Abstract
Epidemiologic studies have implicated periodontitis as a risk factor for the development of cardiovascular disease. However, no prospective studies investigating this potential relationship have been carried out. Age- and sex-matched New Zealand White rabbits were maintained on a diet consisting of 0.5% fat for 13 weeks to induce the accumulation of lipid deposits in the aorta as a model for atherogenesis. One-half of the animals received silk ligatures around their mandibular premolars followed by an application of a periodontal pathogen, Porphyromonas gingivalis, to induce periodontitis. Animals were sacrificed after 14 weeks. Periodontal disease severity was quantified radiographically, histologically, and by direct visualization of bone loss on defleshed skulls. Lipid deposition was evaluated by computer-assisted morphometry in the aortas en face after lipid deposits were stained with Sudan IV. Animals with experimentally induced periodontitis had more extensive accumulations of lipids in the aorta than did nonperiodontitis animals (P < 0.05), and there was a positive correlation between the severity of periodontal disease and the extent of lipid deposition (r2 = 0.9501). The results provide direct evidence that periodontitis may be a risk factor and may contribute to the pathogenesis of atherosclerosis. The data support the concept that infections at remote locations can modulate atherosclerotic events distantly.
Atherosclerosis is a progressive disease process that involves large- to medium-sized muscular and large elastic arteries. Complications associated with atherosclerosis, including coronary thrombosis and myocardial infarction, contribute to over 50% of the deaths related to this disease in the United States (13). There is general agreement implicating a role for innate immune activation and inflammation in the pathogenesis of atherosclerosis, thrombosis, and neointimal thickening after arterial injury (18). While a role for inflammation is generally accepted, the initiating factors leading to the inflammatory injury remain speculative. Recent evidence has led to hypotheses implicating the involvement of one or more infectious agents in the initiation of atherosclerosis, either through direct damage to the vessel wall or through nonspecific activation of innate immune pathways (7, 18, 19). A variety of pathogens, including Chlamydia pneumoniae, Helicobacter pylori, Cytomegalovirus, Herpes simplex virus, Streptococcus sanguinis, and Porphyromonas gingivalis, have been associated with the pathogenesis of atherosclerosis and have been detected in human atheromas (4, 6).
Adult periodontitis is a chronic inflammatory disease resulting from infections by specific microbial species that colonize the oral cavity. The pathogens are mainly gram-negative anaerobic species and include P. gingivalis, Bacteroides forsythus, and Treponema denticola. While these organisms clearly initiate disease, the pathogenesis of periodontitis is thought to be mediated for the most part by host-mediated tissue injury resulting from inflammation. As a result of periodontal infection and inflammation, there is a loss of epithelial integrity within the periodontal pocket, which results in bacteremia following manipulation of the oral tissues. In a patient with periodontitis, even daily routine procedures like tooth brushing and chewing have been shown to induce a transient bacteremia (20). Thus, periodontitis is a chronic infection which can result in repeated systemic exposure to gram-negative bacteria and bacterial products.
Recent epidemiologic studies have implicated periodontitis as a risk factor for atheromatous changes in blood vessels and subsequent vascular events (1). There are two prevailing hypotheses for the relationship between periodontitis and cardiovascular disease. First, periodontal bacteria may have a direct effect on the vasculature. P. gingivalis is a common periodontal pathogen that has an interesting set of virulence factors, including hemagglutination, trypsin-like proteases (gingipains), and the ability to invade epithelial and endothelial cells (5). It has been proposed that P. gingivalis invasion is an initiating event in the pathogenesis of atheromas, and P. gingivalis DNA has been detected in carotid atheromas (6). An alternative hypothesis is that local inflammation causes an enhanced inflammatory response at distant sites without the spread of the infectious agent. In one study, P. gingivalis injected into a murine air pouch induced COX-2 mRNA expression in the heart and lungs 3 h later (16). These data suggest that a local or focal infection with this pathogen may have a systemic impact on the status of the innate immune system. In a recent paper (11), Li and coworkers demonstrated with an apoE knockout mouse model that bacteremia caused by intravenous injections of P. gingivalis resulted in increased lipid deposition in major vessels. In our present study, we sought to evaluate the effect of periodontitis on the cardiovascular outcome of a high-fat diet in a rabbit model to test the hypothesis that periodontitis will enhance lipid deposition in major vessels.
MATERIALS AND METHODS
Animal model.
