Abstract
The contribution of murine Toll-like receptors 2 and 4 (TLR2 and -4, respectively) to cytokine induction by heat-killed bacteria was analyzed in vitro and in vivo. Gram-negative bacteria induced cytokines primarily via TLR4; the contribution of TLR2 was only minor. Neither TLR4 nor, surprisingly, TLR2 was required in the MyD88-dependent response to Staphylococcus aureus.
Highly conserved microbial components such as lipopolysaccharide (LPS), lipopeptides (LPs), lipoteichoic acids (LTAs), and peptidoglycan (PGN) serve as markers for the recognition of pathogens by Toll-like receptors (TLRs) in mammals (4, 14, 19, 23, 24, 26, 28, 32). The interaction of these components with TLRs on cells of the innate immune system induces the production of cytokines and other endogenous mediators essential for antimicrobial defense. TLR4 serves as signaling receptor for LPS (5, 15, 23), and TLR2 serves as the signaling receptor for molecules such as LP, LTA, and PGN (22). In mice, both TLR4- and TLR2-mediated responses to LPS and to bacterial LPs, respectively, can be strongly enhanced by priming with live or killed pathogens (9-11), such as Propionibacterium acnes (13, 16). This pathogen-induced hypersensitivity is gamma interferon (IFN-γ) mediated (8, 16). Hypersensitive mice overproduce tumor necrosis factor alpha (TNF-α) and interleukin-6 (IL-6) upon challenge and exhibit an enhanced susceptibility to the lethal activity of LPS, LP, and TNF-α. Priming with P. acnes also induces a weak, IFN-γ-independent sensitization to Staphylococcus aureus and to components of gram-negative bacteria other than LPS (20).
In this study, we analyzed the relative contributions of TLR2 and TLR4 to the bacterial induction of IL-6 and TNF-α in macrophages in vitro and in unsensitized and P. acnes-sensitized mice in vivo, using C57BL/10 animals deficient in TLR2, TLR4, or both. Wild-type C57BL/10ScSn and C57BL/6 mice and TLR4-deficient C57BL/10ScN (21, 29) mice were bred in the animal facilities of the Max-Planck-Institut. TLR2-deficient mice (30), provided by Tularik, Inc., South San Francisco, Calif., were backcrossed six times to either C57BL/10ScSn mice to obtain TLR2 single-deficient mice or to C57BL/10ScN mice to obtain TLR2/TLR4 double-deficient mice. MyD88-deficient mice (1) were provided by S. Akira (Research Institute for Microbial Diseases, Osaka, Japan). Heat-killed Salmonella enterica serovar Typhimurium and P. acnes (strain ATCC 12930) were prepared as described previously (25). A laboratory strain of S. aureus and two fresh clinical isolates of methicillin-sensitive S. aureus, provided by K. Pelz and R. Engelhardt (Institute for Medical Microbiology and Hygiene, Freiburg, Germany), were used. The bacteria were grown overnight in Trypticase soy broth (Difco Laboratories, Detroit, Mich.) at 37°C and then washed and heat killed (56°C for 1 h).
