Short abstract
Explaining risks to patients in an effective way is an essential part of ensuring that consent is “informed.” A consultant in risk communication discusses the strategies that can help doctors to communicate risks clearly, and thereby also build closer relationships with their patients
Effective risk communication is the basis for informed patient consent for medical treatment, yet until recently doctors have lagged behind other professionals in learning this skill. In other industries where risks have to be conveyed to the public (such as chemical, nuclear, water, and food industries) usually only a few people carry out this task on behalf of their organisations and they are specially trained. In contrast, in health care (where the risks are usually far higher and more uncertain and complex) almost every doctor who interacts with patients has to communicate information on risk, yet few have any training.
Specific strategies can help to remedy this deficiency and improve patients' understanding of risks. Doctors can now choose from a “toolbox” of simple, practical, time efficient techniques that benefit the widest possible variety of patients.
Methods
I have taught risk communication in risk prone professions outside medicine for over a decade.1 More recently, I have adapted my materials to respond to the needs of doctors and genetic counsellors.2 I continually review both the literature about risk communication and web based discussion groups, and this practice has informed this article.
I suggest here a set of strategies that doctors can use immediately to become more effective in helping patients to understand risks. Using visual aids also helps to foster good doctor-patient partnerships. The suggestions that follow are not a recipe of essential steps but rather a toolbox of techniques which, depending on the circumstances, can help to improve doctors' ability to communicate risk effectively.
The challenges for doctors
Communicating risk is not simple. Many different dimensions and inherent uncertainties need to be taken into account. Recent findings on the perception of risks and benefits from a psychological perspective further complicate the task. For example, Lloyd and colleagues have suggested that patients just extract the gist of any information—not the detail—to make decisions.3
Furthermore, most patients' assessment of risks is primarily determined not by facts but by emotions.4 Thus, although most doctors can readily provide a competent account of the biomedical data relating to a particular risk, this alone is likely to be sterile. If the patient's feelings skew an understanding of the facts, then his or her ability to make objective decisions about clinical management will be impaired.
For this reason, the most powerful precursor for effective risk communication is for the doctor to strive to display both competence and a caring approach.5 The doctor should therefore wish to discuss risks in a context that would enable the patient to have the best chance of understanding those risks (fig 1).6
Fig 1.

Competence and caring in relation to building trust. Adapted from Spence6
Trade-offs of risks and benefits
It is prudent to remind patients that virtually all treatments are inevitably associated with some risk of possible harm. This not only reflects the truth but also helps to counteract the tendency of some patients to expect totally risk-free medicine. It also enables the doctor to reassure the patient that all medical staff will do their best for the patient whatever treatment is chosen.
How to communicate the numbers
As well as empathising with the emotions of the patient, doctors are responsible for quoting estimates for the possible outcomes on the basis of previous cases. Often they do this by simply describing a possible treatment then telling the patient about the most likely associated risks on the basis of some unspecified population. Several simple techniques, however, can improve the way you communicate numbers.
Avoid using descriptive terms only
Avoid explaining risks in purely descriptive terms (such as “low risk”). Instead, elaborate by providing estimated numbers. Abundant evidence exists that descriptive terms reflect the speaker's perspective, with the patient often understanding the risks to be of a totally different order of magnitude.7
Use standardised vocabulary
Discuss with colleagues at a local and national level the use of a standardised vocabulary of descriptive words that consistently relate to approximate levels of probability so that miscommunication is reduced.8 The European Union's suggestions for a standardised vocabulary (“very common,” “common,” “uncommon,” “rare,” and “very rare”), however, do not communicate risk effectively: patients' interpretations of these terms do not seem to correlate with the probabilities that they were intended to convey. Different countries also probably bring different shades of meaning to various descriptions.9
Use consistent denominator
Express the odds of possible outcomes with a consistent denominator—for example, 40 out of 1000 and 5 out of 1000, rather than 1 in 25 and 1 in 200. If different denominators are used, many patients mistake which is the greater risk.10 Some may think that 1 in 200 is a bigger risk than 1 in 25, presumably because the number is larger. Using a common denominator is just as accurate and communicates just as well to people of all educational levels.
Offer positive and negative outcomes
Never present only the negative perspective (or “frame”). Ideally offer outcomes in both positive and negative forms—for example, chances of survival and of death, or chance of side effects and of remaining free of side effects. A choice expressed as offering a “97 out of 100 chance of being cured” is psychologically more acceptable than a “3 out of 100 chance of dying.” In situations where the patient's attitude is especially important in the healing process, reinforce the placebo effect by presenting the odds in a positive manner.11 However, honesty (including presenting outcomes in both positive and negative forms) is more likely to foster mature and resilient doctor-patient partnerships.
Use absolute numbers
Whenever possible, use absolute numbers—not relative risks. Patients can easily misinterpret statements such as “three times as many people were cured with approach A as with approach B.”12 These issues are described further in the accompanying paper by Gigerenzer and Edwards (pp 741-4).13
Use visual aids for probabilities
Use appropriate visual aids to help patients from all backgrounds to understand your explanations.14 Even in developed countries substantial numbers of patients have poor numeracy or literacy skills and are likely to have difficulty understanding the meaning of the numbers that doctors wish to share. For these people, visual aids can help by showing the numbers in perspective. The pie chart (pioneered by Florence Nightingale15) is a prime example of a simple yet effective visual aid, helpful to people at all academic levels.
I have developed several tools for helping to explain the risks of different orders of likelihood (figs 2, 3, 4).
Fig 2.