A total of 12 male New Zealand White rabbits (Milbrook Breeding Laboratories) matched for age and weight were used. The IACUC committee of Brigham and Women's Hospital approved the animal protocol. The animals were individually housed with regular day and night light exposure (a cycle of 10 h of light and 14 h of darkness). All animals received water ad libitum and were fed a high-fat diet (0.5% [wt/wt] cholesterol) (Harlan Teklad). The animals were divided randomly into two groups of six animals each and were anesthetized (40 mg of ketamine/kg of body weight and 9 mg of xylazine/kg of body weight). Animals in the test group (i.e., periodontal group) had a 3-0 silk suture placed around the second premolar of both mandibular quadrants. P. gingivalis (strain A7436) was grown as previously described (10, 22). Briefly, cells were cultured on agar plates containing Trypticase soy agar supplemented with 0.5% (wt/vol) yeast extract, 5% defibrinated sheep red blood cells, 5 μg of hemin per ml, and 1 μg of vitamin K per ml. Plates were incubated for 3 days at 37°C in jars that were anaerobically maintained through palladium-catalyzed hydrogen-carbon dioxide envelopes (GasPak Plus; Becton Dickinson Microbiology Systems, Sparks, Md.). Colonies were randomly selected and anaerobically subcultured overnight at 37°C in Schaedler's broth supplemented with vitamin K and hemin. Cell numbers were spectrophotometrically determined at 600 nm (11), and 109 CFU (0.8 optical density) was mixed with carboxymethycellulose to form a thick slurry which was applied topically to the ligated teeth. The control group received carboxymethylcellulose slurry without P. gingivalis. For the first 7 weeks of the experiment, 109 CFU of the P. gingivalis slurry was applied topically around the suture on Monday, Wednesday, and Friday, with the rabbits under anesthesia (isofluorane). At these times, the sutures were also checked, and lost or loose sutures were replaced. The control animals were anesthetized using the same protocol and were given the carboxymethylcellulose slurry only, without P. gingivalis. Weekly measurements of body weight and standard hematological parameters, including clinical chemistry (complete blood count and total cholesterol levels), were recorded for all animals.
Specimen collection.
After 14 weeks, the rabbits were euthanized by pentobarbital overdose and the aortas were removed for en face quantification. The mandibles were removed for periodontal lesion quantification.
Aorta and atherosclerotic lesion quantitation.
After euthanasia, the entire aorta from each rabbit was perfused for 20 min with ice-cold phosphate-buffered saline, pH 7.4, containing 20 μM butylated hydroxy toluene (Sigma) and 2 μM EDTA by using a cannula inserted in the left ventricle. The aorta was then pressure fixed for 20 min with cold formaldehyde-sucrose solution (10% neutral formalin, 5% sucrose, 20 μM butylated hydroxy toluene, and 2 μM EDTA [pH 7.4]). The entire aorta was dissected free, adventitial fat was removed, and the aorta was opened longitudinally. The aorta was briefly rinsed in 70% ethanol followed by staining (with 0.5% Sudan IV-35% ethanol-50% acetone) for 6 min. Destaining was performed with 80% ethanol for 5 min (9). Each aorta was then mounted on a flat surface, and digital images of the aorta surface were obtained (Olympus digital camera). Images were stored in PICT format on a compact disc, and analyses were performed as previously described (11). The area covered by the lipid plaque was expressed as a percentage of the total surface area of the aorta. This area was expressed as pixels rather than millimeters to adjust for any variations in the captured image.
Periodontal lesion characterization.
After euthanasia, the mandible of each rabbit was dissected free of muscles and soft tissue; the attached gingiva was kept intact with the alveolar bone. The mandible was split into two halves from the midline between the central incisors. The left half was taken for morphometric analysis of the bone loss, and the right half was used for histological evaluation of periodontitis.
Macroscopic analysis of bone levels.
The left half of the mandible was defleshed by immersion in 10% hydrogen peroxide for 10 min. The soft tissue was carefully removed, and the mandible was stained with methylene blue for visual distinction between the teeth and bone. The bone level around the second premolar was measured directly with a calibrated (0.5 mm) periodontal probe. Measurements were made from the top of the tooth to the bone crest at three points each, at the buccal and lingual sides. A mean crestal bone level around the tooth was calculated. Similarly, for the proximal bone level, measurements were made at the mesial and distal aspects of the tooth. The measurements were taken from the buccal and lingual sides on the proximal aspects of the second premolar, and the mean proximal bone level was calculated. Bone level was also quantified by image analysis (Image Pro 4). The sectioned mandible was mounted and photographed using an inverted microscope at a magnification of ×10. The captured image was analyzed as described above, and the mean crestal bone level around the tooth was calculated in millimeters.