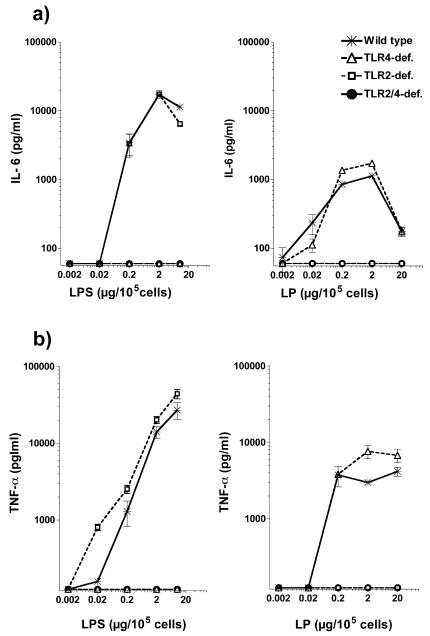
IL-6 and TNF-α responses served as a measure of macrophage sensitivity to the bacterial agents used. Mouse macrophages obtained in vitro from bone marrow precursors (7) were stimulated in triplicate with graded amounts of bacterial components or whole bacteria (in 10 μl per well), and culture supernatants were collected 4 and 24 h later for TNF-α and IL-6 measurements, respectively. TNF-α in cell supernatants was measured with a bioassay (2, 6), and IL-6 was measured with an enzyme-linked immunosorbent assay (PharMingen, San Diego, Calif.). Figures 1 and 2 show the results obtained with macrophages from wild-type and TLR2- and TLR4-deficient mice stimulated with different agents. There was a strict requirement for TLR4 and TLR2 in the responses of the macrophages to LPS and LP, respectively (Fig. 1). As expected, LPS of S. enterica serovar Typhimurium (12) induced dose-dependent IL-6 and TNF-α responses (Fig. 1, left) only in wild-type and TLR2-deficient macrophages, while LP (Pam3Cys-Ser-Lys4; EMC Microcollections GmbH, Tübingen, Germany) induced such responses only in wild-type and TLR4-deficient cells (Fig. 1, right).
FIG. 1.
Role of TLR4 and TLR2 in the IL-6 response of macrophages to LPS or synthetic LP (Pam3CysSK4). Bone marrow-derived macrophages of wild-type, TLR4-deficient, TLR2-deficient, and TLR2/TLR4 double-deficient mice were stimulated with different amounts of LPS (left panels) or LP (right panels) for 4 h (TNF-α) and 24 h (IL-6). IL-6 (a) and TNF-α (b) were measured in cell supernatants. One representative experiment of 10 is shown.
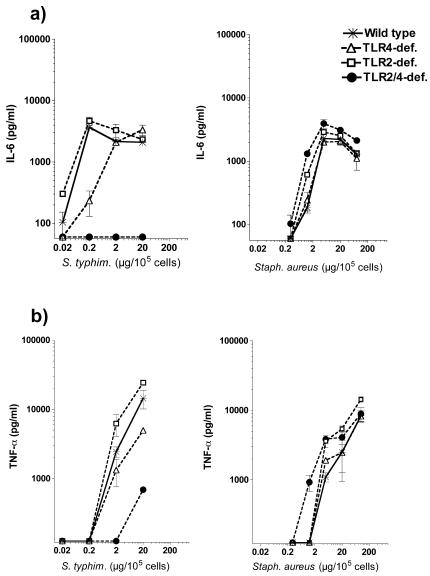
FIG. 2.
Role of TLR4 and TLR2 in the IL-6 and TNF-α responses of macrophages to heat-killed S. enterica serovar Typhimurium and S. aureus. Bone marrow-derived macrophages of wild-type, TLR4-deficient, TLR2-deficient, and TLR2/TLR4 double-deficient mice were stimulated with different amounts of heat-killed S. enterica serovar Typhimurium (left panels) or S. aureus (right panels) for 4 h (TNF-α) and 24 h (IL-6). IL-6 (a) and TNF-α (b) were measured in cell supernatants. One representative experiment of 10 is shown.
The cytokine responses to S. enterica serovar Typhimurium were mediated predominantly by TLR4 and to a minor extent by TLR2 (Fig. 2, left). The responses were markedly lower in the absence of TLR4 but not in the absence of TLR2. The concomitant absence of both receptors further reduced the TNF-α response and abolished the IL-6 response completely. Results similar to these were also obtained with heat-killed Escherichia coli, Proteus mirabilis, Pseudomonas aeruginosa, Pseudomonas saccharophila, S. enterica serovar Minnesota S form, S. enterica serovar Minnesota R595 (Re), S. enterica serovar Typhi, and S. enterica serovar Enteritidis (data not shown). Thus, LPS plays a dominant role in the cytokine response of macrophages to gram-negative bacteria. Furthermore, almost the entire cytokine-inducing activity of gram-negative bacteria in macrophages is TLR4 and TLR2 dependent.
