Short abstract
As patients want to participate more in decision making, and as the range of medical options expands, clinicians are challenged to improve their communication of risk and supportive skills. Are practitioners' counselling skills up to the job?
Different decisions require different strategies to communicate risk and support decisions, and we consider that two broad classes of decisions exist for patients. The first class lies in the area of “effective” health services, in which the benefits are large compared with harms—the participation of patients improves control of chronic conditions1 and the widespread underuse of these beneficial options.2 The second is in “preference sensitive” health services, in which the ratios of benefit to harm are either uncertain or dependent on patient values2—participation of patients improves quality of decisions and prevents overuse in the subset of informed patients who don't value the options.3
Table 1.
Differences in decision support for effective versus preference sensitive medical options
| Decision support process | Effective (benefit:harm ratio known with substantive or moderate benefit relative to harms) | Preference sensitive (benefit:harm ratio uncertain or known but close call that depends on patient's values) |
|---|---|---|
| Brief counselling | ||
| Clarify decision | Clinical problem
|
Clinical problem
|
| Recommended standard | No recommended standard, options | |
| Strength of evidence | Strength of evidence | |
| Patient's role | Patient's role | |
| Benefits and harms | Benefits, harms, scientific uncertainties | |
| Clarify values | In your opinion, is the [potential benefit] more important to you than the [chance of harm]? | Single option: In your opinion, is the [potential benefit] more important to you than the [risk/uncertainty of harm]? Multiple options: Which option has the potential benefits that are most important to you and the potential harms that are least important to you? |
| Screen for problems | Decisional uncertainty | Decisional uncertainty and related deficits in knowledge, values clarity, and support |
| Implementation: low priority or low confidence in changing |
| Referral to intensive decision support as needed | ||
|---|---|---|
| Probe stage and barriers to change | Probe stage and barriers to decision making | |
| Tailor interventions to motivations and barriers: | Tailor interventions to factors contributing to decisional uncertainty: | |
| • Information | • Information | |
| • Motivational interviewing | • Values clarification | |
| • Coaching change skills | • Coaching deliberation skills | |
| Facilitate progress in stage of change | Facilitate progress in stage of decision making | |
| Facilitate transfer of learning to future decisions | Facilitate transfer of learning to future decisions | |
| Evaluation | ||
|---|---|---|
| Process: knowledge, decisional conflict, self confidence, and progress in stage of change | Process: knowledge, realistic risk perceptions, decisional conflict, self confidence, and progress in stage of decision making | |
| Uptake and continuance of recommended option | Match between choice and patient values for benefits, harms, scientific uncertainties | |
| Underuse of effective health services | Overuse of options that informed patients don't value | |
| Health outcomes | Health outcomes may be variable due to scientific uncertainty or marginal benefit:harm ratios. Most important question for options with known benefits and harms is did patients achieve benefits preferred most and avoid harms preferred least? | |
| Decisional regret |
We investigated practical and effective approaches that doctors and practitioners can use when counselling patients about these two classes of decisions. Box 1 shows the sources we used. These approaches should help patients to understand options, benefits, harms, probabilities, and scientific uncertainties; clarify the personal value of the ratio of benefit to harm; and participate in decision making according to needs.
“Effective” versus “preference sensitive” decisions
The goal in decision making is to select health services that increase the chances of valued health outcomes and that minimise the chances of undesired consequences according to the best available scientific evidence. w3 w7
In some cases, the best strategy is clear to both practitioners and patients because the scientific evidence of benefits and harms is known and the harms are minimal relative to the benefits. Most informed clinicians would recommend the options and most informed patients would agree that the benefits outweigh the harms. Wennberg et al label services with known and favourable ratios of benefit to harm as “effective.”2 Examples include eye examinations and monitoring haemoglobin A1c and blood lipid for people with diabetes and the use of aspirin, β blockers, and angiotensin converting enzyme (ACE) inhibitors for patients with myocardial infarction.
