Abstract
Background
In sub-Saharan areas, malaria transmission was mainly ensured by Anopheles. gambiae s.l. and Anopheles. funestus vectors. The immune response status to Plasmodium falciparum was evaluated in children living in two villages where malaria transmission was ensured by dissimilar species of Anopheles vectors (An. funestus vs An. gambiae s.l.).
Methods
A multi-disciplinary study was performed in villages located in Northern Senegal. Two villages were selected: Mboula village where transmission is strictly ensured by An. gambiae s.l. and Gankette Balla village which is exposed to several Anopheles species but where An. funestus is the only infected vector found. In each village, a cohort of 150 children aged from one to nine years was followed during one year and IgG response directed to schizont extract was determined by ELISA.
Results
Similar results of specific IgG responses according to age and P. falciparum infection were observed in both villages. Specific IgG response increased progressively from one-year to 5-year old children and then stayed high in children from five to nine years old. The children with P. falciparum infection had higher specific antibody responses compared to negative infection children, suggesting a strong relationship between production of specific antibodies and malaria transmission, rather than protective immunity. In contrast, higher variation of antibody levels according to malaria transmission periods were found in Mboula compared to Gankette Balla. In Mboula, the peak of malaria transmission was followed by a considerable increase in antibody levels, whereas low and constant anti-malaria IgG response was observed throughout the year in Gankette Balla.
Conclusion
This study shows that the development of anti-malaria antibody response was profoundly different according to areas where malaria exposure is dependent with different Anopheles species. These results are discussed according to i) the use of immunological tool for the evaluation of malaria transmission and ii) the influence of Anopheles vectors species on the regulation of antibody responses to P. falciparum.
Background
Plasmodium falciparum malaria is a major cause of human morbidity and mortality throughout tropical Africa. In sub-Saharan areas, malaria transmission is caused by several anopheles vectors, mostly Anopheles gambiae sensu stricto (s.s.) and Anopheles arabiensis from the Anopheles. gambiae complex, Anopheles funestus and Anopheles pharaoensis [1,2]. Depending on their bio-ecology, these species tend to alternate in different situations and seasons, since An. funestus breeds prolifically in swampy habitats with much vegetation, whereas freshwater members of the An. gambiae complex do best in small sunlit pools. The anthropophilic sibling species An. arabiensis and/or An. gambiae s.s. usually predominate in areas where the environmental conditions do not provide plentiful breeding sites for An. funestus [3], or where house-spraying has eliminated An. funestus [4]. Thus, An. gambiae sensu lato (s.l.) is the principal malaria vector in many epidemiological settings of the Afro-tropical region, such as Kenya [5], Tanzania [6], Zimbabwe [7], Zaire [8], and Senegal [9]. Nevertheless, in some local ecological environment (presence of permanent swamps and emergence vegetation), An. funestus can play a predominant role in malaria transmission. In Savannah areas, An. funestus has been shown to relay An. gambiae s.l., which reaches its peak of abundance in the early dry season [10].
In the Northern part of Senegal, malaria transmission is low, unstable and seasonal with an average of two to seven infective bites/person/year [11,12]. The management of Manantali and Diama dams, that have decreased the salinity gradient along the Senegal River, has probably contributed to the reappearance of An. funestus (which disappeared as a result of the drought in the 1970s) [12]. This situation has contributed to maintain malaria transmission at the beginning of the dry season [13]. The concomitant presence of An. gambiae and An. funestus vectors in this region provided an opportunity to survey this particular situation in which high risk of intense malaria transmission in populations presenting low anti-malaria immunity is commonly seen [14].
In many epidemiological studies, malaria transmission can be estimated by evaluating the density of Anopheles vectors infected by Plasmodium associated with the degree of infection/morbidity attributed to malaria in human [15]. Serological investigations have been also used to determine malaria transmission based on the antibody (Ab) levels against antigens to P. falciparum [16]. Recent immunological studies revealed that Ab directed to a panel of sporozoites and pre-erythrocytes antigens (NANP10, TRAP, SALSA, GLURP, STARP) or crude schizont extract increased with malaria exposure [17,18]; these Ab responses, therefore, estimate the level of malaria transmission rather than an immune-dependent protection [19].
To explore the risk and dynamics of malaria transmission, a longitudinal survey using an immunological marker, was conducted in Northern Senegal. Specific antibodies to P. falciparum blood stages have been screened using antigenic materiel derived from parasite lysates crude schizont [20] as a wide panel of parasite antigens [21]. This suggests that IgG Ab levels directed to wide antigens of P. falciparum represent a sort of global "picture" of anti-malaria immunity and gives information about malaria transmission.
In the present study, the objectives were
1) To evaluate IgG responses to P. falciparum wide antigens in two sites located in Northern Senegal (Mboula and Gankette Balla villages) where different Anopheles species are responsible for malaria transmission (An. gambiae s.l. and An. funestus, respectively)
2) To analyse the relationships between specific Ab levels and parasitological and entomological data
3) To analyse the one-year dynamics of Ab responses to P. falciparum in both villages according to the period of malaria transmission
Methods
Study population
The study was conducted in the north of Senegal, in two villages, Mboula and Gankette Balla, located along the Senegal River Basin, nearby Ferlo and the Lake Guiers, respectively. In this area, the prevalence and intensity of P. falciparum are known to be low in children less than 15 years of age [11]. This site is a dry savannah, with rainy season from July to October, and represents thus a typical area of the Sahelian and sub-Sahelian regions of Africa, with approximately 400 mm of rain by year. Malaria transmission in this area is seasonal from September to December [11,13].
The study population is in majority from the Wolof ethnic group. A longitudinal study was performed during one year, between June 2004 and June 2005 in both villages. Five passages (June, September, December 2004 and March, June 2005) were undertaken and, for each passage, a cohort of 150 children aged from one to nine years was selected for each village. The later passage included the distribution of permethrin-impregnated bet nets.