The IL-6 and TNF-α responses of the different types of macrophages to S. aureus were not significantly different, regardless of the presence or absence of TLR2 or TLR4, (Fig. 2). This was true for different experiments in which a laboratory strain and two fresh clinical isolates of S. aureus were used. This indicates that the activation of macrophages by S. aureus is independent of TLR2 and TLR4.
To the contrary, in a previous study (27), TLR2-deficient macrophages produced reduced amounts of TNF-α and IL-6 in response to heat-killed S. aureus. Of note, in the study described above, different type of macrophages were used, only a single dose of bacteria was examined, and there was no information about whether the TLR2-deficient mice used were backcrossed to a defined background. However, that study also indicated the involvement of an additional signaling receptor(s) in the response to S. aureus.
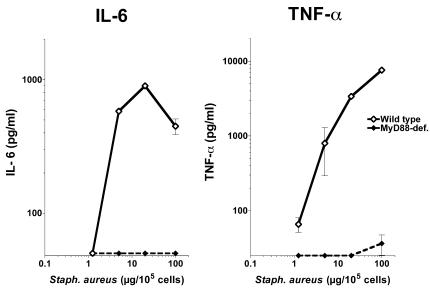
MyD88 is an important adapter protein common to signaling pathways via members of TLR family (17). We therefore examined the responsiveness of MyD88-deficient and wild-type macrophages to S. aureus. As shown in Fig. 3, the absence of MyD88 completely abolished the IL-6 and TNF-α responses of macrophages to S. aureus. This shows, in agreement with previous results (27), that a MyD88-dependent signaling pathway is essential for the recognition of S. aureus and suggests the involvement of a TLR distinct from TLR2 and TLR4.
FIG. 3.
Role of MyD88 in the IL-6 and TNF-α responses of macrophages to heat-killed S. aureus. Bone marrow-derived macrophages of wild-type (C57BL/6) and MyD88-deficient mice were stimulated with different amounts of heat-killed S. aureus for 4 h (TNF-α) and 24 h (IL-6). IL-6 and TNF-α were measured in cell supernatants. One representative experiment of two is shown.
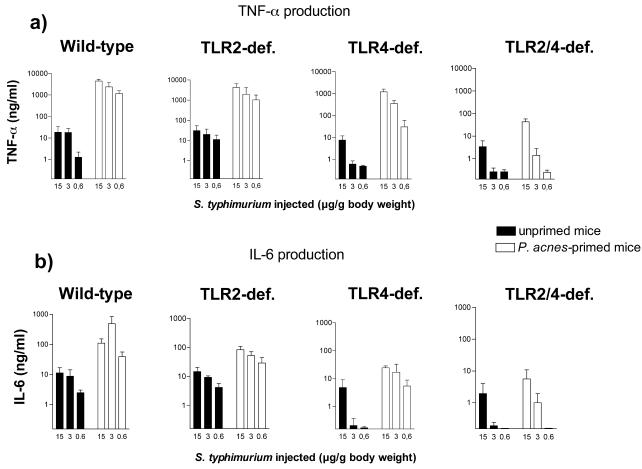
Generally, macrophages may be divided into different types with distinct biological properties according to their location and function (18). It may therefore be assumed that the relative importance of TLRs for bacterial recognition is different in different macrophage types and might at least in part differ from that in the macrophages used in the present study. Furthermore, in vivo, in addition to macrophages, other cell types may contribute to the cytokine release induced by bacteria. For this reason, we also investigated the importance of the two TLRs in the systemic cytokine response of mice to S. enterica serovar Typhimurium and S. aureus. Groups of unsensitized and P. acnes-sensitized (16) wild-type and TLR4-, TLR2-, and TLR4/TLR2 double-deficient mice were challenged intravenously with different amounts of bacteria. Thereafter, TNF-α and IL-6 responses were determined in plasma collected 1 and 2 h after challenge. In unsensitized mice, the absence of TLR4 substantially reduced the cytokine response to S. typhimurium (Fig. 4). An additional