on their ability to correctly interpret youth behaviors. Replication of this study is recommended to determine whether the observed results extend to community-based populations.
Second, post–high school education is composed of a variety of technical training programs, vocational schools, and community college programs, yet the general education requirements for entry and completion of programs is likely to vary substantially. Although an estimate of years of education may be easily attained, the degree to which years of education relates to a broad and uniform exposure to child behavior is hard to determine. It is far from clear what kind of educational background improves a parent's ability to monitor and recognize a child's capacity for sustained attention. Finally, ADHD measures should be properly normed on a wide range of populations and alternative forms of the measures could be developed for use with different populations.
CONCLUSIONS
Reliable and consistent diagnosis is a necessary condition in the effective treatment of ADHD and other disorders. Given the present findings, the impact of caregiver education level on endorsement of psychiatric symptoms should be studied further. Investigations of item analyses and other methods of symptom assessment will be needed before we have a more complete understanding of how a respondent's level of education affects the endorsement of a child's symptoms. As parent report is often the primary source of information in the psychiatric assessment of children and adolescents, an increased understanding of the complex interaction of socioeconomic, cultural, and psychiatric variables will be crucial in ensuring that effective and appropriate assessment and treatment reach youths most in need.
Acknowledgments
The Patterns of Youth Mental Health Care in Public Service Systems Study was supported by NIMH grant U01 MH55282. The preparation of this manuscript was also supported by 2P50MH50313-06. Dr. Aarons was supported by MH01695.
REFERENCES
- 1.Bauermeister JJ, Bird HR, Canino G, Rubio-Stipec M, et al. Dimensions of attention deficit hyperactivity disorder: findings from teacher and parent reports in a community sample. J Clin Child Psychol. 1995;24:264–271. [Google Scholar]
- 2.Gomez R, Harvey J, Quick C, Scharer I, Harris G. DSM-IV ADHD: confirmatory factor models, prevalence, and gender and age differences based on parent and teacher ratings of Australian primary school children. J Child Psychol Psychiatry. 1999;40:265–274. [PubMed] [Google Scholar]
- 3.Lahey BB, Applegate B, McBurnett K, et al. DSM-IV field trials for attention deficit hyperactivity disorder in children and adolescents. Am J Psychiatry. 1994;151:1673–1685. doi: 10.1176/ajp.151.11.1673. [DOI] [PubMed] [Google Scholar]
- 4.Wolraich ML, Lambert WE, Baumgaertel A, Garcia-Tornel S, Feurer ID, Bickman L. Teachers' screening for attention deficit/hyperactivity disorder: comparing multinational samples on teacher ratings of ADHD. J Abnorm Child Psychol. 2003;31:445–455. doi: 10.1023/a:1023847719796. [DOI] [PubMed] [Google Scholar]
- 5.Biederman J, Faraone SV, Keenan K, et al. Familial association between attention deficit disorder and anxiety disorders. Am J Psychiatry. 1991;148:251–256. doi: 10.1176/ajp.148.2.251. [DOI] [PubMed] [Google Scholar]
- 6.Cadoret RJ, Stewart MA. An adoption study of attention deficit/hyperactivity/aggression and their relationship to adult antisocial personality. Compr Psychiatry. 1991;32:73–82. doi: 10.1016/0010-440x(91)90072-k. [DOI] [PubMed] [Google Scholar]