Box 1: Sources for study
Wennberg's definition of “effective” and “preference sensitive” health services2 w1
Classification schemes for evaluating health services according to the strength of scientific evidence and the magnitude of ratios of benefit to harm4,5
Recent reviews of decision support interventions for “effective” care decisions1,6-14
Cochrane systematic review (2003 update) of trials of patient decision aids for “preference sensitive” options, including an inventory of hundreds of decision aids and 62 ongoing and published randomised controlled trials describing their efficacy3
Reviews of papers describing patient centred communication15-18 w2 and evidence based patient choice w3-w6
Personal experiences of training health professionals to develop their decision support skills in practices and call centres in Canada, the United Kingdom, the United States, and Latin America
Box 2: Schemes for classifying medical options according to strength of scientific evidence and magnitude of ratios of benefit to harm
Chalmer's scheme used in Clinical Evidence5 Beneficial—Clear evidence from randomised controlled trials; expectation of harms is small compared with benefits
Likely to be beneficial—Less well established than beneficial rating
Trade off between benefits and harms—Clinicians and patients should weigh up the beneficial and harmful effects according to individual circumstances and priorities
Unknown effectiveness—Insufficient data
Unlikely to be beneficial—Less well established than likely to be beneficial
Likely to be ineffective or harmful—Clear evidence of harmfulness of intervention
US preventive task force guidelines4
A—Strongly recommend (good quality evidence; substantial magnitude of benefit over harm)
B—Recommend in favour of routine provision (fair evidence; moderate benefit)
C—Close call, no recommendation either for or against routine provision (good or fair evidence; small magnitude of benefit or sensitive to patient values)
I—Insufficient evidence to recommend either for or against routine provision (poor quality evidence)
D—Recommend against routine provision (good or fair evidence; zero or negative magnitude of benefit over harm)
With “preference sensitive” decisions, the best strategy for an individual is unclear. Firstly, there may be inadequate evidence to draw conclusions about the ratio of benefit to harm. Secondly, the ratio may be known, but it is affected by patients' values. Wennberg et al label these decisions as preference sensitive because the best choice depends on how a person values the known risks of benefits and harms plus the scientific uncertainties.2 Examples include antenatal screening, screening for prostate cancer, management of symptoms of menopause, menorrhagia, benign prostate enlargement, back pain, or early stage breast or prostate cancers.
To guide practitioners and patients in the identification of which decisions have clearer answers and which ones are less clear, evidence based groups now classify options for care not only according to the strength of scientific evidence but also the magnitude of ratios of benefit to harm. Box 2 summarises the classification schemes of Chalmers5 and the US Preventive Task Force.4 When we analysed the Chalmers' classifications used in the 1999 issue of Clinical Evidence, 54 treatments were classified as “trade offs between benefits and harms” and 286 were classified as “uncertain”; the remainder were labelled “beneficial” and “likely beneficial.”5 These descriptions may be useful to primary care practitioners and patients in discerning which care options would be considered effective (for example, beneficial and likely beneficial) and which care options are preference sensitive (trade offs between benefits and harms; uncertain). For the specialties, Tugwell et al are the first to have incorporated these concepts in an evidence based text for specialists. w8 They not only classify and describe benefits, harms, and scientific uncertainties for several rheumatological treatments (rheumatoid arthritis, osteoarthritis, gout, tennis elbow, etc) but also include consumer summaries for both classes of decisions and patient decision aids for preference sensitive options.
Commonalities and differences in decision support
Commonalities
As a general principle, decision support should respect a patient's individual values, personal resources, and capacity for self determination. Ideally, the approach is patient centred, in which the interaction is aimed at seeing the situation through the individual patient's eyes.15-17 It includes sharing power and responsibility based on a therapeutic alliance to reach an agreement about the problem, the options, and the role in decision making.18 Patients are helped to become involved in deliberating, planning, and implementing the negotiated option.
The decision support process may involve several members of the practice team. For example, the physician may provide brief counselling by clarifying the decision and the patient's values and by screening for difficulties in decision making or implementation. For those experiencing difficulties, patients can be referred to educational materials and support from nurses, pharmacists, or other appropriate practitioners located at the practice or centres linked to the practice such as information services or nurse call centres.
Differences: “effective” options
As shown in the table, the directiveness, intensity, and focus of decision support are usually different for each class of decision. For effective decisions, counselling may be more directive because a standard of care is recommended. It may be briefer because the choice is easier to comprehend and to resolve (see fig 1 for a sample dialogue). Screening for difficulties usually uncovers implementation problems rather than decisional problems. These problems are examined by using techniques such as motivational interviewing14 to assess stage of change, priorities for change, self confidence in making changes, and other personal barriers to change. Tailored strategies are then used to address motivations, confidence, and barriers. In recent reviews of educational approaches that encourage participation of patients and reflection on internal motivation and confidence, there have been positive effects on behaviour change, control of chronic conditions, and underuse of these beneficial options in many6-13 but not all studies. w9
Fig 1.
