Abstract
The technique of prostate biopsy has evolved over the past 10 years to improve our ability to detect prostate cancer. Extended biopsy schemes can be performed in the office under local anesthesia and are well tolerated. In addition to detection, the role of extended biopsy schemes in refining tumor grading and risk assessment has become better defined. This review discusses the evolution of prostate biopsy techniques from the sextant scheme to the extended scheme and demonstrates the latter’s utility in clinical decision making.
Key words: Prostate biopsy, Prostate cancer
The early and accurate detection of prostate cancer is critical for the appropriate management of patients. In most cases, a prostate biopsy is the initial means of making a diagnosis. Transperineal biopsies under finger guidance were the most common means of detecting prostate cancer until transrectal biopsies under ultrasound guidance were introduced.1 A prostate nodule or symptomatic metastatic disease was the indication to perform a prostate biopsy. With the clinical introduction of prostate-specific antigen (PSA), a new indication for prostate biopsy arose, specifically, an elevated PSA in the absence of any abnormality on digital rectal examination (DRE) or symptoms.2 The need for “random sampling” of the prostate arose, and systematic biopsy was introduced.
Sextant Biopsies
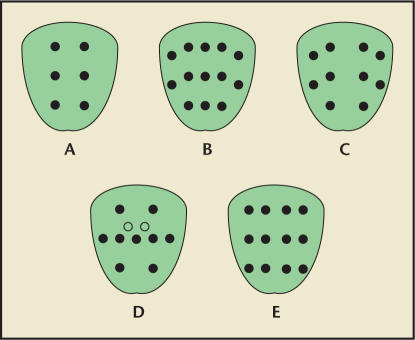
In 1989, systematic sextant biopsies under transrectal ultrasound guidance revolutionized our ability to detect prostate cancer.3 As originally described, 6 biopsies were obtained in the parasagittal plane halfway between the lateral border and midline of the prostate on both right and left sides from the base, mid-gland, and apex (Figure 1A). This systematic scheme resulted in a much higher cancer detection rate than was seen in prior prostate cancer screening studies. With respect to the derivation of the sextant template, no obvious reason other than symmetry was apparent for either the number or position of the needle core samples. Little was done regarding the refinement of this technique until, in an editorial, Stamey suggested moving the biopsies more laterally to better sample the anterior horns of the peripheral zone.4 This recommendation came from the better understanding of the zonal origin of prostate cancer offered by the meticulous pathological description from McNeal and colleagues.5 It was clear that the majority of prostate cancers (approximately 80%) originated in the peripheral zone. Thus, the entire excursion of laterally directed needles would traverse the peripheral zone, maximizing the sampling of this critical zone.
Figure 1.
Schematic diagram of biopsy schemes in coronal plane. A. Standard sextant biopsy scheme. B. 5-region biopsy scheme. C. 10-core biopsy scheme. D. 11-core biopsy scheme. Light circles represent transition zone biopsies. E. 12-core biopsy scheme.
Sampling Error in Sextant Biopsies
A systematic biopsy is a sampling of the prostate gland and, as with sampling under any circumstance, sampling error can occur. That error occurs was well demonstrated by a unique study in which 2 consecutive sets of sextant biopsies of the prostate were performed in a single office visit in 137 consecutive patients.6 A total of 43 cancers were detected in the entire study population (31% cancer detection rate). Using the first sextant biopsy set as the reference set, 30 cancers were detected (70% of all cancers). When the second biopsy set of the same prostates was used as the reference, however, 40 cancers were detected (93% of all cancers).
A second line of evidence regarding sampling error from sextant biopsies comes from the observation that in a referral-based population undergoing sextant biopsies, cancer detection rates are inversely related to prostate size.7 Cancer detection rates were 40%, 37%, 29%, 22%, 15%, and 12% for prostate sizes of 20 cc, 30 cc, 40 cc, 50 cc, 60 cc, and 70 cc, respectively. Although this phenomenon is, in part, related to selection bias (ie, men with larger prostates due to benign prostatic hyperplasia have an elevated PSA level and thus enrich a population referred for an abnormal PSA), it also may reflect sampling error (ie, 6 needle cores sample a large prostate less efficiently than a small prostate).