For each child, parasitological measurements of malaria were performed at each passage using thick blood smears (TBS) obtained by finger-prick. The smears were Giemsa-stained to identify Plasmodium species and the number of malaria parasites was counted. Parasite density was defined as the number of P. falciparum parasites/μl of blood. In the same way, capillary blood collection was done for each child at each passage for the determination of specific IgG levels by ELISA.
The present study followed ethical principles according to the Helsinki Declaration, and was approved by the Ethical Committee of the Ministry of Health of Senegal (CNRS; June 2004). Informed consent was obtained from the studied population.
Entomological analysis
Adult mosquitoes were collected in June, September, December 2004 and March 2005 in both villages by human-landing collection. In each village, mosquito populations were caught in three selected households in six collection sites half indoor/half outdoor (7:00 p.m to 7:00 a.m) during two consecutive nights. The number of bites per human per night (BHN) was calculated by dividing the number of mosquitoes caught by the total person-night used for the period. Mosquitoes caught were brought to the laboratory, counted and identified morphologically to Anopheles species [22]. Anopheles infection rate was studied by ELISA (Enzyme-Linked ImmunoSorbent Assay) for P. falciparum circumsporozoite antigen (CSP). For all specimens, only 0.04% An. funestus collected in Gankette Balla was positive for P. falciparum CSP with an entomological inoculation rate (EIR) estimated to 3.00 infected bites. In contrast, transmission was not perceptible in Mboula whereas An. gambiae s.l. is the strict potential collected vector (EIR = 0).
Evaluation of antibody response
ELISA was used to evaluate IgG directed to total extract of schizont. Total schizont antigen is a soluble extract of P. falciparum schizont lysate obtained from infected erythrocyte and kindly provided by D. Dive from the Institut Pasteur of Lille.
Schizont extract (7.5 μg/ml) were coated on flat-bottom microtiter plates (Nunc, Roskilde, Danemark) with 100 μL/well for 2 h 30 at 37°C. Plates wells were then blocked for 30 mn at room temperature with 200 μL of blocking buffer, pH 6.6 (Phosphate-Buffered Saline, PBS), 0.5% gelatin (Merck, Darmstadt, Germany) and washed one time with PBS, pH 7.2, 0.1% Tween 20 (Sigma Chemical Co). Individuals sera were incubated in duplicate at 4°C overnight at a 1/50 dilution (in PBS-Tween-0.1%). This dilution was determined as the optimum after several preliminary experiments. For detecting human IgG, plates were incubated for 90 min at 37°C with 100 μL of mouse biotinylated mAb to human IgG (BD Pharmingen, San Diego CA, USA) diluted 1/1000 in PBS-Tween 0.1%, after three times washing with PBS-Tween 0.1%. Plate wells were then washed four times with PBS-Tween and incubated for 30 minutes at room temperature with 100 μL of peroxydase-conjugated streptavidin (Amersham Biosciences, les Ulis, France). After washing six times with PBS-Tween, colorimetric development was carried out using ABTS (2.2'-azino-bis (3-ethylbenzthiazoline 6-sulfonic acid) diammonium; Sigma, St Louis, MO, USA) in 50 mM citrate buffer (Sigma, pH = 4, containing 0.003% H2O2) and absorbance (OD) was measured at 405 nm. Individuals results were expressed as ΔDO value calculated according to the formula: ΔDO = ODx-ODn, where ODx is the individual OD value of infected individuals and ODn was the individual OD value for each serum without antigen. The reproducibility of OD-positive values from IgG responders in the study children was verified in three later assays. A negative control (pool of sera from European individuals) was used for each assay. A subject was considered an immune responder if this ODx was higher than the ODn + (3 × SD) value.
Statistical analysis
All data were analysed with Graph Pad Prism® (Graph Pad, San Diego, USA) and R software version 2.3.1. After verifying that values in each group did not assume a Gaussian distribution, differences in Ab levels were tested by Mann-Whitney U-test and Kruskal-Wallis test between more than two groups. The non-parametric Friedman-test matched pair test was used to compare paired sera all along the follow up. Spearman's correlation was used to check for correlations between parameters. All differences were considered significant when P < 0.05.
Results
Evolution of specific IgG response during one year follow-up
The percentage of anti-malaria IgG responders, the P. falciparum prevalence in children and the intensity of exposure to both major Anopheles species bites (BHN) along the year follow-up, are presented on Table 1.
Table 1.
Characteristics of studied populations during one year follow-up: P. falciparum prevalence, specific IgG immune responders and entomological data of Anopheles exposure.
| Mboula (n = 62) | Gankette Balla (n = 89) | |||||||
| P.P.f1 | Responders2 (%) | An. gambiae3 (BHN) | An. funestus3 (BHN) | P.P.f1 | Responders2 (%) | An. Gambiae3 (BHN) | An. funestus3 (BHN) | |
| June 04 | 5.5 | 49/62 (79.03) | 0.25 | 0 | 4 | 61/89 (68.54) | 0 | 9.83 |
| Sept 04 | 16.1 | 51/62 (82.26) | 3 | 0 | 7.4 | 65/89 (73.03) | 0.17 | 117 |
| Dec 04 | 21.9 | 51/62 (82.26) | 0.08 | 0 | 7 | 67/89 (75.08) | 0.50 | 96.33 |
| March 05 | 22 | 53/62 (85.48) | 0 | 0 | 5.7 | 65/89 (73.03) | 0.17 | 18.17 |
| June 05 | 10 | 50/62 (80.65) | ND | ND | 4.7 | 64/89 (71.91) | ND | ND |
1P.P.f: Prevalence of P. falciparum in children (%).