Radiographic analysis.
The percentage of the tooth in bone was calculated radiographically using a modification of the Bjorn technique (3). The radiographs were taken by digital X ray (Schick Technologies). To quantify bone loss, the length of the tooth from the cusp tip to the apex of the root was measured, as was the length of the tooth structure outside the bone, from the cusp tip to the coronal extent of the proximal bone. From this, the length of tooth within the bone was measured. Bone values are expressed as the percentage of the tooth in bone obtained through the following relationship: [(length of tooth in bone)/(total length of tooth)] × 100.
Histological analysis.
Bone and teeth of the other mandible halves were decalcified, processed, and embedded in paraffin. Thin sections (thickness, 7 μm) were cut and stained conventionally with hematoxylin and eosin to identify the cellular composition of the inflammatory infiltrate.
P. gingivalis 16S rRNA amplification by PCR.
Formalin-fixed aortic samples (approximately 90 mg each) were cut from the proximal, thoracic, and abdominal portions, frozen in liquid nitrogen, and then ground. The residual fixative was removed by three 10-ml changes of 50 mM Tris-HCl (pH 8.0) for 1 h each (23). DNA was isolated through phenol-chloroform extraction and ethanol precipitation and used as a template for PCR with specific primers (F, 5′-CGGTGCCAGCCGCGGTAATACG-3′; R, 5′-TACATAGAAGCCCCGAAGGAAGAC-3′) for a 520-bp P. gingivalis 16S rRNA fragment (21). We used 50-μl PCR mixes, which included approximately 200 ng of total genomic DNA, 3.5 U of Taq polymerase (Expand High Fidelity; Roche Applied Science), and primers and MgCl2 to final concentrations of 300 nM and 2 mM, respectively. Thermal cycler (Perkin-Elmer model 9600) conditions were set at 94°C for 2 min and 35 cycles of a 3-step PCR (94, 56, and 72°C for 1 min each), followed by a final elongation cycle of 72°C for 10 min. As an optimization step in the PCR approach, we sought to determine the detection threshold of the system by using pure P. gingivalis cultures. To this end, P. gingivalis cells were cultured for 3 days in Schaedler's broth and cell numbers were spectrophotometrically estimated as described above. Tenfold serial dilutions of P. gingivalis cells ranging from 106 to 101 CFU were then amplified by using the aforementioned conditions. DNA products were resolved in 1.2% agarose gel, stained with ethidium bromide, and analyzed through UV light.
Statistical analysis.
All of the en face and periodontal measurements were done in a blind fashion on coded samples, and the quantitative measurements were made twice. The extent of lipid deposit, periodontal disease, and other study parameters were analyzed by Student's t test (two tailed). A P value of ≤0.05 was considered significant. The relationship between the extent of lipid deposition and the extent of periodontal disease was analyzed by the Pearson correlation coefficient. All values in the text, tables, and figures are means ± standard errors of the means.
RESULTS
All animals survived the experiment. No clinical signs of infection or illness were noted in any of the animals at any time. Both groups of animals had comparable levels of total cholesterol in their sera. At baseline, the total level of cholesterol was 14 ± 4 and 13 ± 4 mg/dl in the control and test (i.e., periodontal disease) groups, respectively. After 14 weeks, the total cholesterol was 731 ± 349 and 858 ± 418 mg/dl, respectively. There were no significant differences in blood cell counts or body weight over the 14-week period (Table 1). The aorta of one animal in the test group was destroyed in processing and rendered unusable. It was excluded from the final analysis.
TABLE 1.
Cholesterol levels, blood cell counts, and body weight outcomes between groups throughout the studya
| Group time point | Cholesterol (mg/dl)b | leukocytes (103/μl) | Lymphocytes (103/μl) | Monocytes (103/μl) | Granulocytes (103/μl) | Wt (kg) |
|---|---|---|---|---|---|---|
| Control | ||||||
| Baseline | 14 ± 40 | 6 ± 0.80 | 4.16 ± 0.27 | 0.91 ± 0.47 | 0.91 ± 0.34 | 3.15 ± 0.07 |
| 14 wk | 731 ± 349 | 8.67 ± 2.63 | 6.47 ± 1.65 | 0.74 ± 0.41 | 1.75 ± 0.58 | 3.6 ± 0.24 |
| Periodontitis | ||||||
| Baseline | 13 ± 4 | 10.52 ± 3.04 | 7.46 ± 1.71 | 1.8 ± 1.2 | 1.26 ± 0.40 | 3.25 ± 0.13 |
| 14 wk | 858 ± 418 | 10.93 ± 2.44 | 8.2 ± 2.09 | 1.14 ± 0.10 | 1.59 ± 0.54 | 3.7 ± 0.33 |
Values are means ± standard errors of the means. Differences between control and periodontitis group results were not significant (P < 0.05).