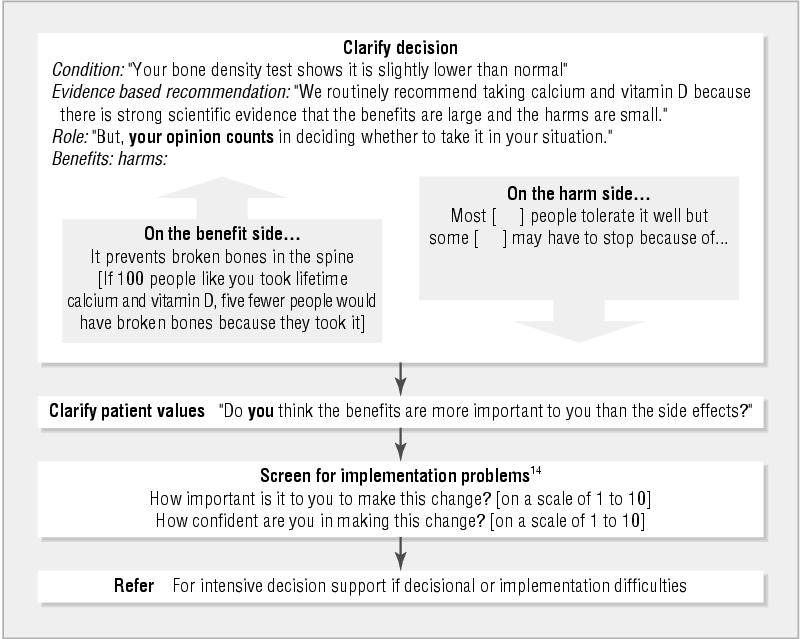
Brief decision support for “effective” options (for taking calcium and vitamin D after diagnosis of low bone density)
Differences: preference sensitive options
For preference sensitive options, counselling is non-directive. There is no right or wrong choice and a decision may or may not involve making a change in behaviour. A reasonable option may be “watchful waiting” as in the case of benign prostate conditions or menopausal symptoms. Therefore, screening for implementation problems is not always required. However, in cases where all options involve a change in status quo (for example, which colon cancer screening test to use), strategies described previously may help individuals who have identified difficulties in implementation of their chosen option.
Box 3: How decision aids affected quality of decisions3
Increased knowledge scores by 19 points out of 100 (95% confidence interval 13 to 24)
Improved the proportion of patients with realistic perceptions of the chances of benefits and harms by 40% (10% to 90%)
Lowered decisional conflict (uncertainty) related to feeling uninformed by 9 points out of 100 (6 to 12)
Reduced the proportion of patients who are passive in decision making by 30% (10% to 50%)
Reduced the proportion of people who remain undecided after counselling by 57% (30% to 70%)
Improved agreement between what a patient values and which option is chosen (three trials measured agreement in different ways)
Many patients may find it difficult to make decisions (decisional conflict).w10 The uncertainty about what to choose arises, firstly, from the inherent complexity of the choice involving trade offs between benefits and harms and scientific uncertainties and, secondly, from modifiable factors such as inadequate knowledge, unclear values, and inadequate support for decision making. These modifiable factors can be addressed with information, clarification of values, and coaching or guidance in the steps of decision making.
With preference sensitive options, the complexity of the decision often requires more detailed discussion of options, benefits, harms, probabilities, and scientific uncertainties. To streamline the process, evidence based decision aids have been developed as adjuncts to counselling. Over 400 decision aids for patients have been registered and described in an inventory developed by a Cochrane Collaboration review team3 (see also www.ohri.ca/decisionaid). Decision aids describe options and outcomes in sufficient detail for decision making. Other components may include the health condition stimulating the need for a decision; probabilities of outcomes tailored to the patient's health profile; exercises for clarification of values, which ask the patient to rate the personal importance of each benefit and harm; balanced examples of others' experiences with decision making; and guidance or coaching in the steps of decision making and communication by using strategies such as personal worksheets. The medium for delivery of decision aids varies (print, boards, videos, audio-guided workbooks), and most developers are now producing web based applications.