absence of TLR2 in TLR2/TLR4 double-deficient mice lowered this response further (P values for comparison of TNF-α response of TLR4-deficient to TLR2/TLR4 double-deficient mice: 15 μg/g, 0.024; 3 μg/g, 0.002; and 0.6 μg/g, 0.0096). Generally, P. acnes-sensitized mice challenged with S. enterica serovar Typhimurium produced higher cytokine levels than the respective unsensitized animals (Fig. 4). The absence of TLR2 alone had no effect on the enhanced responses to S. enterica serovar Typhimurium, while the absence of TLR4 substantially reduced these responses. Furthermore, the combined deficiency of both TLRs resulted in an extensive loss of responsiveness. Altogether, the results obtained in vivo and in vitro show that the cytokine responses to gram-negative pathogens are dependent predominantly on TLR4 and, to a much lesser extent, on TLR2. The identities of the TLR2-dependent ligand or ligands of gram-negative bacteria were not addressed here, but lipoproteins are likely candidates (3, 33). The secondary role of TLR2 may be explained by a low concentration or little accessibility (31) of the respective ligands in bacteria. Alternatively, the signal transduction efficacy of the TLR2 in bone marrow-derived macrophages may be lower than that of TLR4. The finding that the synthetic LP was less efficient than LPS in inducing cytokines in macrophages supports this idea.
FIG. 4.
Roles of TLR4 and TLR2 in the TNF-α and IL-6 responses to S. enterica serovar Typhimurium in unprimed and P. acnes-primed mice. Wild-type, TLR4-deficient (def.), TLR2-deficient, and TLR2/TLR4 double-deficient mice (6 to 9 animals per group) were injected intravenously with P. acnes (25 μg/g of body weight) or remained untreated (control). Seven days later, all mice were challenged with different amounts of S. enterica serovar Typhimurium. Plasma was collected 1 h (TNF-α) and 2 h (IL-6) after challenge.
The inducibility of enhanced cytokine responses to S. enterica serovar Typhimurium in P. acnes-primed TLR2-deficient mice excludes a major role for TLR2 in the actual mechanism of sensitization. A major role for TLR4 in sensitization was excluded earlier (20). This is useful information, since the innate receptors involved in the P. acnes-mediated sensitization have not been identified yet.
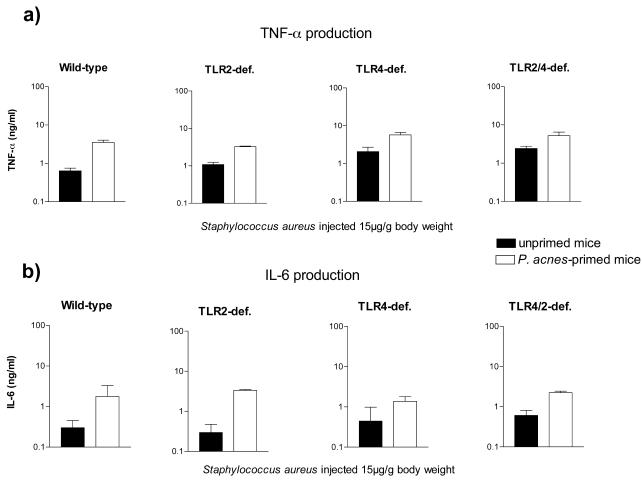
S. aureus (Fig. 5) was a much weaker inducer of TNF-α and IL-6 than S. enterica serovar Typhimurium (Fig. 4) in P. acnes-primed and unprimed mice, respectively. Furthermore, the responses of primed and unprimed TLR2-, TLR4-, and TLR2/TLR4 double-deficient mice were not reduced (Fig. 5), indicating that the latter were neither TLR2 nor TLR4 dependent. TLR2-independent cytokine induction by S. aureus is also strongly suggested by the weak activity of S. aureus in P. acnes-primed mice. As shown previously, P. acnes priming strongly enhances TLR2-mediated cytokine responses by 2 orders of magnitude (20).