Difference between 14-week and baseline values for both groups were significant (P < 0.01).
Morphometric analysis of bone levels.
Table 2 shows individual values for crestal bone level and proximal bone level in both groups at the end of the experiment. The mean crestal bone loss in the group with periodontal disease was significantly greater in the test group than in the control group. Similarly, the values for proximal bone loss were significantly different between the groups (P ≤ 0.05) (Table 2).
TABLE 2.
Changes in the periodontal supporting bone after 14 weeks in the periodontitis and control groups
| Group and rabbit | Mean bone loss (mm)a
|
% Tooth in bone | |
|---|---|---|---|
| Crestal | Proximal | ||
| Periodontitis | |||
| 54 | 4.41 | 4 | 84 |
| 55 | 3.76 | 3 | 81.35 |
| 56 | 10.24 | 6.75 | 53.4 |
| 57 | 7.67 | 5.75 | 67.7 |
| 58 | 5.16 | 5 | 68.75 |
| Mean ± SEM (n = 5) | <6.24 ± 2.67c | 4.9 ± 1.46b | 71.04 ± 12.16 |
| Mean ± SEM (n = 3) | 7.69 ± 2.54c | 5.8 ± 0.87b | 63.28 ± 8.5 |
| Control | |||
| 59 | 4.33 | 3 | 82.54 |
| 60 | 3.91 | 2.5 | 79.5 |
| 61 | 3.66 | 3.87 | 86.2 |
| 62 | 2.58 | 3.5 | 82.75 |
| 63 | 2.75 | 3.87 | 82.75 |
| 64 | 4.58 | 3.12 | 81.67 |
| Mean ± SEM (n = 5) | 3.63 ± 0.81 | 3.31 ± 0.53 | 82.56 ± 2.1 |
Expressed as the distance between a fixed reference point (tooth cusp tip) and the bone crest.
Significantly different from value for control group at a P of <0.05.
Significantly different from value for control group at a P of <0.005.
In the test group, the progression of periodontal destruction was not uniform. Two of the periodontal disease animals (animals 54 and 55) did not demonstrate any crestal or proximal bone loss. The values from these two animals were comparable to values from the group without induced periodontal disease. Hence, the data were analyzed twice; once including these animals in the periodontitis group and once without including them, and the analyses were corrected for multiple comparisons. The results for the crestal and proximal bone loss in the two groups still remained highly significant (P ≤ 0.05) (Table 2).
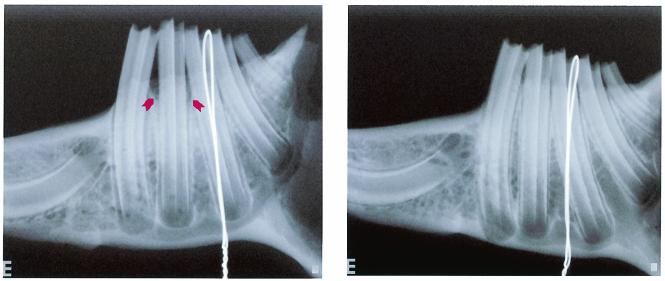
Radiographic analysis.
Radiographic bone loss in this model of periodontal disease is depicted in Fig. 1. There was a statistically significant (P < 0.05) loss of interproximal bone detected radiographically in the test group compared to the level of bone in the control group (Table 2). Again, if the two nonreacting animals (54 and 55) in the test group were dropped from the analysis, the significance level was ≤0.005.
FIG. 1.
Digital standardized radiograph of test (left panel) and control (right panel) animal jaws. The radiographs were taken with standardized alignment in three directions. The percentage of the tooth outside the bone was calculated according to a modified technique of Bjorn et al. (3). The left panel shows clear bone loss in the second premolar area (arrows).