Evolution of the Extended Biopsy Schemes for Initial Biopsy Patients
Sextant biopsies remained the standard practice and were unquestioned until the novel study from Eskew and colleagues reported on a 5-region biopsy scheme.8 The 5 regions included the standard sextant biopsy regimen obtained halfway between the lateral border and midline of the prostate on both right and left sides (regions 2 and 4) but also obtained 2 biopsies from each lateral aspect of the prostate (regions 1 and 5) and 3 biopsies from the midline at the apex, mid-gland, and base (region 3) (Figure 1B). In their initial report on 119 patients, the overall cancer detection rate was 40%, much higher than the 20% to 25% typically seen in sextant biopsy series. The authors reported a very high complication rate of gross hematuria in over 80% of the patients. In reviewing the location of the needle placement from region 3, it was apparent that these needle cores penetrated the urethra. Before one could eliminate these needle cores from a biopsy scheme, however, it was important to note the unique contribution to cancer detection that these sites provided. In fact only 2 of the 48 cancers in this series were uniquely identified by these midline region 3 biopsies.
This work prompted an investigation on the utility of adding 4 lateral biopsies of the peripheral zone to the routine sextant biopsy regimen (10-core biopsy scheme, Figure 1C).9 Because the midline biopsies described above had a very low unique cancer detection rate and resulted in a high complication rate, they were deleted from our biopsy template. We reported on 483 patients who were undergoing an initial biopsy either for an elevated PSA level or an abnormal DRE. Using gray-scale transrectal ultrasound, we first biopsied all hypoechoic lesions and performed then a 10-core extended biopsy scheme. Our protocol also attempted to control for prostate size by taking 6 additional cores from the transition zone (16-core scheme) for any gland greater than 50 cc in size. Forty-two percent of the patients had cancer on biopsy (202/483). Routine sextant biopsies detected 161 cancers (80% of all cancers detected), and the combination of sextant and lateral biopsies, for a total of 10 peripheral zone biopsies, detected 194 cancers (96% of all cancers detected). Only 8 of 202 cancers (4%) were detected by the lesion-directed biopsies (n = 5) or the transition zone biopsies (n = 3). We concluded: 1) traditional sextant biopsies may miss over 20% of cancers; 2) a lateral sextant regimen (apex, lateral mid, lateral base) outperforms the traditional midlobar sextant regimen (89% vs 80%, respectively; P = .027); 3) regardless of the number of systematic biopsies performed (6 vs 8 vs 10), variations in cancer detection rates were most pronounced in patients with PSA levels < 10 ng/mL or in patients with prostate sizes ≥ 50 cc, reflecting the importance of sampling as patients with lower PSA levels or larger prostates more commonly may have smaller cancer volumes per unit of prostate tissue; 4) anteriorly directed biopsies rarely uniquely identify cancers in men undergoing initial biopsies with an extended peripheral zone scheme; 5) when performed in conjunction with extended peripheral-zone biopsy schemes, lesion-directed biopsies provide little unique cancer identification; and 6) when comparing the detection rates of the 5 systematic peripheralzone regions in the 10-biopsy scheme, the midlobar base region demonstrated the lowest detection rate as well as the lowest unique cancer detection rate. From the last observation we concluded that the midlobar base biopsy could be omitted from the systematic biopsy scheme. The low yield from this biopsy site may result, in part, from sampling the central zone, where the incidence of cancer is low (< 5%).
Several other investigators have reported on various extended biopsy schemes. Babaian and associates evaluated an 11-core biopsy strategy in 362 patients (Figure 1D).10 Of note, only 85 of these patients (23%) were first-time biopsy patients. The biopsy scheme included the standard sextant along with bilateral anterior-horn biopsies, bilateral transition-zone biopsies, and a midline biopsy. The detection rate for patients undergoing initial biopsy was 34% (29 of 85), and 9 cancers were uniquely identified by non-sextant sites (31% increase in cancer detection rate). Of the non-sextant, uniquely identified cancers, 7 were identified by the anterior-horn biopsies and 2 by the transition-zone biopsy.