- 7.Biederman J, Faraone SV, Keenan K, et al. Family-genetic and psychosocial risk factors in DSM-III attention deficit disorder. J Am Acad Child Adolesc Psychiatry. 1990;29:526–533. doi: 10.1097/00004583-199007000-00004. [DOI] [PubMed] [Google Scholar]
- 8.Bird HR, Gould MS, Yager T, Staghezza B, Canino G. Risk factors for maladjustment in Puerto Rican children. J Am Acad Child Adolesc Psychiatry. 1989;28:847–850. doi: 10.1097/00004583-198911000-00006. [DOI] [PubMed] [Google Scholar]
- 9.Barkley RA. A critique of current diagnostic criteria for attention deficit hyperactivity disorder: clinical and research implications. J Dev Behav Pediatr. 1990;11:343–352. [PubMed] [Google Scholar]
- 10.Helman CG. Culture, Health, and Illness: An Introduction for Health Professionals. Wright-PSG; Bristol, Boston, MA: 1994. [Google Scholar]
- 11.Aarons GA, Brown SA, Hough RL, Garland AF, Wood PA. Prevalence of adolescent substance use disorders across five sectors of care. J Am Acad Child Adolesc Psychiatry. 2001;40:419–426. doi: 10.1097/00004583-200104000-00010. [DOI] [PubMed] [Google Scholar]
- 12.Garland AF, Hough RL, McCabe KM, Yeh M, Wood PA, Aarons GA. Prevalence of psychiatric disorders in youths across five sectors of care. J Am Acad Child Adolesc Psychiatry. 2001;40:409–418. doi: 10.1097/00004583-200104000-00009. [DOI] [PubMed] [Google Scholar]
- 13.Shaffer D, Fisher P, Lucas CP, Dulcan MK, Schwab-Stone ME. NIMH Diagnostic Interview Schedule for Children Version IV (NIMH DISC- IV): description, differences from previous versions, and reliability of some common diagnoses. J Am Acad Child Adolesc Psychiatry. 2000;39:28–38. doi: 10.1097/00004583-200001000-00014. [DOI] [PubMed] [Google Scholar]
- 14.Jensen P, Roper M, Fisher P, et al. Test-retest reliability of the Diagnostic Interview Schedule for Children (DISC 2.1). Parent, child, and combined algorithms. Arch Gen Psychiatry. 1995;52:61–71. doi: 10.1001/archpsyc.1995.03950130061007. [DOI] [PubMed] [Google Scholar]
- 15.Schwab-Stone M, Fallon T, Briggs M, Crowther B. Reliability of diagnostic reporting for children aged 6–11 years: a test-retest study of the diagnostic interview schedule for children–revised. Am J Psychiatry. 1994;151:1048–1054. doi: 10.1176/ajp.151.7.1048. [DOI] [PubMed] [Google Scholar]
- 16.Aarons GA. Multiple indicator multiple cause (MIMIC) models in health services and clinical research; Proceedings of the 16th Annual Research Conference: A system of Care for Children's Mental Health: Expanding the Research Base; Tampa, FL. 2004. pp. 455–458. [Google Scholar]
- 17.Myers MG, Aarons GA, Tomlinson K, Stein MB. Social anxiety, negative affectivity and substance use among high school students. Psychol Addict Behav. 2003;17:277–283. doi: 10.1037/0893-164X.17.4.277. [DOI] [PubMed] [Google Scholar]
- 18.Muthén LK, Muthén BO. Mplus User's Guide. Muthén & Muthén; Los Angeles, CA: 1998. [Google Scholar]
- 19.Muthén BO. A general structural equation model with dichotomous, ordered categorical, and continuous latent variable indicators. Psychometrika. 1984;49:115–132. [Google Scholar]
- 20.Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equation Model. 1999;6:1–55. [Google Scholar]
- 21.Eiraldi RB, Power TJ, Nezu CM. Patterns of comorbidity associated with subtypes of attention-deficit hyperactivity disorder among 6- to 12-yr-old children. J Am Acad Child Adolesc Psychiatry. 1997;36:503–514. doi: 10.1097/00004583-199704000-00013. [DOI] [PubMed] [Google Scholar]
- 22.Faraone SV, Biederman J, Weber W, Russell RL. Psychiatric, neuropsychological, and psychosocial features of DSM-IV subtypes of attention-deficit/hyperactivity disorder: results from a clinically referred sample. J Am Acad Child Adolesc Psychiatry. 1998;37:185–193. doi: 10.1097/00004583-199802000-00011. [DOI] [PubMed] [Google Scholar]