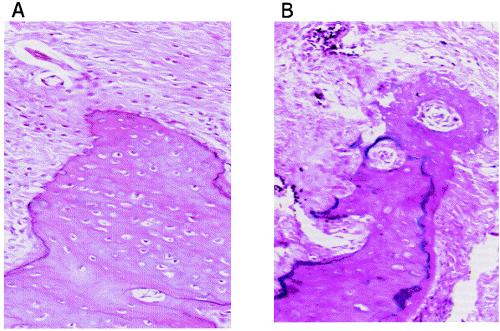
Histopathological analysis.
Histologic sections revealed increased cellular infiltration in the group with periodontal disease, which is characteristic of chronic periodontitis in humans. Additionally, alveolar bone resorption was evident, as was loss of connective tissue organization and connective tissue attachment to the teeth in the test group (Fig. 2). Rabbits 54 and 55 did not display increased cellular infiltration compared to the controls.
FIG. 2.
Histological assessment of bone resorption due to P. gingivalis application. Panel A shows cells from a control animal whose bone levels were not affected by the placement of the ligature plus vehicle. In contrast, panel B shows cells from an animal of the periodontitis group where resorption of the bone crest was observed in response to the placement of ligatures soaked with P. gingivalis. This animal developed severe aortic lipid deposition (hematoxylin and eosin staining; magnification, ×174).
Quantitation of aortic lipid deposits.
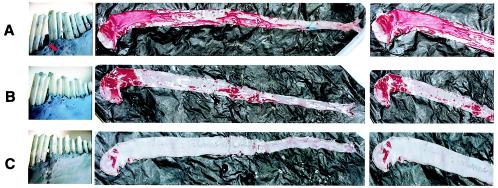
Figure 3 demonstrates the degrees of lipid deposition in the aortas of rabbits with and without periodontal disease. As shown in panel A, periodontitis and the accompanying bone loss were associated with extensive aortic lipid deposition. In contrast, the control animal in panel B demonstrated minimal lipid deposition. The association between periodontal disease and lipid deposition is also depicted in panel C; a rabbit in the test group that did not develop bone loss or periodontal disease also did not exhibit an increase in the deposition of lipid in its aorta. The mean percentages of the surface areas of the aortas covered by lipid plaque are summarized in Table 3. Animals 54 and 55 of the periodontitis group, the same ones that did not develop periodontitis, did not develop lipid deposits either. Again, statistical analyses were performed twice, excluding these two animals in the second analysis. It was observed that the group with periodontal disease had a greater extent of lipid deposition than did the group with no periodontal disease (P ≤ 0.05).
FIG. 3.
Representative results of periodontal lesion quantification and en face analysis. (A) Test group. The images show an extensive loss of bone in the second premolar area (arrow) and extensive coverage by atherosclerotic plaque of the same animal's aorta. (B) Control group. The images show the crestal bone with no loss around the second premolar and the aorta of the same animal, where minimal plaque is visible. (C) Test group. The images show the crestal bone from an animal that failed to develop any periodontal lesion and the same animal's aorta, which shows minimal plaque development as well.
TABLE 3.
Lipid deposition area analysis
| Group and animal | % Aortic surface area |
|---|---|
| Periodontitis | |
| 54 | 2.77 |
| 55 | 2.26 |
| 56 | 56.61 |
| 57 | 19.5 |
| 58 | 26.74 |
| Mean ± SEM (n = 3)a | 34.28 ± 19.67b |
| Mean ± SEM (n = 5) | 21.57 ± 22.27 |
| Control | |
| 59 | 17.3 |
| 60 | 4 |
| 61 | 12.46 |
| 62 | 10.8 |
| 63 | 5.71 |
| 64 | 17.63 |
| Mean ± SEM (n = 3) | 11.31 ± 5.6 |
Animals 54 and 55 failed to develop periodontal disease and lipid deposition and were therefore excluded from analysis.
Significantly different (P < 0.05) from value for control group.
Correlation between severity of periodontal disease and aortic lipid deposition.
The individual values of crestal bone level, proximal bone level, and percentage of tooth in bone in the periodontitis group were compared to the extent of lipid deposition by using the Pearson product correlation coefficient (r). All the parameters of periodontal lesion were found to correlate positively with the extent of lipid deposition (Table 4). Further, a direct correlation between the percentage of tooth exposed from the bone loss and the percentage of the aorta covered by lipid was observed (r2 = 0.9501). In other words, in the present trial, 95% of the variability of aortic lipid deposition can be explained by the severity of the periodontal disease as measured through bone loss assessment. These data provide the first direct evidence of periodontal disease influencing plaque and lipid accumulation in vivo.