Paling Perspective Scale© —for giving perspective to risks of low order of probability.16 From research report by Small P et al17
Fig 3.

Paling Palette© —for displaying most medical risks with a probability of higher than 1 in 1000.16 The doctor or genetic counsellor fills in the relevant data while sitting beside the patient. This format shows the estimates of positive and negative outcomes simultaneously and presents unambiguous visual representations of the probabilities. The patient may take a printout home for further consideration, or the form may be signed by the patient and a copy kept on file
Fig 4.

Revised Paling Perspective Scale© —for displaying risks covering widely different orders of magnitude16
Ensure that consent is “informed”
For many patients, truly “informed” consent (or indeed “dissent”) is difficult to achieve without visual aids. Professionals in communications do not consider information and data to be the same. Information is considered to be data (facts) presented in a context that allows them to be meaningful to the listener. Unless probability data are expressed in some meaningful context, a case could be made that, for less educated patients, so called informed consent or dissent is often not informed at all. Good visual aids can help the viewer to see the risk numbers in context, thus providing information and not just data.
Use visual aids to build partnership
When simple visual communication tools are shared between doctor and patient, they offer an opportunity to deepen the bond between them. The closer the doctor-patient partnership, the more likely the patient is to be satisfied. Malpractice claims are also less likely; when primary care physicians with no malpractice claims against them were compared with those who had been the subject of such claims, distinct differences were found in style of communication. Statements about what to expect, enabling discussion to take place, and taking time to explore the human dimensions were all seen as teachable behaviours associated with fewer malpractice claims.18
Strategies to discuss and elicit responses
Recent meta-analyses have highlighted the fact that women doctors in general are better than men at encouraging patients to talk more freely.19 This does not mean that men are irretrievably impeded by their gender from gaining high scores in eliciting responses from patients. Indeed, in gynaecology, where there is usually a strong preference among patients for women doctors, the men were at least equal to (and often better than) the women in all aspects of their conversational style. Thus adjustments of conversational style seem to be possible with motivation and training.
Summary points
The way doctors communicate risk can affect a patient's perception of risks
Supplement verbal explanations with numerical data
Use absolute numbers; do not use relative risks or percentage improvements
State the odds from a positive and negative perspective and use a consistent denominator
Use visual aids wherever possible, to maximise understanding
Use of simple visual aids can also improve the doctor-patient relationship
Make sure the patient's informed consent is based on information—not just data
Future of risk communication in health care
Effective risk communication can improve the quality of health care in all countries and all disciplines. Three important developments are needed in this area.
Firstly, doctors need more training in communicating risk to patients.20 The motivation for this may be stimulated by the potential for improving doctor-patient partnerships (and in some countries, such as the United States, for lowering the risk of malpractice suits).
Secondly, more research is needed on how different strategies, particularly use of visual aids, help patients to understand risk. Similar studies have already assessed analogous visual tools such as the Wong-Baker FACES pain rating scale—widely used to help patients communicate their level of pain.21