- 23.Barrett ML, Berney TP, Bhate S, et al. Diagnosing childhood depression: who should be interviewed-parent or child? The Newcastle child depression project. Br J Psychiatry. 1991;159:2–27. [PubMed] [Google Scholar]
- 24.Kashani JH, Orvaschel H, Burk JP, Reid JC. Informant variance: the issue of parent-child disagreement. J Am Acad Child Adolesc Psychiatry. 1985;24:437–441. doi: 10.1016/s0002-7138(09)60561-6. [DOI] [PubMed] [Google Scholar]
- 25.Faraone SV, Biederman J, Milberger S. How reliable are maternal reports of their children's psychopathology? One year recall of psychiatric diagnoses of ADHD children. J Am Acad Child Adolesc Psychiatry. 1995;34:1001–1008. doi: 10.1097/00004583-199508000-00009. [DOI] [PubMed] [Google Scholar]
- 26.Verhulst FC, Van Der Ende J. Assessment of child psychopathology: relationships between different methods, different informants and clinical judgment of severity. Acta Psychiatr Scand. 1991;84:155–159. doi: 10.1111/j.1600-0447.1991.tb03120.x. [DOI] [PubMed] [Google Scholar]
- 27.McBurnett K, Lahey BB, Pfiffner LJ. Diagnosis of attention deficit disorders in DSM-IV: scientific basis and implications for education. Except Child. 1993;60:108–117. [Google Scholar]
- 28.Gaziano C, O'Leary J. Childbirth and infant development knowledge gaps in interpersonal settings. J Health Communication. 1998;3:29–51. doi: 10.1080/108107398127490. [DOI] [PubMed] [Google Scholar]
- 29.Jackson AP. Black, single, working mothers in poverty: preferences for employment, well-being, and perceptions of preschool-age children. Soc Work. 1993;38:26–34. [Google Scholar]
- 30.Bussing R, Schoenberg NE, Perwien AR. Knowledge and information about ADHD: evidence of cultural differences among African-American and white parents. Soc Sci Med. 1998;46:919–928. doi: 10.1016/s0277-9536(97)00219-0. [DOI] [PubMed] [Google Scholar]
- 31.Biederman J, Faraone SV, Keenan K, et al. Further evidence for family-genetic risk factors in attention deficit hyperactivity disorder: patterns of comorbidity in probands and relatives in psychiatrically and pediatrically referred samples. Arch Gen Psychiatry. 1992;49:728–738. doi: 10.1001/archpsyc.1992.01820090056010. [DOI] [PubMed] [Google Scholar]
- 32.Gjone H, Stevenson J, Sundet JM. Genetic influence on parent-reported attention-related problems in a Norwegian general population twin sample. J Am Acad Child Adolesc Psychiatry. 1996;35:588–596. doi: 10.1097/00004583-199605000-00013. [DOI] [PubMed] [Google Scholar]
- 33.Levy F, Hay DA, McStephen M, Wood C, et al. Attention-deficit hyperactivity disorder: a category or a continuum? Genetic analysis of a large-scale twin study. J Am Acad Child Adolesc Psychiatry. 1997;36:737–744. doi: 10.1097/00004583-199706000-00009. [DOI] [PubMed] [Google Scholar]
- 34.De Garmo DS, Forgatch MS, Martinez CRJ. Parenting of divorced mothers as a link between social status and boys' academic outcomes: unpacking the effects of socioeconomic status. Child Dev. 1999;70:1231–1245. doi: 10.1111/1467-8624.00089. [DOI] [PubMed] [Google Scholar]
- 35.Faraone SV, Tsuang MT. Measuring diagnostic accuracy in the absence of a “gold standard.”. Am J Psychiatry. 1994;151:650–657. doi: 10.1176/ajp.151.5.650. [DOI] [PubMed] [Google Scholar]
- 36.DuPaul GJ, Stoner G. ADHD in the Schools: Assessment and Intervention Strategies. Guilford Press; New York, NY: 1994. [Google Scholar]
- 37.Edelbrock C. Problems and issues in using rating scales to assess child personality and psychopathology. School Psychol Rev. 1983;12:293–299. [Google Scholar]