FIG. 5.
Role of TLR4 and TLR2 in the TNF-α and IL-6 response to S. aureus in unprimed and P. acnes-primed mice. Wild-type, TLR4-deficient, TLR2-deficient, and TLR2/TLR4 double-deficient mice (6 to 9 animals per group) were injected intravenously with P. acnes (25 μg/g of body weight) or remained untreated (control). Seven days later, all mice were challenged with S. aureus (15 μg/g of body weight). Plasma was collected 1 h (TNF-α) and 2 h (IL-6) after challenge.
In conclusion, a MyD88-dependent receptor or receptors distinct from TLR2 and TLR4 are implicated in the induction of TNF-α and IL-6 by S. aureus. Consequently, TLR2-dependent components such as PGN and LTA are not involved in this effect. An attempt to identify the receptor in question by using HEK293 cells ectopically expressing one or more different TLRs (TLR1 to -9) together with CD14 and MD-2 so far has been unsuccessful (data not shown). However, a possible lack of unknown coreceptor molecules in HEK293 cells might have been responsible. Further investigations are required to identify the receptors involved in the cytokine responses of S. aureus.
Acknowledgments
We are grateful to Jasmin Kühnle, Hella Stübig, Helga Kochanowski, and Nadja Goos for excellent technical assistance.
This study was partly supported by DFG, SP “Angeborene Immunität” (FR 448/4-1).
Editor: F. C. Fang
REFERENCES
- 1.Adachi, O., T. Kawai, K. Takeda, M. Matsumoto, H. Tsutsui, M. Sakagami, K. Nakanishi, and S. Akira. 1998. Targeted disruption of the MyD88 gene results in loss of IL-1- and IL-18-mediated function. Immunity 9:143-150. [DOI] [PubMed] [Google Scholar]
- 2.Aggarwal, B. B., W. J. Kohr, P. E. Hass, B. Moffat, S. A. Spencer, W. J. Henzel, T. S. Bringman, G. E. Nedwin, D. V. Goeddel, and R. N. Harkins. 1985. Human tumor necrosis factor. Production, purification, and characterization. J. Biol. Chem. 260:2345-2354. [PubMed] [Google Scholar]
- 3.Aliprantis, A. O., D. S. Weiss, J. D. Radolf, and A. Zychlinsky. 2001. Release of Toll-like receptor-2-activating bacterial lipoproteins in Shigella flexneri culture supernatants. Infect. Immun. 69:6248-6255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Aliprantis, A. O., R. B. Yang, M. R. Mark, S. Suggett, B. Devaux, J. D. Radolf, G. R. Klimpel, P. Godowski, and A. Zychlinsky. 1999. Cell activation and apoptosis by bacterial lipoproteins through toll-like receptor-2. Science 285:736-739. [DOI] [PubMed] [Google Scholar]
- 5.Beutler, B., X. Du, and A. Poltorak. 2001. Identification of Toll-like receptor 4 (Tlr4) as the sole conduit for LPS signal transduction: genetic and evolutionary studies. J. Endotoxin Res. 7:277-280. [PubMed] [Google Scholar]
- 6.Freudenberg, M. A., and C. Galanos. 1991. Tumor necrosis factor alpha mediates lethal activity of killed gram-negative and gram-positive bacteria in d-galactosamine-treated mice. Infect. Immun. 59:2110-2115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Freudenberg, M. A., D. Keppler, and C. Galanos. 1986. Requirement for lipopolysaccharide-responsive macrophages in galactosamine-induced sensitization to endotoxin. Infect. Immun. 51:891-895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Freudenberg, M. A., M. Kopf, and C. Galanos. 1996. Lipopolysaccharide-sensitivity of interferon-gamma-receptor deficient mice. J. Endotoxin. Res. 3:291-295. [Google Scholar]