Gore and colleagues evaluated a 12-core biopsy scheme in 396 patients.11 A standard sextant scheme was combined with a laterally directed sextant scheme at the apex, mid, and base bilaterally (Figure 1E). This series comprised 264 (67%) first-time biopsy patients, and the cancer detection rate in this subgroup was 42%. Standard sextant biopsies would have detected only 71% of the cancers in this group. The lateral sextant biopsy scheme along with the apical and base biopsies from the standard sextant scheme detected all of the cancers in this subgroup.
We felt it important to attempt to validate extended biopsy schemes in a fashion analogous to that employed in clinical trials. Too often in therapeutic trials, agents that are found to be successful in single-institution studies show lower efficacy in multicenter trials. To achieve this, we analyzed a retrospective data set of 2299 first-time biopsy patients who had undergone a 12-core systematic biopsy scheme (standard sextant and lateral sextant) by 167 communitybased urologists.12 This large series demonstrated the reproducibility of extended biopsy schemes in the hands of practicing urologists, and it should be noted that the overall cancer detection rate (44%) was essentially identical to those demonstrated by several of the above-mentioned, single-center studies. This study also enabled us to make additional observations regarding the pathologic characteristics stratified as a function of patient age or PSA. In general, increasing patient age was associated with a higher cancer detection rate, a larger number of cores involved with cancer, longer measured length of cancer on an individual core, and a higher rate of high-grade cancer (Gleason grade 4 or 5). Similar trends were observed with increasing PSA levels. With respect to the individual yield of a particular core site, the lowest yield came from the midlobar-mid and midlobar-base biopsy from the standard sextant scheme. When various biopsy schemes were retrospectively simulated and then compared with the “gold-standard” 12-biopsy scheme (assume it detects 100% of the cancers in the population) the following rates were observed: standard sextant had 78%; lateral-apex, lateralmid, lateral-base (lateral sextant) had 83%; apex, lateral-apex, lateral-mid, lateral-base (optimal 8-core scheme) had 92%; apex, mid, lateral-apex, lateral-mid, lateral-base (optimal 10-core scheme) had 96%.
The above study helped validate the 12-core extended biopsy scheme, but even with this approach there is a possibility of undersampling the apex of the prostate. The entire apex is composed of peripheral zone. As described above, biopsies performed at the apex or lateral apex may not sample the anterior apex. In 1 study in which men underwent a 12-core scheme involving the standard sextant and lateral-mid, lateral-base, and anterior apex, the anterior apex uniquely contributed to cancer detection in 6% of men with a normal DRE and prostates ≤ 50 cc in size.13
Repeat-Biopsy Patients
Urologists are often troubled by patients with a negative biopsy who continue to have a rising PSA or other indicator that raises concern for a missed cancer. There have been several attempts to refine PSA for more accurate assessment of the need for repeat biopsy, including the PSA level indexed to either total prostate volume (PSA density), transition-zone volume (transition-zone density), or the free:total PSA ratio. One large study involving 820 patients with a prior negative biopsy demonstrated that the free:total PSA ratio (area under the curve [AUC] = 0.745) and transitionzone density (AUC = 0.691) were more powerful predictors of cancer on repeat biopsy compared with PSA density (AUC = 0.618) or total PSA (0.603).14 The change of PSA over time (PSA velocity and PSA doubling time) has been suggested as possible indicators for prostate biopsy, but a recent report from the European Randomized Study of Screening for Prostate Cancer failed to show clinical utility for either PSA velocity (AUC = 0.549) or PSA doubling time (AUC = 0.573).15
A recent development in the area of prostate cancer markers has been the introduction of a urine test designed to detect messenger RNA of the prostate-cancer gene 3 (PCA3), which is highly expressed in the majority of prostate-cancer cells.16 The utility of this urinary assay was assessed recently in 233 men who had at least one prior negative biopsy. An adequate urinary sample was obtained in 97% of patients, and the PCA3 assay outperformed PSA in predicting cancer with an AUC = 0.68 compared with an AUC = 0.52 for PSA.17