2 Number of responders in anti-schizonte IgG response (%).
3 BHN = number of mosquito bites per human per night.
ND: Not Determined
The entomological data indicated that mainly An. gambiae s.l. was collected by using the human-landing method in Mboula village (only two An. pharoensis mosquitoes collected during the one year follow-up) suggesting that children were practically exposed only to bites by An. gambiae species. The exposure to An. gambiae bites was maximum in September but stayed low (BHN = 3). Whereas no infected An. gambiae was detected, moderate prevalence of P. falciparum was observed during the seasonal transmission (16 to 22%). Indeed, prevalence increased in September to reach a peak in December and March. It could be thus considered that An. gambiae species was the strict vector in Mboula. In contrast, in Gankette Balla, individuals were largely exposed to An. funestus bites as indicated by very high BHN compared to low An. gambiae BHN. In addition, exposure to An. funestus was higher in September and December and this species is the strict vector in this village. A very low prevalence of P. falciparum was observed during the year follow-up.
In both villages, high specific IgG responders were found with prevalence ranging from 68 to 85% (Table 1). For each village, the rate of responders was relatively constant during the year follow-up. A highest prevalence of P. falciparum infection was found in Mboula which presented differences according to the passage with a peak between December and March 2005 (Table 1). Therefore, the evolution of P. falciparum prevalence did not seem to influence the % of IgG responders in both villages.
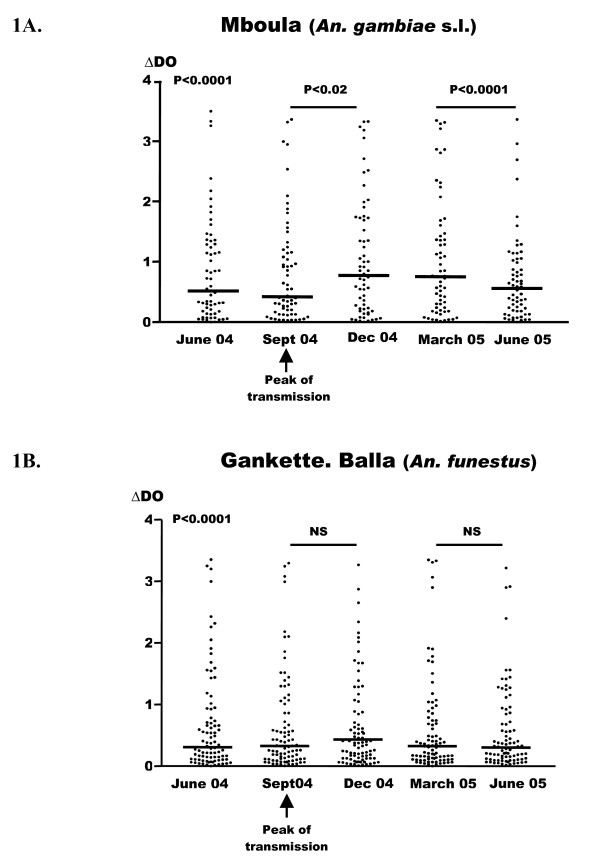
In contrast to the percentage of responders, differences in the levels of specific antibody responses were observed between both villages (Figure 1). The highest Ab levels to schizont extract were observed in Mboula all along the studied period, compared to Gankette Balla (Figure 1C). In Mboula, a significant increase of specific IgG responses was observed between September to December (Figure 1A, P < 0.02). Thereafter, these responses mildly declined from March to June 2005 (Figure 1A, P < 0.0001). This variation of the specific IgG Ab levels according to months appeared roughly concomitant with the peak of malaria transmission (September to March – Table 1). In contrast, no variation of IgG Ab levels was observed along the year follow-up in Gankette Balla (Figure 1B).
Figure 1.
Anti-P. falciparum IgG responses according to the malaria transmission periods in the two villages. Individual absorbance (ΔDO) results obtained for each passage are shown only for children presents for all passages (n = 62/passage in Mboula and 89/passage in Gankette Balla). Figure 1C showed median values of antibody levels (expressed in median values) in children from Mboula and Gankette Balla. NS = No Significant.
Specific IgG response and P. falciparum infection
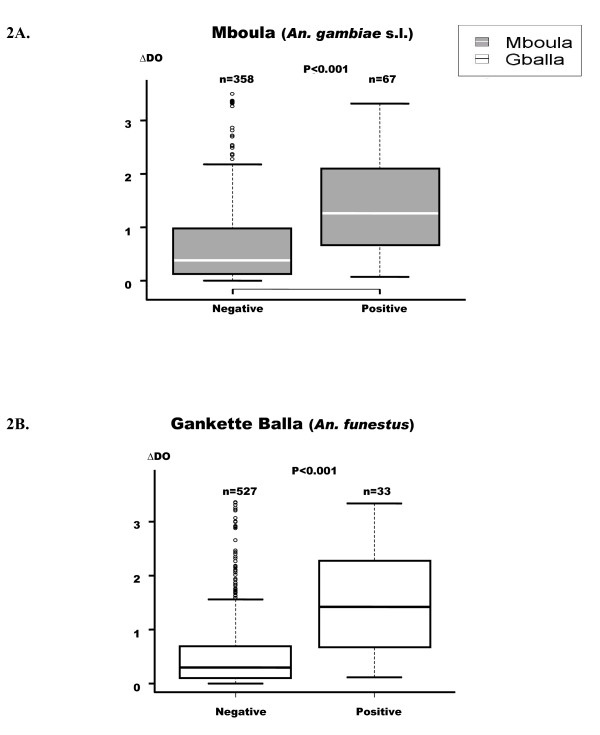
IgG Ab levels directed to schizont extract were presented according to the presence or the absence of P. falciparum infection (Figure 2). Malaria infection was diagnosed by a positive thick blood smears in children. The presented results concern the cumulative data from all passages.
Figure 2.