The Cochrane review team recently completed a systematic review of 34 randomised controlled trials conducted in Canada, the United Kingdom, and the United States; more than 30 other trials are ongoing.3 The use of decision aids as adjuncts to counselling had superior effects on the quality of decisions compared with usual practices (see box 3).3 Decision aids had comparable effects to usual care interventions on patient satisfaction, anxiety, and health outcomes that were not linked to patient values.
The impact of decision aids on the use of elective surgical procedures was remarkable and was consistent among privately versus publicly funded health systems.3 The rates of use of the most invasive surgical procedures (hysterectomy, mastectomy, prostatecomy, discectomy, coronary bypass surgery) declined by 23% (95% confidence interval 10% to 30%) in favour of more conservative surgical or medical options, without adversely affecting patients' health outcomes, satisfaction, or anxiety. Therefore, decision aids have the potential to prevent overuse of preference sensitive options in the subset of informed patients who do not value them.
Box 4: Essential strategies to improve decision quality
Improvement in access to a comprehensive library of decision aids (see website www.ohri.ca/decisionaid for a listing of decision aids); the Cochrane Collaboration review team3 is currently rating decision aids by using standard criteria known as CREDIBLE (Competent developers and development; Recent; Evidence based; Devoid of conflicts of Interest; BaLanced presentation of options, benefits, harms; Efficacious)
Development of practitioner training in decision support skills for preference sensitive decisions and in the use of decision aids
Expansion of existing information, education, and decision support service models to accommodate preference sensitive decisions (for example, on site and regional education programmes for patients, libraries for patients, and nurse call centres linked to practices)
Few studies have evaluated the effect of decision aids on patient-practitioner communication. One recent Canadian trial showed that patients who were prepared for counselling with a detailed decision aid had the same amount of counselling time with their primary care physicians as patients who were prepared with a simpler pamphlet but the quality of the time spent was different.w11-w13 For the patients given a decision aid, physicians were more likely to clarify the decision and the patients' status of decision making; there was better agreement between patients' and physicians' assessments of decisional conflict (uncertainty) and related needs regarding clarity of knowledge and values; and patients and physicians were more satisfied with the patients' preparation for decision making. Figure 2 gives a sample dialogue of decision support provided for preference sensitive options.
Fig 2.

Brief decision support for preference sensitive options (51 year old low risk woman with severe hot flushes and associated impairments in sleep and work unrelieved by conservative measures; worried about risks)
Infrastructure to support risk communication and decision support
The rates of use of “effective therapies” such as β blockers range from 5% to 92%, even in groups of “ideal candidates.”2 A key factor in explaining this large variation is lack of an infrastructure to support the use of these options. This includes education, decision support, and information systems for practitioners and patients.2,6 The Wagner model of collaborative care includes these elements to promote uptake of effective options to manage chronic conditions.6 Wagner maintains that changes are needed in the delivery of care to accomplish this goal: realignment of an organisation's incentives and priorities, re-engineering of the delivery system from reactive to proactive, and education of providers and patients to work as partners in managing chronic conditions.
Summary points
Different decisions require different strategies to communicate risk and support decisions if we are to improve the underuse of “effective” options that improve health outcomes and prevent the overuse of “preference sensitive” options that informed patients don't value
Evidence based classifications help to distinguish between effective versus preference sensitive options
For effective options, the goal is to improve uptake and health outcomes by providing brief counselling, assessing implementation difficulties, and referring to services that inform, motivate, and address barriers to change
For preference sensitive options, the goal is to improve the match between what informed patients value and what is provided by providing brief counselling, assessing decisional uncertainty, and referring to services that provide decision aids and information, clarify values, and coach in the steps of decision making
There are also wide variations in practice in the use of preference sensitive options.2 Box 4 shows three essential strategies for ensuring that variations in practice are consistent with the distribution of preferences of informed patients.