No matter what parameter is used to determine the need for a repeat biopsy, it is important to first address the adequacy of the initial biopsy. Factors to consider include the location and number of cores taken as well as the size of the prostate. We have previously reported that in a repeat-biopsy population, detection rates vary as a function of the extent of the initial biopsy.18 If the prior negative biopsy was a sextant scheme, the cancer detection rate was 39% with a repeat extended biopsy, whereas if the prior negative biopsy was an extended scheme, the cancer detection rate was 28%. Because we individually labeled each core from the repeat biopsy, we could identify the unique cancer detection rate from each site. In general, apical and laterally directed biopsies resulted in the highest unique cancer detection rates. The yield from laterally directed biopsies decreased in patients who had undergone prior extended biopsy schemes, because these regions had been previously sampled by this negative biopsy. A subset of 139 patients underwent 6 additional transition-zone biopsies. The unique cancer yields in the transitionzone biopsies (cumulative for a total of 6 cores per patient) were low, regardless of type of prior biopsy scheme (3.4% for prior sextant biopsy and 5.6% for prior extended biopsy). This further confirmed the lack of utility of transition biopsies in these patients.
More aggressive biopsy approaches have been advocated in patients with prior negative biopsies. The largest “saturation biopsy” series analyzed 224 men.19 It must be noted that these biopsies are performed under anesthesia as an outpatient procedure. The mean number of cores obtained was 23 (range 14 to 45). Indications for repeat biopsy included elevated PSA in 108, abnormal DRE and elevated PSA in 27, abnormal DRE alone in 4, high-grade prostatic intraepithelial neoplasia in 64, and atypia in 21. Cancer was detected in 77 of 224 patients (34%). Complications occurred in 27 patients (12%) and included sepsis in 1, hematuria requiring hospitalization in 12, and urinary retention in 10. This study did not provide information regarding positive biopsy site identification. Thus, statements regarding the utility of such approaches seem premature.
The utility of an office-based saturation biopsy for initial biopsy has been studied by Jones and colleagues.20 In sequential cohorts, they demonstrated similar cancer detection rates in patients undergoing a 24-core saturation scheme (45%, 62 of 139) compared with a 10-core scheme (52%, 45 of 87). Thus, saturation biopsies do not appear to be necessary for initial biopsy.
Another approach similar to saturation biopsy techniques has used a transperineal template to better sample the prostate. In this series, 88 men had a mean of 15.1 cores taken, and cancer was identified in 38 (43%).21 High grade prostatic intraepithelial neoplasia or atypia was the indication for repeat biopsy in 12 (14%). All procedures were performed as outpatients using general or regional anesthesia. Although this study suggested the zone of origin for the cancers (peripheral or transition) based on the specific sector of the core on the grid, such assumptions might be flawed due to variation in prostate sizes and shapes as well as the anatomic boundaries of the peripheral and transition zones (anterior horn of peripheral zone extends anteriorly in the lateral aspect of the mid and base of the gland, whereas essentially the entire apex is composed of peripheral zone).
Needle Biopsy and Risk Stratification
Over the past several years, we have appreciated that the utility of the needle cores goes well beyond the presence or absence of cancer. These needle cores also contribute to risk assessment in patients found to have cancer. Accurate grading is important to clinical decision making. We have shown that extended biopsy schemes result in more accurate grade assessment.22 In this series we noted clinically significant upgrading in 23% of patients who had undergone an extended biopsy scheme compared to 38% in those who had undergone a sextant scheme. This observation was validated in a much larger series that showed that obtaining ≥ 8 cores was associated with a lower risk of being upgraded (odds ratio = 0.62).23 The study also showed that upgrading was associated with a higher rate of adverse pathological features as well as a higher risk of serologic relapse (relative risk = 1.86, 95% confidence interval, 1.30–2.64).