Anti-P. falciparum IgG responses according to malaria positive or negative infection in both villages. p value of the Mann-Whitney U-test, Box-whiskers plots illustrate medians with 25th and 75th percentiles, and whiskers for 10th and 90th percentiles. The upper whisker extends to the largest value below the 75th percentile plus the box height multiplied by 1.5. n = number of children with or without malaria positive infection.
The children presenting malaria infection developed higher IgG response than negative children (P < 0.001) (Figures 2A and 2B). Similar results of IgG levels according to P. falciparum infection were found in both villages.
In addition, a correlation was observed between the intensity of malaria infection (number of P. falciparum parasite/μl of blood) and Ab responses in Mboula (r = 0.332, P = 0.02), whereas in Gankette Balla the correlation (r = 0.047, NS) was not significant.
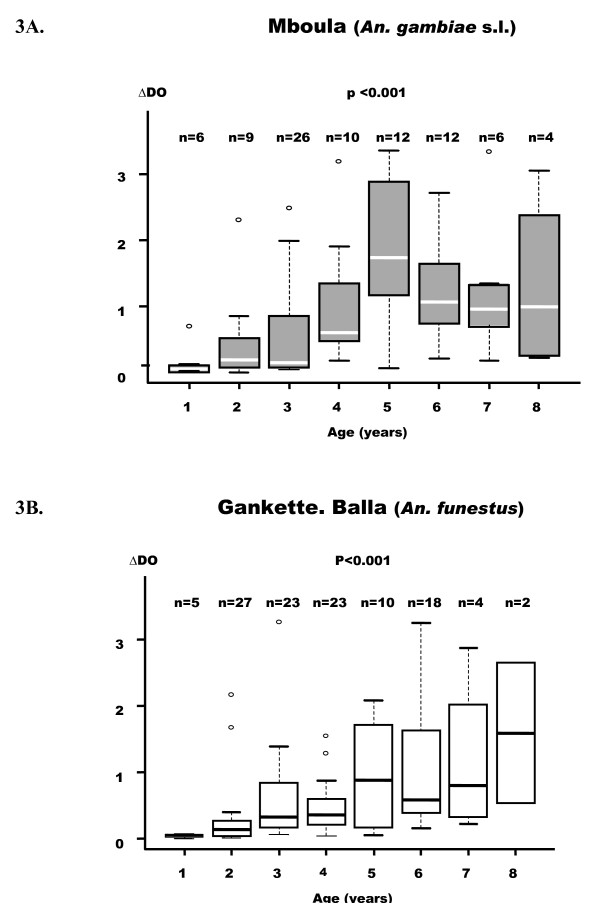
Specific IgG response and age
The levels of anti-shizont IgG after the period of transmission (December) according to the age of children was presented in Figure 3. The relationship between age and Ab levels appeared to be similar in both villages. Indeed, progressive increase of Ab levels was observed in children from one to five years of age and reached a peak at five. After this age, a slight decrease or a plateau was observed.
Figure 3.
Anti-P. falciparum IgG responses according to age in the two villages. p value of the Kruskal-Wallis U-test. Box-whiskers plots illustrate medians with 25th and 75th percentiles, and whiskers for 10th and 90th percentiles. The upper or lower whisker extends to the largest value below the 75th percentiles plus the box height multiplied by 1.5.
In Gankette Balla, specific IgG responses appeared to be correlated with age, even in children not infected by P. falciparum (r = 0.604, P = 0.004). This result suggests that the age-dependent increase of specific IgG response was not dependent to malaria status. In Mboula, this positive correlation was not significant in uninfected children (r = 0.195, P = 0.132).
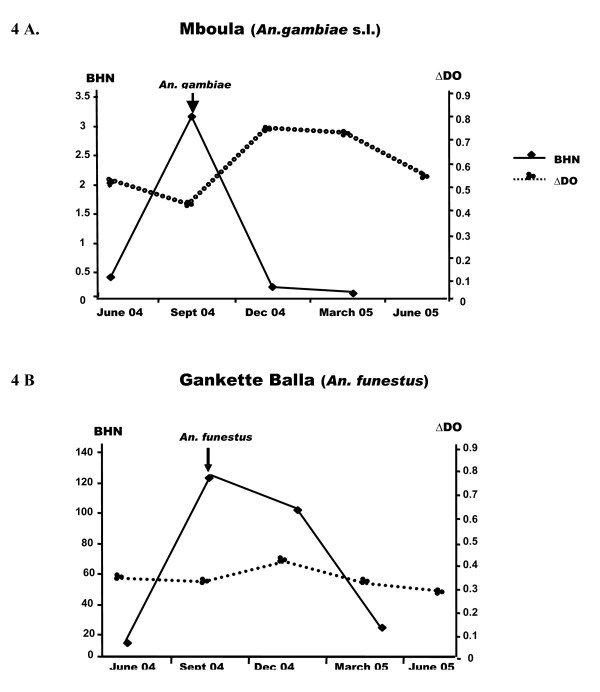
Comparison of specific IgG response with the intensity of exposure to Anopheles
The relationship between specific IgG levels (median) and entomological data evaluating the intensity of exposure to both major Anopheles species (number of aggressive mosquitoes per person per night, BHN) were presented during one year follow-up (Figure 4).
Figure 4.
Relationships between anti-P. falciparum IgG responses and the intensity of exposure to major Anopheles bites. Right and left scale delineates respectively the number of bites per human per night (BHN) and P. falciparum IgG levels (ΔDO).
In Mboula (Figure 4A), the exposure to An. gambiae increased during the period of high malaria transmission (September). This peak of An. gambiae BHN was followed by an increase in levels of specific IgG in December to March (Figure 4A). In contrast, in Gankette Balla, the peak of BHN in September was not followed by an evolution of IgG responses (Fig. 4B).