Thirdly, research should assess further how differences in culture, age, and gender affect patients' perception of risks. Few studies have examined how different groups respond to risks of any kind, and no studies seem to have investigated which approaches are the most effective for communicating medical risks to different populations. Since the time of Aristotle it has been recognised that there are different “possible ways of persuading people about any subject,”22 and this is probably the case with different cultures. Given the many diverse circumstances in which medicine is practised throughout the world, it is important always to be empathetic to the individual situation of each patient. By adopting a set of simple and practical strategies, doctors should be better able to convey information on risk to their patients.
Figure 5.
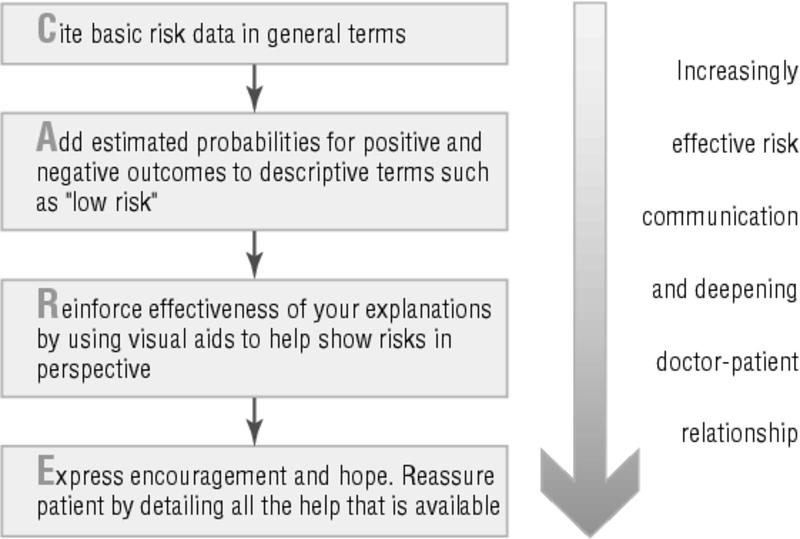
Making risk communication more effective
Supplementary Material
References
- 1.Paling J. Up to your armpits in alligators? How to sort to what risks are worth worrying about. Gainesville, FL: Risk Communication and Environmental Institute, 1997.
- 2.Stalling P. New tool for presenting risk in obstetrics and gynecology. Obstet Gynecol 2001;98: 345-9. [DOI] [PubMed] [Google Scholar]
- 3.Lloyd A, Hayes P, Bell RF, Naylor AR. The role of risk and benefit perception in informed consent for surgery. Med Decis Making 2001;21: 141-9. [DOI] [PubMed] [Google Scholar]
- 4.Ropeik D, Clay G. Risk! A practical guide for deciding what's really safe and what's really dangerous in the world around you. New York: N Y Houghton Mifflin, 2002.
- 5.Bennett P. Understanding responses to risk: some basic findings. In: Bennett P, Calman K. Risk communication and public health. Oxford: Oxford Medical Publications,1999: 3-19.
- 6.Spence J. Excellence by design: leadership. Gainesville, FL: Adbiz Publishers, 2003.
- 7.Merz JF, Druzdzel MS, Mazur DJ. Verbal expressions of probability in informed consent litigation. Med Decis Making 1991;11: 273-81. [DOI] [PubMed] [Google Scholar]
- 8.Calman KC. Cancer: science and society and the communication of risk. BMJ 1996;313: 799-802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Berry DC, Raynor DK, Knapp P, Bersellini E. Patients' understanding of risk associated with medication use: impact of European Commission guidelines and other risk scales. Drug Safety 2003;26: 1-11. [DOI] [PubMed] [Google Scholar]
- 10.Grimes DA, Snively GR. Patients' understanding of medical risks: implications for genetic counseling. Obstet Gynecol 1999;93: 910-4. [DOI] [PubMed] [Google Scholar]
- 11.McNeil BJ, Pauker SG, Sox HC, Tversky A. On the elicitation for alternative therapies. N Engl J Med 1982;306: 1259-62. [DOI] [PubMed] [Google Scholar]
- 12.Malenka DJ, Baron JA, Johanson S, Warenberger J, Ross JM. The framing effect of relative and absolute risk. J Gen Intern Med 1997;8: 543-8. [DOI] [PubMed] [Google Scholar]
- 13.Gigerenzer G, Edwards A. Simple tools for understanding risks: from innumeracy to insight. BMJ 2003;327: 741-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Edwards A, Elwyn G, Mulley A. Explaining risks: turning numerical data into meaningful pictures. BMJ 2002;324: 827-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nightingale F. Notes on matters affecting the health, efficiency, and hospital administration of the British army, founded chiefly on the experience of the late war. London: Harrison and Sons, 1858.
- 16.Paling J. Medics are from Mars and patients are from Pluto: how to help patients understand risks. Gainesville, FL: Risk Communication Institute (in press).
- 17.Small PA, Paling J. Communicating risks associated with a possible smallpox attack. http://ccl.ichp.edu/smallpox/ (accessed 10 September 2003).
- 18.Levinson W, Roter DL, Mullooly JP, Dull VT, Frankel RM. Physician-patient communication: the relationship with malpractice claims among primary care physicians and surgeons. JAMA 1997;277: 553-9. [DOI] [PubMed] [Google Scholar]
- 19.Roter DL, Hall JA, Aoki Y. Physician gender effects in medical communication. A meta-analytic review. JAMA 2002;288: 756-64. [DOI] [PubMed] [Google Scholar]
- 20.Edwards A, Mathews E, Pill R, Bloor M. Communicating about risk: diversity among primary care professionals. Fam Pract 1998;15: 296-300. [DOI] [PubMed] [Google Scholar]
- 21.Wong DL, Baker CM. Pain in children: comparison of assessment scales. Pediatr Nursing 1988;141: 9-17. [PubMed] [Google Scholar]
- 22.Aristotle. Rhetoric. (Quoted in Ross D. Aristotle. 5th ed. New York: Methuen, 1964.)
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.



 Full size PDF versions of figures
Full size PDF versions of figures