In addition to more accurate clinical grading, extended biopsy schemes have contributed to more accurate clinical staging and risk of failure. Unfortunately biopsy results have not been directly incorporated into formal staging systems such as the TNM classification for prostate cancer. Such an omission is, in my opinion, a gross oversight that one hopes will be corrected in the future. Below I will illustrate some of the more recent studies from the Shared Equal Access Regional Cancer Hospital (SEARCH) research group that have better defined the importance of needle biopsy results in predicting a pathologic endpoint such as extracapsular extension, positive surgical margins, or seminal vesicle invasion and thus might alter the decision of whether to preserve the neurovascular bundle or to undertake a wide excision on a specific side at radical prostatectomy.
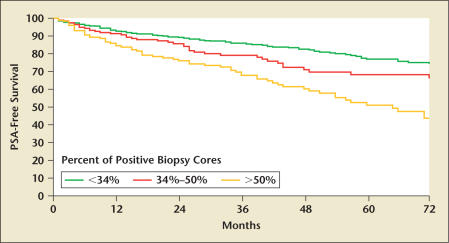
In 1 study of 1094 patients treated by radical prostatectomy, we demonstrated on multivariate analysis that the percentage of positive cores independently predicted positive surgical margins (odds ratio = 3.2), non-organ confined disease (odds ratio = 9.8), and seminal vesicle invasion (odds ratio = 22.5).24 In addition, the percentage of positive cores independently predicted risk of serologic relapse (hazard ratio = 5.0) (Figure 2). We further assessed whether the dominant force in predicting risk of relapse was the total percentage of positive cores or the percentage of positive cores from the most involved side, and we noted that it was the latter. In addition we observed that the percentage of positive cores further stratified low and intermediate risk patients using the traditional D’Amico classification but not the high-risk patients.25
Figure 2.
Kaplan-Meier estimates of biochemical recurrence rates of patients treated with radical prostatectomy stratified by the percent of cores positive on the biopsy. Pairwise P values: <34% vs 34%–50%, P = .030; < 34% vs > 50%, P < .001; 34%–50% vs > 50%, P = .006. PSA, prostate-specific antigen. Adapted from Freedland SJ et al.24
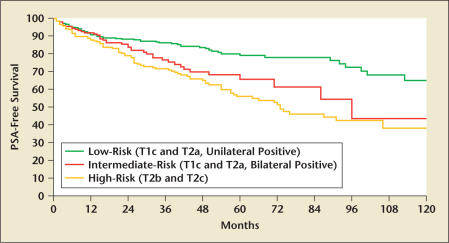
In another study we evaluated 992 patients treated by radical prostatectomy and directly determined whether biopsy laterality could improve upon either the 1992 or 1997 TNM classification system for prostate cancer.26 As currently described, the TNM system relies predominantly upon findings on DRE, which introduces significant subjectivity. We sought to determine whether knowing if the prostate biopsy was positive on 1 side or both sides contributed to assessment of risk of serologic relapse. We found that if patients had either T1c or T2a disease, they could be further substratified on the basis of whether they had unilateral or bilateral positive biopsies (Figure 3). In a multivariate analysis, this refined staging system outperformed both the 1992 and the 1997 TNM staging system.
Figure 3.
Kaplan-Meier estimates of biochemical recurrence rates of patients treated with radical prostatectomy stratified by a staging system based upon a combination of the 1992 TNM staging system and biopsy laterality (unilateral vs bilateral positive). Log rank P < .001. PSA, prostate-pecific antigen. Adapted from Freedland SJ et al.26
Conclusions
Extended prostate biopsy schemes increase cancer detection rates by more efficiently sampling the prostate. An initial biopsy should include a minimum of 12 cores with particular attention to sampling the lateral aspect of the prostate. A repeat biopsy should take additional cores from the anterior apex, or a saturation biopsy should be considered. Extended biopsies result in more accurate clinical grading and significantly contribute to risk assessment. Future revisions of the TNM classification system should include biopsy data.