Discussion
The main point of the study was the comparison of the specific Ab response in two villages where exposure to Anopheles bites and malaria transmission were caused by two different vector species (An. gambiae s.l. vs An. funestus). For this purpose, the evolution of anti-schizont IgG levels in relation to the intensity of exposure to Anopheles species was analysed during one year. The IgG response against whole P. falciparum extract antigens was thus assessed in children living on both villages according to intensity of exposure to Anopheles species, age, period of transmission and presence of malaria infection (Table 1, Figure 3, Figure 1 and Figure 2, respectively). Specific IgG responses differed between villages and passages and remained higher in Mboula. The peak of anti-malaria IgG response appeared to follow the increase of prevalence observed in September in Mboula. In contrast, no season effect was observed in Gankette Balla. The high rate of malaria infection observed in Mboula during seasonal transmission and the very low and continuous prevalence in Gankette Balla could be one explanation of these differences observed between both villages. This positive correlation between high or low prevalence of P. falciparum infection and Ab responses levels has been reported in other epidemiological studies [23,24].
In spite of the differences of specific IgG responses between villages, positive association of immune response with P. falciparum infection was observed. This association was independent of vector species (similar in both villages) and could result from a booster effect of the presence of long-lasting presence of the parasite on the specific immunity [25,26]. The studied specific Ab responses appeared thus to be associated with malaria infection rather than anti-malarial protective immunity. The association observed between malaria infection and anti-P. falciparum IgG responses in both villages need the use of better immunological tools in order to closely evaluate the intensity of transmission. For this purpose, it has been shown that the Ab responses against different sporozoite (TRAP, CSP, NANP10) or pre-erythrocyte antigens (LSA, STARP, SALSA) are positive serological markers of malaria transmission [18,19,27]. This research is currently on the way for both studied villages in order to evaluate which adequate antigens could be used as transmission marker in children exposed to malaria, even if transmission is caused by different vector species. In addition, IgG isotypes response could be investigated as another tool to evaluate malaria transmission in a more precise manner. Indeed, Ramasamy et al [28] reported a strong relationship between cytophilic IgG1 and IgG3 Ab responses directed to sporozoite and merozoite surface antigens and malaria transmission dynamism. In addition, non-cytophilic IgG2 and IgG4 response could be, an indicator of primo-invasion [29,30].
It has been also reported that specific IgG responses increased progressively in children aged from one- to five years and then stay high until eight. This influence of age was similar in both villages and appeared to be independent to of malaria status. This intrinsic increase of anti-malaria Ab response with age was commonly reported in children living in malaria areas and in populations highly exposed to infection [31,32]. This age-dependent immune response was thought to correspond to naturally acquired immunity and to long-term memory cells of the antigenic repertoire to P. falciparum [25]. In the present study, the fact that infected children were exposed to different Anopheles species and that the prevalence of P. falciparum infection was very different between villages, did not appear to be a factor of variation of the age-dependent development of anti-malarial IgG responses.
In Mboula, the peak of An. gambiae s.l. exposure (September) was followed by the high IgG responses in December, which remained stable until March. In contrast, no difference of Ab responses was observed in Gankette Balla according to season, whereas the exposure of An. funestus vector was very high in September-December. This situation of high exposure to An. funestus species accompanied with a very low prevalence of P. falciparum infection was rarely observed in the epidemiological studies which have taken place in Senegal and elsewhere in Africa [33,34]. Several extrinsic and intrinsic epidemiological factors (genetic background of individuals, different history of malaria infection and use of anti-malaria prevention...) could be involved to explain these profound differences between the development of anti-malarial immunity in both villages exposed to two separated Anopheles vectors. Nevertheless, these immune differences could be attributed to the characteristics of malaria transmission in the areas studied. In Gankette Balla, high exposure to larval An. funestus species, resulting in the reconstitution of their breeding sites, could provide optimal conditions to aquatic stages and thus allow the emergence of adults. An. funestus collected in Gankette Balla were young, the most part having never laid and strikingly zoophilic; they seemed to present a very low vectorial capacity (Dia, unpublished). This particular situation could explain the low malaria transmission and low prevalence of P. falciparum observed in this village and could clarify the absence of seasonal variations of anti-malarial Ab response. In contrast, the low, but marked, season-dependent exposure to An. gambiae s.l. vector in Mboula appeared to induce a significant increase of specific IgG response. The bionomics of An. gambiae s.l. is closely related to human populations (anthropophilic and endophilic) and its high susceptibility to human malaria parasite endows this vector with a high vectorial ability [35]. This is why, there are significant behavioural differences between both species with a higher anthropophilic rate (75.82%) of An. gambiae s.l. in Mboula compared to An. funestus (33.18%) in Gankette Balla (Dia, unpublished).
The present study shows a close association between the presence of P. falciparum infection and the level of anti-schizont IgG response. However, it is conceivable that the bite by different Anopheles species vector which caused transmission could influence the anti-malarial Ab responses. Indeed, it is now well known that the saliva of arthropod vectors presents an immunomodulatory effect [36-38]. In addition, it has been suggested that mosquito saliva could influence parasitaemia by regulating anti-P. falciparum protective immunity [39,40]. In the present study, it has been shown that the profile of some salivary proteins and their respective immunogenicity could be different according to An. funestus and An. gambiae species (Remoue, personal communication). The identification of the different proteins between both species is actually under investigation. The variation of salivary proteins expression according to mosquito species and their secretion during the bite has been also observed between Aedes species [41]. It could thus be possible that the salivary proteins of different Anopheles species could show dissimilarity and induces a different immune regulation on the development of anti-malarial immunity. Recently, it has been demonstrated that IgG responses to Anopheles saliva is detected in children living in malaria area and represent a marker of the intensity of An. gambiae exposure [42]. The comparison of specific anti-P. falciparum and anti-saliva Ab responses in these villages according to the season is currently under investigation in the same cohort. This project will be one step to validate the hypothesis that the bite by different Anopheles vectors could influence the anti-parasite immune response.