Decision support services for effective options and more recently preference sensitive options are expanding rapidly in the United States. Many of them are provided by nurse call centres that are funded by the health plans. This can pose difficulties to practitioners whose patients have diverse plans with diverse types of decision support services. The challenge is to find better ways to link decision support services to practices. A movement known as “information therapy (Ix),” headed by Donald Kemper, is working to lobby for reimbursement of providers who give “prescription strength” information tailored to need (the right information for the right patient at the right time as part of the process of care). w14
In Canada and the United Kingdom nurse call centres mainly triage to the appropriate level of professional or self care. Decision support services for chronic diseases and preference sensitive options are still in the early phases of demonstration projects. However, with single payers the potential to link decision support services to practices is more feasible. Funding for these activities is always an issue. Demonstration projects need to confirm the value of reinvesting resources saved by improving underuse of effective services and preventing overuse of preference sensitive services to build and sustain effective “just in time” systems to support decision making.
Supplementary Material
 A list of extra references (w1-w14) can be found on bmj.com
A list of extra references (w1-w14) can be found on bmj.com
Contributors: All authors drafted and revised the article. DS compiled evidence on decision aids. FL compiled evidence on patient centred care. AMO'C is the guarantor.
Competing interests: None declared.
References
- 1.Weingarten SR, Henning JM, Badamgarav E, Knight K, Hasselblad V, Gano A, et al. Interventions used in disease management programmes for patients with chronic illness—which ones work? BMJ 2002;325: 925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wennberg JE, Fisher ES, Skinner JS. Geography and the debate over Medicare reform. www.healthaffairs.org/WebExclusives/Wennberg_Web_Excl_021302.htm (accessed 17 September 2003) [DOI] [PubMed]
- 3.O'Connor AM, Stacey D, Entwistle V, Llewellyn-Thomas, H, Rovner D, Holmes-Rovner M, et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev 2003;(2): CD001431. [DOI] [PubMed]
- 4.Harris RP, Helfand M, Woolf SH, Lohr KW, Mulrow CD, Teuch SM, et al. Current methods of the US preventive services task force: a review of the process. Am J Prev Med 2001;20: 21-35. [Google Scholar]
- 5.Clinical evidence. Issue 2. London: BMJ Publishing, 1999.
- 6.Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness: the chronic care model, part 2. JAMA 2002;288: 1909-14. [DOI] [PubMed] [Google Scholar]
- 7.Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness. JAMA 2002;288: 1775-9. [DOI] [PubMed] [Google Scholar]
- 8.Bodenheimer T, Lorig K, Holman H, Grumbach K. Patient self management of chronic disease in primary care. JAMA 2002;288: 2469-75. [DOI] [PubMed] [Google Scholar]
- 9.Barlow J, Wright C, Sheasby J, Turner A, Hainsworth J. Self-management approaches for people with chronic conditions: a review. Patient Education and Counseling 2002;48: 177-87. [DOI] [PubMed] [Google Scholar]
- 10.Whitlock EP, Orleans T, Pender N, Allan J. Evaluating primary care behavioral counseling interventions: an evidence-based approach. Am J Prev Med 2002;22: 267-84. [DOI] [PubMed] [Google Scholar]
- 11.Rutter D, Quine L. Social cognition models and changing health behaviours. In: Rutter D, Quine L, ed. Changing health behaviour: intervention and research with social cognition models. Buckingham: Open University Press, 2002: 1-27.
- 12.Vermeire E, Hearnshaw H, ValRoyen P, Denekens J. Patient adherence to treatment: Three decades of research. A comprehensive review. J Clin Pharm Ther 2001;26: 331-42. [DOI] [PubMed] [Google Scholar]
- 13.Orbell S, Sheeran P. Changing health behaviours: the role of implementation intentions. In: Rutter D, Quine L, ed. Changing health behaviour: intervention and research with social cognition models. Buckingham: Open University Press, 2002: 123-37.
- 14.Emmons KM, Rollnick S. Motivational interviewing in health care settings. Am J Prev Med 2001;20: 68-74. [DOI] [PubMed] [Google Scholar]
- 15.Mead N, Bower P. Patient-centredness: a conceptual framework and review of the empirical literature. Soc Sci Med 2000;51: 1087-110. [DOI] [PubMed] [Google Scholar]
- 16.Stewart M. Towards a global definition of patient centred care. BMJ 2001;322: 444-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Weston WW, Brown JB, Stewart MA. Patient-centred interviewing. Part I: understanding patients' experiences. Can Fam Physician 1989;35: 147-51. [PMC free article] [PubMed] [Google Scholar]
- 18.Brown JB, Weston WW, Stewart MA. Patient-centred interviewing. Part II: finding common ground. Can Fam Physician 1989;35: 153-7. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