Main Points.
Sextant biopsies undersample most prostates and can miss many cancers.
Extended biopsies increase cancer detection rates and decrease sampling error.
Initial biopsies should include at least 12 cores from the peripheral zone.
For repeat biopsies, consideration for anterior apical biopsies or saturation approaches is recommended.
Extended biopsies result in more accurate clinical grading and significantly contribute to risk assessment.
References
- 1.Cooner WH, Mosley BR, Rutherford CL. Clinical application of transrectal ultrasonography and prostate specific antigen in the search for prostate cancer. J Urol. 1988;139:758–761. doi: 10.1016/s0022-5347(17)42624-3. [DOI] [PubMed] [Google Scholar]
- 2.Stamey TA, Yang N, Hay AR. Prostate-specific antigen as a serum marker for adenocarcinoma of the prostate. N Engl J Med. 1987;317:909–916. doi: 10.1056/NEJM198710083171501. [DOI] [PubMed] [Google Scholar]
- 3.Hodge KK, McNeal JE, Terris MK, Stamey TA. Random systematic versus directed ultrasound guided transrectal core biopsies of the prostate. J Urol. 1989;142:71–75. doi: 10.1016/s0022-5347(17)38664-0. [DOI] [PubMed] [Google Scholar]
- 4.Stamey TA. Making the most out of six systematic sextant biopsies. Urology. 1995;45:2–12. doi: 10.1016/s0090-4295(95)96168-2. [DOI] [PubMed] [Google Scholar]
- 5.McNeal JE, Redwine EA, Freiha FS, Stamey TA. Zonal distribution of prostatic adenocarcinoma: correlation with histologic pattern and direction of spread. Am J Surg Pathol. 1988;12:897–906. doi: 10.1097/00000478-198812000-00001. [DOI] [PubMed] [Google Scholar]
- 6.Levine MA, Ittman M, Melamed J, Lepor H. Two consecutive sets of transrectal ultrasound guided sextant biopsies of the prostate for the detection of prostate cancer. J Urol. 1998;159:471–476. doi: 10.1016/s0022-5347(01)63951-x. [DOI] [PubMed] [Google Scholar]
- 7.Karakiewicz PI, Bazinet M, Aprikian AG. Outcome of sextant biopsy according to gland volume. Urology. 1997;49:55–59. doi: 10.1016/S0090-4295(96)00360-3. [DOI] [PubMed] [Google Scholar]
- 8.Eskew LA, Bare RL, McCullough DL. Systematic 5 region prostate biopsy is superior to sextant method for diagnosing carcinoma of the prostate. J Urol. 1997;157:199–203. [PubMed] [Google Scholar]
- 9.Presti JC , Jr, Chang JJ, Bhargava V, Shinohara K. The optimal systematic prostate biopsy scheme should include 8 rather than 6 biopsies: results of a prospective clinical trial. J Urol. 2000;163:163–166. [PubMed] [Google Scholar]
- 10.Babaian RJ, Toi A, Kamoi K. A comparative analysis of sextant and an extended 11-core multisite directed biopsy strategy. J Urol. 2000;163:152–157. [PubMed] [Google Scholar]
- 11.Gore JL, Shariat SF, Miles BJ. Optimal combinations of systematic sextant and laterally directed biopsies for the detection of prostate cancer. J Urol. 2001;165:1554–1559. [PubMed] [Google Scholar]
- 12.Presti JC , Jr., O’Dowd G, Miller MC. Extended peripheral zone biopsy schemes increase cancer detection rates and minimize variance in prostate specific antigen and age related cancer rates: results of a community multi-practice study. J Urol. 2003;169:125–129. doi: 10.1016/S0022-5347(05)64051-7. [DOI] [PubMed] [Google Scholar]