TABLE 4.
Correlation analysis of the periodontitis group
| Measurement | Crestal bone loss
|
Proximal bone loss
|
% Tooth in bone
|
SAa
|
||||
|---|---|---|---|---|---|---|---|---|
| r | P | r | P | r | P | r | P | |
| Crestal bone loss | 1.000 | 0.947b | 0.014b | −0.929 | 0.022 | 0.896 | 0.040 | |
| Proximal bone loss | 0.947b | 0.014 | 1.000 | −0.932b | 0.021 | 0.898 | 0.038 | |
| % Tooth in bone | −0.929b | 0.022 | −0.932b | 0.021 | 1.000 | −0.975c | 0.005 | |
| SA | 0.896b | 0.040 | 0.898b | 0.038 | −0.975c | 0.005 | 1.000 | |
SA, surface area of the aorta covered by lipid deposits.
Significant correlation at a P of 0.05 (two tailed).
Significant correlation at a P of 0.01 (two tailed).
P. gingivalis 16S rRNA amplification by PCR.
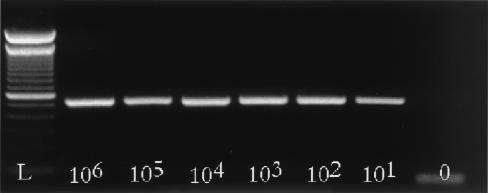
The minimum amplification detection threshold of the system observed in the PCR optimization procedure was 10 cells of P. gingivalis (Fig. 4). P. gingivalis 16S rRNA has not been amplified from genomic DNA obtained from any of the aortas analyzed by using the PCR-optimized conditions.
FIG. 4.
For PCR optimization, 10-fold serial dilutions of 3-day P. gingivalis cultures were amplified under the conditions described in the text. The conditions used in our study were able to detect P. gingivalis 16S rRNA genes from as few as 101 CFU obtained from a pure culture.
DISCUSSION
In this study we report that in the rabbit high-fat diet model, animals with experimentally induced periodontitis develop vascular lipid deposits to a greater extent than periodontally healthy controls. Further, there is a positive correlation between the extent of lipid deposition and the severity of periodontal disease. There is growing evidence linking periodontal disease and atherosclerosis on the epidemiologic level (2). Recently, a prospective study using a murine apoE knockout model revealed that repeated systemic injections of P. gingivalis contributed to the initiation and progression of lipid accumulation in major vessels (11). While the cardiovascular outcomes of that study were similar to the results reported here, there are several important differences between the two models. First, in the murine model, bacteria were recovered from the lipid lesions. Bacterial lesion recovery in the mouse model is most likely a result of the systemic intravenous injection of bacteria and the well-known fact that P. gingivalis can invade cells, especially endothelial cells (5). Further, the apoE knockout mouse is a genetically altered animal. The combination of the altered host response and the nonphysiologic introduction of an intravenous pathogen make it difficult to directly compare these experiments to human disease.
The present study was designed to test the hypothesis that the presence of periodontal disease modifies the development of atheromatous changes. Our aim was also to examine the mechanism by which periodontal disease might contribute to the development of the vascular lesions. As reported, we have developed an animal model in which both periodontal disease and atheromatous changes can be measured simultaneously. Our findings demonstrate that a diet consisting of 0.5% cholesterol can induce measurable lipid accumulation in the major vessels of the rabbit, and periodontal disease accelerates or increases lipid accumulation. The laboratory parameters measured, including peripheral blood cell counts and body weight, were not different between groups. There were no obvious systemic indicators of illness in the periodontitis group in spite of the topical application of the pathogen. This finding is consistent with observations from studies of human periodontal disease, which is also asymptomatic, without fever, weight loss, or other indicators of infection. It is interesting, however, that elevated C-reactive protein levels in periodontitis patients without cardiovascular disease have been reported (14). Importantly, in our study, there was no difference in the serum cholesterol levels between the two groups.
An interesting and unexpected outcome of the study was the varied levels of susceptibility of the rabbits to periodontal disease. This difference is, however, consistent with observations of humans, in whom the susceptibility to periodontal breakdown is quite varied, seemingly independent of the presence of pathogens, which are ubiquitous. In humans, this difference in levels of susceptibility is hypothesized to be linked to host response traits, with individuals with a robust innate immune response being more susceptible to disease (15). Of particular interest in the context of this work was the observation that two animals in the periodontitis group failed to develop periodontal disease and aortic lipid deposition. In these animals, periodontal infection might not have been successfully induced and thus atherosclerosis did not progress. Another possibility that should not be ruled out is that those animals were resistant to periodontal infection, which may in turn suggest a common susceptibility trait for the two diseases. To support the latter premise, however, more experiments would be necessary.