Conclusion
The main original results of the present study show that the acquired anti-P. falciparum IgG response in children was different in two areas where malaria transmission was ensured by different Anopheles species. Previously, it has been demonstrated that in a Leishmania animal model, the immune regulation of Phlebotomus saliva can induce a substantial effect on the development of infection and pathology [43,44]. Thus, the present study suggests that the development of anti-parasite immune response could be influenced by the vector bite. The multi-disciplinary approach of the malaria transmission, bringing entomological, parasitological, epidemiological and immunological data, appeared to be necessary to validate this hypothesis.
Authors' contributions
JBS and FR have equally contributed to the design, acquisition, analysis, interpretation of data and manuscript drafting.
ID, LK contributed to conception of study and contributed markedly to the analysis of entomological data.
SG, CS, SM, ST, CT, for field activities and microscopic examinations.
AMS provided expertise and technical support for evaluation of the immune responses.
FS participated in the conception and coordination of the study and helped to draft the manuscript.
GR provided the scientific supervision in Saint Louis and revised the manuscript.
This study was performed in the framework of the "Pal-Fleuve programme" which is a structure developing multidisciplinary approaches (entomology, parasitology, immunology...) and complementary researches on malaria exposure/transmission in Northern Senegal. This programme includes four units of research: EPLS (Association Espoir Pour La Santé) – Saint Louis; IRD-UR024 (Epidémiologie et Prévention) – Dakar; UCAD (Université Cheikh Anta Diop) – Dakar and IPD (Institut Pasteur de Dakar).
Acknowledgments
Acknowledgements
The authors gratefully acknowledge the populations of Mboula and Gankette Balla villages for their participation to the study. We are grateful also the health care agents of these two villages. We wish to thank Daniel DIVE (INSERM 547, Insitut Pasteur de Lille, France) for providing the total extract of schizont antigens. We extend special thanks to Sophie Guilloneau and Sonia Fortin for their advice on data analysis.
The PAL-Fleuve programme was supported by the EPLS association, the Délégation Générale pour l'Armement (DGA-French Ministry of Defense), the French Ministry of Research (PAL+ program) and the Research Institute for Development. JB Sarr holds fellowships from the Conseil Régional de Saint-Louis, Sénégal.
Contributor Information
Jean Biram Sarr, Email: sarrjeanbirame@yahoo.fr.
Franck Remoue, Email: remoue@ird.sn.
Badara Samb, Email: badarasambe@yahoo.fr.
Ibrahima Dia, Email: dia@pasteur.sn.
Sohibou Guindo, Email: soiguindo@yahoo.fr.
Cheikh Sow, Email: sowch@ird.sn.
Sophie Maiga, Email: somaiga@hotmail.com.
Seydou Tine, Email: seydoutine@hotmail.com.
Cheikh Thiam, Email: ndombothiam@yahoo.fr.
Anne-Marie Schacht, Email: an.schacht@gmail.com.
François Simondon, Email: francois.simondon@mpl.ird.fr.
Lassana Konate, Email: konatela@yahoo.fr.
Gilles Riveau, Email: gilles.riveau@netcourrier.com.
References
- Coluzzi M. Advances in the study of Afrotropical malaria vectors. Parassitologia. 1993;35 Suppl:23–29. [PubMed] [Google Scholar]
- Trape JF, Pison G, Spiegel A, Enel C, Rogier C. Combating malaria in Africa. Trends Parasitol. 2002;18:224–230. doi: 10.1016/S1471-4922(02)02249-3. [DOI] [PubMed] [Google Scholar]
- Lindsay SW, Armstrong Schellenberg JR, Zeiler HA, Daly RJ, Salum FM, Wilkins HA. Exposure of Gambian children to Anopheles gambiae malaria vectors in an irrigated rice production area. Med Vet Entomol. 1995;9:50–58. doi: 10.1111/j.1365-2915.1995.tb00116.x. [DOI] [PubMed] [Google Scholar]
- Toure YT. The current state of studies of malaria vectors and the antivectorial campaign in west Africa. Trans R Soc Trop Med Hyg. 1989;83 Suppl:39–41. doi: 10.1016/0035-9203(89)90602-0. [DOI] [PubMed] [Google Scholar]
- Mbogo CN, Snow RW, Kabiru EW, Ouma JH, Githure JI, Marsh K, Beier JC. Low-level Plasmodium falciparum transmission and the incidence of severe malaria infections on the Kenyan coast. Am J Trop Med Hyg. 1993;49:245–253. doi: 10.4269/ajtmh.1993.49.245. [DOI] [PubMed] [Google Scholar]
- Magesa SM, Wilkes TJ, Mnzava AE, Njunwa KJ, Myamba J, Kivuyo MD, Hill N, Lines JD, Curtis CF. Trial of pyrethroid impregnated bednets in an area of Tanzania holoendemic for malaria. Part 2. Effects on the malaria vector population. Acta Trop. 1991;49:97–108. doi: 10.1016/0001-706X(91)90057-Q. [DOI] [PubMed] [Google Scholar]
- Mpofu SM. Seasonal vector density and disease incidence patterns of malaria in an area of Zimbabwe. Trans R Soc Trop Med Hyg. 1985;79:169–175. doi: 10.1016/0035-9203(85)90327-X. [DOI] [PubMed] [Google Scholar]