- 13.Meng MV, Franks JH, Presti JC , Jr, Shinohara K. The utility of apical anterior horn biopsies in prostate cancer detection. Urol Oncol. 2003;21:361–365. doi: 10.1016/s1078-1439(03)00031-0. [DOI] [PubMed] [Google Scholar]
- 14.Djavan B, Zlotta A, Remzi M. Optimal predictors of prostate cancer on repeat prostate biopsy: a prospective study of 1,051 men. J Urol. 2000;163:1144–1149. [PubMed] [Google Scholar]
- 15.Raaijmakers R, Wildhagen M, Ito K. Prostate-Specific Antigen change in the European Randomized Study of Screening for Prostate Cancer, section Rotterdam. Urology. 2004;63:316–320. doi: 10.1016/j.urology.2003.09.028. [DOI] [PubMed] [Google Scholar]
- 16.Fradet Y, Saad F, Aprikian A. uPM3, a new molecular urine test for the detection of prostate cancer. Urology. 2004;64:311–316. doi: 10.1016/j.urology.2004.03.052. [DOI] [PubMed] [Google Scholar]
- 17.Marks LS, Fradet Y, Deras IL. PCA3 molecular urine assay for prostate cancer in men undergoing repeat biopsy. Urology. 2007;69:532–535. doi: 10.1016/j.urology.2006.12.014. [DOI] [PubMed] [Google Scholar]
- 18.Hong YM, Lai FC, Chon CH. Impact of prior biopsy scheme on pathologic features of cancers detected on repeat biopsies. Urol Oncol. 2004;22:7–10. doi: 10.1016/S1078-1439(03)00147-9. [DOI] [PubMed] [Google Scholar]
- 19.Stewart CS, Leibovich BC, Weaver AL, Lieber MM. Prostate cancer diagnosis using a saturation needle biopsy technique after previous negative sextant biopsies. J Urol. 2001;166:86–92. [PubMed] [Google Scholar]
- 20.Jones JS, Patel A, Schoenfield L. Saturation technique does not improve cancer detection as an initial prostate biopsy strategy. J Urol. 2006;175:485–488. doi: 10.1016/S0022-5347(05)00211-9. [DOI] [PubMed] [Google Scholar]
- 21.Igel TC, Knight MK, Young PR. Systematic transperineal ultrasound guided template biopsy of the prostate in patients at high risk. J Urol. 2001;165:1575–1579. [PubMed] [Google Scholar]
- 22.King CR, McNeal JE, Gill HR, Presti JC., Jr Extended prostate biopsy scheme improves reliability of Gleason grading: Implications for radiotherapy patients. Int J Radiat Oncol. 2004;59:386–391. doi: 10.1016/j.ijrobp.2003.10.014. [DOI] [PubMed] [Google Scholar]
- 23.Freedland SJ, Kane CJ, Amling CL. Undergrading and overgrading of prostate needle biopsies: risk factors and clinical implications. Urology. 2007;69:495–499. doi: 10.1016/j.urology.2006.10.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Freedland SJ, Aronson WJ, Terris MK. Percent of prostate needle biopsy cores with cancer is a significant independent predictor of PSA recurrence following radical prostatectomy: results from the SEARCH Database. J Urol. 2003;169:2136–2141. doi: 10.1097/01.ju.0000065588.82511.06. [DOI] [PubMed] [Google Scholar]
- 25.D’Amico AV, Whittington R, Malkowicz SB. Biochemical outcome after radical prostatectomy, external beam radiation therapy or interstitial radiation therapy for clinically localized prostate cancer. JAMA. 1998;280:969–974. doi: 10.1001/jama.280.11.969. [DOI] [PubMed] [Google Scholar]
- 26.Freedland SJ, Presti JC , Jr., Terris MK. Improved clinical staging system combining biopsy laterality and TNM stage for men with T1c and T2 prostate cancer: results from the SEARCH database. J Urol. 2003;169:2129–2136. doi: 10.1097/01.ju.0000065763.21602.14. [DOI] [PubMed] [Google Scholar]