This is the first report of a positive correlation between the severity of periodontal disease and the extent of atheromatous vessel changes. There is precedent for a relationship between infection and atherosclerosis (8). It has been previously reported that an infectious agent anywhere in the body may lead to coactivation of the innate immune system, which accelerates atherosclerosis. Richardson et al. (17) have reported that atherosclerosis was accelerated in hypercholesterolemic rabbits simultaneously suffering from respiratory tract (but not vascular) infections with Pasteurella multocida. Based on these observations, it has been suggested that there may be an infectious component in the development of cardiovascular lesions. However, as noted by Libby et al. (12), human atheromas often lack any indication of the presence of infectious agents, and even if an infectious particle is present in the lesion, a pathogenic role is far from established for that organism.
Conversely, there is a body of evidence supported by our study that suggests that an elevated innate host response is a risk factor for cardiovascular disease and periodontitis. An important corollary to this observation is the suggestion that local inflammation can alter the systemic inflammatory state. As an example, the work of Pouliot and coworkers (16) revealed that initiation of isolated inflammation in the murine dorsal air pouch model resulted in an upregulation of COX-2 mRNA in the heart and lung. Taken together, the data support the hypothesis that the degree of the inflammatory response to insult or injury is a major determinant in the pathogenesis of inflammatory diseases, including periodontitis and cardiovascular disease. Moreover, while these traits are known to be under genetic control, the traits are also modifiable by environmental factors, such as bacteria, and local inflammation at a single site may modify the response trait at remote locations in the body.
In conclusion, we have provided prospective data suggesting a link between periodontitis and cardiovascular disease in an animal model. Further, the evidence suggests that focal inflammation in the oral cavity can have direct effects on the innate immune response in other organ systems by increasing the risk for inflammatory-cell-mediated tissue injury.
Acknowledgments
We thank Margaret Morrissey for her excellent technical assistance.
This study was supported by U.S. Public Health Service grant DE13499. Eraldo L. Batista, Jr., is supported by the CAPES Foundation, Brasilia, Brazil (grant BEX 1539/99-2).
The T. Van Dyke and G. Stahl laboratories contributed equally to this study.
Editor: J. D. Clements
REFERENCES
- 1.Beck, J., R. Garcia, G. Heiss, P. S. Vokonas, and S. Offenbacher. 1996. Periodontal disease and cardiovascular disease. J. Periodontol. 67:1123-1137. [DOI] [PubMed] [Google Scholar]
- 2.Beck, J. D., S. Offenbacher, R. Williams, P. Gibbs, and R. Garcia. 1998. Periodontitis: a risk factor for coronary heart disease? Ann. Periodontol. 3:127-141. [DOI] [PubMed] [Google Scholar]
- 3.Bjorn, H., A. Halling, and H. Thyberg. 1969. Radiographic assessment of marginal bone loss. Odontol. Revy 20:165-179. [PubMed] [Google Scholar]
- 4.Chiu, B., E. Viira, W. Tucker, and I. W. Fong. 1997. Chlamydia pneumoniae, cytomegalovirus, and herpes simplex virus in atherosclerosis of the carotid artery. Circulation 96:2144-2148. [DOI] [PubMed] [Google Scholar]
- 5.Deshpande, R. G., M. B. Khan, and C. A. Genco. 1998. Invasion of aortic and heart endothelial cells by Porphyromonas gingivalis. Infect. Immun. 66:5337-5343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Haraszthy, V. I., J. J. Zambon, M. Trevisan, M. Zeid, and R. J. Genco. 2000. Identification of periodontal pathogens in atheromatous plaques. J. Periodontol. 71:1554-1560. [DOI] [PubMed] [Google Scholar]
- 7.Kuvin, J. T., and C. D. Kimmelstiel. 1999. Infectious causes of atherosclerosis. Am. Heart J. 137:216-226. [DOI] [PubMed] [Google Scholar]
- 8.Lehr, H. A., and K. Kawasaki. 1992. Aggravation of ischaemia-reperfusion injury in the striated muscle microcirculation by acute endotoxemia, p. 449-452. In E. Faist, J. L. Meakins, and F. W. Schildberg (ed.), Host defense dysfunctions in trauma, shock, and sepsis. Springer-Verlag, Heidelberg, Germany.