- 9.Freudenberg, M. A., T. Merlin, M. Gumenscheimer, C. Kalis, R. Landmann, and C. Galanos. 2001. Role of lipopolysaccharide susceptibility in the innate immune response to Salmonella typhimurium infection: LPS, a primary target for recognition of Gram-negative bacteria. Microbes Infect. 3:1213-1222. [DOI] [PubMed] [Google Scholar]
- 10.Galanos, C., M. A. Freudenberg, M. Matsuura, and A. Coumbos. 1988. Hypersensitivity to endotoxin and mechanisms of host-response. Prog. Clin. Biol. Res. 272:295-308. [PubMed] [Google Scholar]
- 11.Galanos, C., M. Gumenscheimer, P. Muhlradt, E. Jirillo, and M. Freudenberg. 2000. MALP-2, a Mycoplasma lipopeptide with classical endotoxic properties: end of an era of LPS monopoly? J. Endotoxin Res. 6:471-476. [PubMed] [Google Scholar]
- 12.Galanos, C., O. Luderitz, and O. Westphal. 1979. Preparation and properties of a standardized lipopolysaccharide from Salmonella abortus equi (Novo-Pyrexal). Zentbl. Bakteriol. Orig A 243:226-244. [PubMed] [Google Scholar]
- 13.Halpern, B. N., A.-R. Prévot, G. Biozzi, C. Stifel, D. Mouton, J. C. Morard, Y. Bouthillier, and C. Decreusefond. 1964. Stimulation de l'activité phagocytaire du systéme réticuloendothélial provoquée par Corynebacterium parvum RES. J. Reticuloendothel. Soc. 1:77-96. [PubMed] [Google Scholar]
- 14.Janeway, C. A., Jr. 1989. Approaching the asymptote? Evolution and revolution in immunology. Cold Spring Harbor Symp. Quant. Biol. 54:1-13. [DOI] [PubMed] [Google Scholar]
- 15.Kalis, C., B. Kanzler, A. Lembo, A. Poltorak, C. Galanos, and M. A. Freudenberg. 2003. Toll-like receptor 4 expression levels determine the degree of LPS-susceptibility in mice. Eur. J. Immunol. 33:798-805. [DOI] [PubMed] [Google Scholar]
- 16.Katschinski, T., C. Galanos, A. Coumbos, and M. A. Freudenberg. 1992. Gamma interferon mediates Propionibacterium acnes-induced hypersensitivity to lipopolysaccharide in mice. Infect. Immun. 60:1994-2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kawai, T., O. Adachi, T. Ogawa, K. Takeda, and S. Akira. 1999. Unresponsiveness of MyD88-deficient mice to endotoxin. Immunity 11:115-122. [DOI] [PubMed] [Google Scholar]
- 18.Laskin, D. L., B. Weinberger, and J. D. Laskin. 2001. Functional heterogeneity in liver and lung macrophages. J. Leukoc. Biol. 70:163-170. [PubMed] [Google Scholar]
- 19.Medzhitov, R., and C. A. Janeway, Jr. 1997. Innate immunity: the virtues of a nonclonal system of recognition. Cell 91:295-298. [DOI] [PubMed] [Google Scholar]
- 20.Merlin, T., M. Gumenscheimer, C. Galanos, and M. A. Freudenberg. 2001. TNF-alpha hyper-responses to Gram-negative and Gram-positive bacteria in Propionibacterium acnes primed or Salmonella typhimurium infected mice. J. Endotoxin Res. 7:157-163. [PubMed] [Google Scholar]
- 21.Merlin, T., A. Sing, P. J. Nielsen, C. Galanos, and M. A. Freudenberg. 2001. Inherited IL-12 unresponsiveness contributes to the high LPS resistance of the Lps(d) C57BL/10ScCr mouse. J. Immunol. 166:566-573. [DOI] [PubMed] [Google Scholar]