- Karch S, Asidi N, Manzambi ZM, Salaun JJ. [The Anopheles fauna and the transmission of human malaria in Kinshasa (Zaire)] Bull Soc Pathol Exot. 1992;85:304–309. [PubMed] [Google Scholar]
- Trape JF, Lefebvre-Zante E, Legros F, Ndiaye G, Bouganali H, Druilhe P, Salem G. Vector density gradients and the epidemiology of urban malaria in Dakar, Senegal. Am J Trop Med Hyg. 1992;47:181–189. doi: 10.4269/ajtmh.1992.47.181. [DOI] [PubMed] [Google Scholar]
- Gillies MT MBD. The anophelinae of Africa South of the Sahara: ; Johannesburg, South Africa. 2nd edn Vol. 54. 1968. [Google Scholar]
- Faye O, Gaye O, Konate L, Molez JF, Feller-Dansokho E, Herve JP. [Prediction and prevention of malaria epidemics in the valley of the Senegal River] Sante. 1998;8:347–352. [PubMed] [Google Scholar]
- Konate L, Diop A, Sy N, Faye MN, Deng Y, Izri A, Faye O, Mouchet J. Comeback of Anopheles funestus in Sahelian Senegal. Lancet. 2001;358:336. doi: 10.1016/S0140-6736(01)05517-9. [DOI] [PubMed] [Google Scholar]
- Akiana J, Camara PI, Sokhna CS, Mbaye A, Gaye O, Konate L, Le Hesran JY. [Development of seasonal malarial illness in a riparian region of Senegal] Parasite. 2003;10:283–284. [PubMed] [Google Scholar]
- Diallo TO, Nguer CM, Tall A, Diouf A, Spiegel A, Perraut R, Garraud O. [Antibodies specific to Plasmodium falciparum antigens in immune individuals: III. Seasonal course of the response to a major antigen of the asexual blood forms in two sites of different malaria exposure] Dakar Med. 1999;44:63–68. [PubMed] [Google Scholar]
- Rodhain F. [Arbovirus-vector relations] Bull Soc Pathol Exot Filiales. 1985;78:763–768. [PubMed] [Google Scholar]
- Roy A, Adak T. Evaluation of malaria endemicity by peptide ELISA. J Commun Dis. 2005;37:183–189. [PubMed] [Google Scholar]
- Kamol-Ratanakul P, Chirakalwasarn N, Lertmaharit S, Dhanamun B, Seublinwong T, Udomsangpetch R, Perlmann H, Perlmann P, Thaithong S. Seroepidemiologic studies of humoral immune response to the Plasmodium falciparum antigens in Thailand. Am J Trop Med Hyg. 1992;47:554–561. doi: 10.4269/ajtmh.1992.47.554. [DOI] [PubMed] [Google Scholar]
- Webster HK, Gingrich JB, Wongsrichanalai C, Tulyayon S, Suvarnamani A, Sookto P, Permpanich B. Circumsporozoite antibody as a serologic marker of Plasmodium falciparum transmission. Am J Trop Med Hyg. 1992;47:489–497. doi: 10.4269/ajtmh.1992.47.489. [DOI] [PubMed] [Google Scholar]
- Orlandi-Pradines E, Penhoat K, Durand C, Pons C, Bay C, Pradines B, Fusai T, Josse R, Dubrous P, Meynard JB, Durand JP, Migliani R, Boutin JP, Druilhe P, Rogier C. Antibody responses to several malaria pre-erythrocytic antigens as a marker of malaria exposure among travelers. Am J Trop Med Hyg. 2006;74:979–985. [PubMed] [Google Scholar]
- Aribot G, Rogier C, Sarthou JL, Trape JF, Balde AT, Druilhe P, Roussilhon C. Pattern of immunoglobulin isotype response to Plasmodium falciparum blood-stage antigens in individuals living in a holoendemic area of Senegal (Dielmo, west Africa) Am J Trop Med Hyg. 1996;54:449–457. doi: 10.4269/ajtmh.1996.54.449. [DOI] [PubMed] [Google Scholar]
- Perraut R, Guillotte M, Drame I, Diouf B, Molez JF, Tall A, Trape JF, Mercereau-Puijalon O, Spiegel A, Garraud O. Evaluation of anti-Plasmodium falciparum antibodies in Senegalese adults using different types of crude extracts from various strains of parasite. Microbes Infect. 2002;4:31–35. doi: 10.1016/S1286-4579(01)01506-4. [DOI] [PubMed] [Google Scholar]
- GILLIES MT BDM. The Anophelinae of Africa South of the Sahara (Ethiopian zoogeographical region) South Afr InstMed Res. 1968. p. 54:343.
- Jakobsen PH, Kurtzhals JA, Riley EM, Hviid L, Theander TG, Morris-Jones S, Jensen JB, Bayoumi RA, Ridley RG, Greenwood BM. Antibody responses to Rhoptry-Associated Protein-1 (RAP-1) of Plasmodium falciparum parasites in humans from areas of different malaria endemicity. Parasite Immunol. 1997;19:387–393. doi: 10.1046/j.1365-3024.1997.d01-234.x. [DOI] [PubMed] [Google Scholar]
- Omosun YO, Anumudu CI, Adoro S, Odaibo AB, Sodeinde O, Holder AA, Nwagwu M, Nwuba RI. Variation in the relationship between anti-MSP-1(19) antibody response and age in children infected with Plasmodium falciparum during the dry and rainy seasons. Acta Trop. 2005;95:233–247. doi: 10.1016/j.actatropica.2005.06.019. [DOI] [PubMed] [Google Scholar]
- Baird JK. Age-dependent characteristics of protection v. susceptibility to Plasmodium falciparum. Ann Trop Med Parasitol. 1998;92:367–390. doi: 10.1080/00034989859366. [DOI] [PubMed] [Google Scholar]
- Tongren JE, Drakeley CJ, McDonald SL, Reyburn HG, Manjurano A, Nkya WM, Lemnge MM, Gowda CD, Todd JE, Corran PH, Riley EM. Target antigen, age, and duration of antigen exposure independently regulate immunoglobulin G subclass switching in malaria. Infect Immun. 2006;74:257–264. doi: 10.1128/IAI.74.1.257-264.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Titanji VP, Tamu VD, Nkuo Akenji TK, Joutchop AS. Immunoglobulin G and subclass responses to Plasmodium falciparum antigens: a study in highly exposed Cameroonians. Clin Chem Lab Med. 2002;40:937–940. doi: 10.1515/CCLM.2002.164. [DOI] [PubMed] [Google Scholar]