- 9.Lehr, H. A., D. A. Mankoff, D. Corwin, G. Santeusanio, and A. M. Gown. 1997. Application of Photoshop-based image analysis to quantification of hormone receptor expression in breast cancer. J. Histochem. Cytochem. 45:1559-1565. [DOI] [PubMed] [Google Scholar]
- 10.Lepine, G., and A. Progulske-Fox. 1996. Duplication and differential expression of hemagglutinin genes in Porphyromonas gingivalis. Oral Microbiol. Immunol. 11:65-78. [DOI] [PubMed] [Google Scholar]
- 11.Li, L., E. Messas, E. L. Batista, Jr., R. A. Levine, and S. Amar. 2002. Porphyromonas gingivalis infection accelerates the progression of atherosclerosis in a heterozygous apolipoprotein E-deficient murine model. Circulation 105:861-867. [DOI] [PubMed] [Google Scholar]
- 12.Libby, P., D. Egan, and S. Skarlatos. 1997. Roles of infectious agents in atherosclerosis and restenosis: an assessment of the evidence and need for future research. Circulation 96:4095-4103. [DOI] [PubMed] [Google Scholar]
- 13.Marcus, A. J., and D. P. Hajjar. 1993. Vascular transcellular signaling. J. Lipid Res. 34:2017-2031. [PubMed] [Google Scholar]
- 14.Noack, B., R. J. Genco, M. Trevisan, S. Grossi, J. J. Zambon, and E. De Nardin. 2001. Periodontal infections contribute to elevated systemic C-reactive protein level. J. Periodontol. 72:1221-1227. [DOI] [PubMed] [Google Scholar]
- 15.Page, R. C., S. Offenbacher, H. E. Schroeder, G. J. Seymour, and K. S. Kornman. 1997. Advances in the pathogenesis of periodontitis: summary of developments, clinical implications and future directions. Periodontol. 2000 14:216-248. [DOI] [PubMed] [Google Scholar]
- 16.Pouliot, M., C. B. Clish, N. A. Petasis, T. E. Van Dyke, and C. N. Serhan. 2000. Lipoxin A(4) analogues inhibit leukocyte recruitment to Porphyromonas gingivalis: a role for cyclooxygenase-2 and lipoxins in periodontal disease. Biochemistry 39:4761-4768. [DOI] [PubMed] [Google Scholar]
- 17.Richardson, M., M. De Reske, K. Delaney, A. Fletch, L. H. Wilcox, and R. L. Kinlough-Rathbone. 1997. Respiratory infection in lipid-fed rabbits enhances sudanophilia and the expression of VCAM-1. Am. J. Pathol. 151:1009-1017. [PMC free article] [PubMed] [Google Scholar]
- 18.Ross, R. 1999. Atherosclerosis is an inflammatory disease. Am. Heart J. 138:S419-S420. [DOI] [PubMed] [Google Scholar]
- 19.Shah, P. K. 1999. Plaque disruption and thrombosis. Potential role of inflammation and infection. Cardiol. Clin. 17:271-281. [DOI] [PubMed] [Google Scholar]
- 20.Silver, J. G., A. W. Martin, and B. C. McBride. 1977. Experimental transient bacteraemias in human subjects with varying degrees of plaque accumulation and gingival inflammation. J. Clin. Periodontol. 4:92-99. [DOI] [PubMed] [Google Scholar]
- 21.Slots, J., A. Ashimoto, M. J. Flynn, G. Li, and C. Chen. 1995. Detection of putative periodontal pathogens in subgingival specimens by 16S ribosomal DNA amplification with the polymerase chain reaction. Clin. Infect. Dis. 20(Suppl.):S304-S307. [DOI] [PubMed] [Google Scholar]
- 22.Sztukowska, M., M. Bugno, J. Potempa, J. Travis, and D. M. Kurtz, Jr. 2002. Role of rubrerythrin in the oxidative stress response of Porphyromonas gingivalis. Mol. Microbiol. 44:479-488. [DOI] [PubMed] [Google Scholar]
- 23.Warford, A. 1996. In situ hybridisation, p. 491-512. In J. D. Bancroft (ed.), Theory and practice of histological techniques, 4th ed. Churchill Livingstone, London, United Kingdom.