- 22.Ozinsky, A., D. M. Underhill, J. D. Fontenot, A. M. Hajjar, K. D. Smith, C. B. Wilson, L. Schroeder, and A. Aderem. 2000. The repertoire for pattern recognition of pathogens by the innate immune system is defined by cooperation between toll-like receptors. Proc. Natl. Acad. Sci. USA 97:13766-13771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Poltorak, A., X. He, I. Smirnova, M. Y. Liu, C. V. Huffel, X. Du, D. Birdwell, E. Alejos, M. Silva, C. Galanos, M. Freudenberg, P. Ricciardi-Castagnoli, B. Layton, and B. Beutler. 1998. Defective LPS signaling in C3H/HeJ and C57BL/10ScCr mice: mutations in Tlr4 gene. Science 282:2085-2088. [DOI] [PubMed] [Google Scholar]
- 24.Schwandner, R., R. Dziarski, H. Wesche, M. Rothe, and C. J. Kirschning. 1999. Peptidoglycan- and lipoteichoic acid-induced cell activation is mediated by toll-like receptor 2. J. Biol. Chem. 274:17406-17409. [DOI] [PubMed] [Google Scholar]
- 25.Sing, A., T. Merlin, H.-P. Knopf, P. J. Nielsen, H. Loppnow, C. Galanos, and M. A. Freudenberg. 2000. Bacterial induction of beta interferon in mice is a function of the lipopolysaccharide component. Infect. Immun. 68:1600-1607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Takeda, K., T. Kaisho, and S. Akira. 2003. Toll-like receptors. Annu. Rev. Immunol. 21:335-376. [DOI] [PubMed] [Google Scholar]
- 27.Takeuchi, O., K. Hoshino, and S. Akira. 2000. Cutting edge: TLR2-deficient and MyD88-deficient mice are highly susceptible to Staphylococcus aureus infection. J. Immunol. 165:5392-5396. [DOI] [PubMed] [Google Scholar]
- 28.Takeuchi, O., K. Hoshino, T. Kawai, H. Sanjo, H. Takada, T. Ogawa, K. Takeda, and S. Akira. 1999. Differential roles of TLR2 and TLR4 in recognition of gram-negative and gram-positive bacterial cell wall components. Immunity 11:443-451. [DOI] [PubMed] [Google Scholar]
- 29.Vogel, S. N., C. T. Hansen, and D. L. Rosenstreich. 1979. Characterization of a congenitally LPS-resistant, athymic mouse strain. J. Immunol. 122:619-622. [PubMed] [Google Scholar]
- 30.Werts, C., R. I. Tapping, J. C. Mathison, T. H. Chuang, V. Kravchenko, I. Saint Girons, D. A. Haake, P. J. Godowski, F. Hayashi, A. Ozinsky, D. M. Underhill, C. J. Kirschning, H. Wagner, A. Aderem, P. S. Tobias, and R. J. Ulevitch. 2001. Leptospiral lipopolysaccharide activates cells through a TLR2-dependent mechanism. Nat. Immunol. 2:346-352. [DOI] [PubMed] [Google Scholar]
- 31.Wu, H. C. 1996. Biosynthesis of lipoproteins, p. 1005-1014. In F. C. Neidhardt, R. Curtiss III, J. L. Ingraham, E. C. C. Lin, K. B. Low, B. Magasanik, W. S. Reznikoff, M. Riley, M. Schaechter, and H. E. Umbarger (ed.), Escherichia coli and Salmonella. Cellular and molecular biology, 2nd ed., vol. 1. ASM Press, Washington, D.C.
- 32.Yoshimura, A., E. Lien, R. R. Ingalls, E. Tuomanen, R. Dziarski, and D. Golenbock. 1999. Cutting edge: recognition of Gram-positive bacterial cell wall components by the innate immune system occurs via Toll-like receptor 2. J. Immunol. 163:1-5. [PubMed] [Google Scholar]
- 33.Zhang, H., D. W. Niesel, J. W. Peterson, and G. R. Klimpel. 1998. Lipoprotein release by bacteria: potential factor in bacterial pathogenesis. Infect. Immun. 66:5196-5201. [DOI] [PMC free article] [PubMed] [Google Scholar]