- Ramasamy R, Nagendran K, Ramasamy MS. Antibodies to epitopes on merozoite and sporozoite surface antigens as serologic markers of malaria transmission: studies at a site in the dry zone of Sri Lanka. Am J Trop Med Hyg. 1994;50:537–547. doi: 10.4269/ajtmh.1994.50.537. [DOI] [PubMed] [Google Scholar]
- Aucan C, Traore Y, Tall F, Nacro B, Traore-Leroux T, Fumoux F, Rihet P. High immunoglobulin G2 (IgG2) and low IgG4 levels are associated with human resistance to Plasmodium falciparum malaria. Infect Immun. 2000;68:1252–1258. doi: 10.1128/IAI.68.3.1252-1258.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wahlgren M, Berzins K, Perlmann P, Persson M. Characterization of the humoral immune response in Plasmodium falciparum malaria. II. IgG subclass levels of anti-P. falciparum antibodies in different sera. Clin Exp Immunol. 1983;54:135–142. [PMC free article] [PubMed] [Google Scholar]
- Boutlis CS, Gowda DC, Naik RS, Maguire GP, Mgone CS, Bockarie MJ, Lagog M, Ibam E, Lorry K, Anstey NM. Antibodies to Plasmodium falciparum glycosylphosphatidylinositols: inverse association with tolerance of parasitemia in Papua New Guinean children and adults. Infect Immun. 2002;70:5052–5057. doi: 10.1128/IAI.70.9.5052-5057.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naik RS, Branch OH, Woods AS, Vijaykumar M, Perkins DJ, Nahlen BL, Lal AA, Cotter RJ, Costello CE, Ockenhouse CF, Davidson EA, Gowda DC. Glycosylphosphatidylinositol anchors of Plasmodium falciparum: molecular characterization and naturally elicited antibody response that may provide immunity to malaria pathogenesis. J Exp Med. 2000;192:1563–1576. doi: 10.1084/jem.192.11.1563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coetzee M, Fontenille D. Advances in the study of Anopheles funestus, a major vector of malaria in Africa. Insect Biochem Mol Biol. 2004;34:599–605. doi: 10.1016/j.ibmb.2004.03.012. [DOI] [PubMed] [Google Scholar]
- Dia I, Diop T, Rakotoarivony I, Kengne P, Fontenille D. Bionomics of Anopheles gambiae Giles, An. arabiensis Patton, An. funestus Giles and An. nili (Theobald) (Diptera: Culicidae) and transmission of Plasmodium falciparum in a Sudano-Guinean zone (Ngari, Senegal) J Med Entomol. 2003;40:279–283. doi: 10.1603/0022-2585-40.3.279. [DOI] [PubMed] [Google Scholar]
- Fontenille D, Lochouarn L, Diagne N, Sokhna C, Lemasson JJ, Diatta M, Konate L, Faye F, Rogier C, Trape JF. High annual and seasonal variations in malaria transmission by anophelines and vector species composition in Dielmo, a holoendemic area in Senegal. Am J Trop Med Hyg. 1997;56:247–253. doi: 10.4269/ajtmh.1997.56.247. [DOI] [PubMed] [Google Scholar]
- Billingsley PF, Baird J, Mitchell JA, Drakeley C. Immune interactions between mosquitoes and their hosts. Parasite Immunol. 2006;28:143–153. doi: 10.1111/j.1365-3024.2006.00805.x. [DOI] [PubMed] [Google Scholar]
- Gillespie RD, Mbow ML, Titus RG. The immunomodulatory factors of bloodfeeding arthropod saliva. Parasite Immunol. 2000;22:319–331. doi: 10.1046/j.1365-3024.2000.00309.x. [DOI] [PubMed] [Google Scholar]
- Remoue F CS., NGom A, Boulanger D, Simondon F Immune responses to arthropod bites during vector-borne diseases. Tropical Immunology. 2005. pp. 377–400.
- Boete C, Paul RE. Can mosquitoes help to unravel the community structure of Plasmodium species? Trends Parasitol. 2006;22:21–25. doi: 10.1016/j.pt.2005.11.007. [DOI] [PubMed] [Google Scholar]
- Paul RE, Diallo M, Brey PT. Mosquitoes and transmission of malaria parasites - not just vectors. Malar J. 2004;3:39. doi: 10.1186/1475-2875-3-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peng Z, Li H, Simons FE. Immunoblot analysis of salivary allergens in 10 mosquito species with worldwide distribution and the human IgE responses to these allergens. J Allergy Clin Immunol. 1998;101:498–505. doi: 10.1016/S0091-6749(98)70357-4. [DOI] [PubMed] [Google Scholar]
- Remoue F, Cisse B, Ba F, Sokhna C, Herve JP, Boulanger D, Simondon F. Evaluation of the antibody response to Anopheles salivary antigens as a potential marker of risk of malaria. Trans R Soc Trop Med Hyg. 2006;100:363–370. doi: 10.1016/j.trstmh.2005.06.032. [DOI] [PubMed] [Google Scholar]
- Belkaid Y, Kamhawi S, Modi G, Valenzuela J, Noben-Trauth N, Rowton E, Ribeiro J, Sacks DL. Development of a natural model of cutaneous leishmaniasis: powerful effects of vector saliva and saliva preexposure on the long-term outcome of Leishmania major infection in the mouse ear dermis. J Exp Med. 1998;188:1941–1953. doi: 10.1084/jem.188.10.1941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kamhawi S. The biological and immunomodulatory properties of sand fly saliva and its role in the establishment of Leishmania infections. Microbes Infect. 2000;2:1765–1773. doi: 10.1016/S1286-4579(00)01331-9. [DOI] [PubMed] [Google Scholar]