Abstract
Cryptococcus neoformans is an encapsulated fungus that is a major cause of meningitis in patients with AIDS. In immunocompetent mice, administration of IgG1 mAb protects against cryptococcal infection, whereas administration of IgG3 is not protective and can accelerate the infection. In beige mice with impaired natural killer cell function, the effects of IgG1 and IgG3 are similar to those observed in immunocompetent mice, suggesting that natural killer cells are not crucial for antibody-mediated modulation of cryptococcal infection. In mice lacking CD4+ T cells, IgG1 is not protective and IgG3 accelerates infection, indicating that CD4+ T cells are required for antibody-mediated protection. In mice lacking CD8+ T cells, both IgG1 and IgG3 antibodies prolong survival, indicating that acceleration of the disease process by IgG3 involves CD8+ T cells. Both IgG1-mediated protection and IgG3-mediated acceleration of infection require interferon γ. These results reveal a functional dependence of passively administered antibody on cellular immunity in cryptococcal infection in mice and have implications for antibody-based therapies in humans in the setting of CD4+ lymphopenia.
Cryptococcus neoformans is a ubiquitous fungus that causes a life-threatening meningoencephalitis in 6–8% of patients with AIDS (1). The disease usually occurs in patients with very low CD4+ T cell counts (1). Once established, C. neoformans infections are usually incurable in immunocompromised individuals, and patients with AIDS require lifelong therapy to prevent relapse (2–4). The difficulties associated with the management of cryptococcal infections in patients with AIDS have stimulated interest in the potential of antibody immunity for prevention and adjunctive therapy (5).
Immunization with cryptococcal capsular glucuronoxylomannan (GXM)-protein-conjugates and infection with C. neoformans can elicit both protective and nonprotective antibodies in mice (6–8). Previous studies have demonstrated that mAbs of the IgG3 subclass were not protective in various mouse models of cryptococcal infection (8, 9). When the 3E5 IgG3 mAb was switched to the IgG1 isotype, the IgG1 switch variant was protective (8). It is not obvious why IgG3 and IgG1 should have such different effects on C. neoformans because both isotypes protect mice from infection with Streptococcus pneumoniae, another encapsulated infectious agent (10). The avidity of the nonprotective 3E5 IgG3 for GXM is higher than its IgG1 switch variant (8), presumably because it polymerizes after binding to antigen (11). The half-life of the two isotypes in the circulation is the same (12), and both IgG3 and IgG1 are opsonic (13), fix complement (14), and can facilitate macrophage-mediated killing of tumor cells in vitro (15). However, the IgG3 and IgG1 isotypes bind to different Fc receptors on mouse macrophages (13), and this may be the basis for their different efficacies against C. neoformans.
In this study, we have investigated the efficacy of administration of IgG3 and IgG1 mAb in mice deficient in natural killer (NK) cells, CD4+ and CD8+ T cells, and interferon γ (IFN-γ) in preventing infection with C. neoformans. Previous studies have shown that each of these cell types and IFN-γ contribute to the host defense against this organism (16–21). Our results using mice with inherited defects in CD4+ and CD8+ cells and IFN-γ confirm and extend those findings. By administering antibodies to these immunodeficient mice, we have shown that T cells and IFN-γ, but not NK cells, are necessary for antibody-mediated protection and enhancement of cryptococcal infection. These results indicate that the CD4/CD8 ratio is very important in determining how antibodies modulate infections with C. neoformans, and perhaps with other infectious agents as well.
MATERIALS AND METHODS
C. neoformans.
Strain 24067 (serotype D) was obtained from the American Type Culture Collection and maintained on Sabouraud dextrose agar (Difco) at 4°C. For murine infection, C. neoformans was grown at 37°C in Sabouraud dextrose broth (Difco) for 24 hr. Yeast cells were washed three times with PBS, and the inoculum was determined by counting in a hemocytometer.
mAbs.
The 3E5 IgG3 was made in response to immunization with GXM-conjugated to tetanus toxoid (6, 22). The IgG1 switch variant of 3E5 (3E5 IgG1) was generated by in vitro isotype switching (23). The variable region sequences of both mAbs are identical (8), and both antibodies bind GXM (8). Ascites was obtained by injecting 107 hybridoma cells into the peritoneal cavity of Pristane-primed (Sigma) BALB/c mice. Antibody concentration was determined by ELISA relative to isotype-matched standards of known concentration.
Animal Experiments.
Female C57BL/6J, BALB/c, β2-microglobulin−/− (24) and beige mice (C57BL/6 bg/bg) (25, 26) were purchased from The Jackson Laboratory. SCID (27) and other immunodeficient mice were bred in a barrier facility in the Cancer Center at Albert Einstein College of Medicine. CD4−/− mice (C2DTM) (28) and wild-type controls were purchased from GenPharm (Mountain View, CA). Breeding pairs for IFN-γ knockout mice (GKO) (29) were obtained from Genentech, and CD8−/− mice (30) were provided by Tak Mak and the Amgen Institute (Ontario Cancer Institute, Toronto, Ontario, Canada) through Barry R. Bloom (Albert Einstein College of Medicine, Bronx, NY). Mice were used at 6 weeks of age. Ten mice per group were given either 1 mg of IgG1, IgG3, or PBS as a control. mAbs were administered through i.p. injection 24 hr before i.v. challenge with 5 × 106 C. neoformans, and mouse deaths were recorded daily.
Organ Colony-Forming Units (cfu) and Serum GXM Levels.
To determine the role of IFN-γ in antibody-mediated modulation of cryptococcal infection, groups of five CD4−/− mice were given 5 × 104 units of IFN-γ (Genzyme) per mouse i.p and treated with 1 mg of IgG1, IgG3, or PBS 1 day before infection. Six days after infection, cfu were determined by plating homogenized brain or lung tissue on Sabouraud dextrose agar (8). The cfu are expressed as the mean ± SD.
Serum GXM levels were determined by capture ELISA (31). Before ELISA, serum obtained 6 days after infection was diluted 1:25 with PBS, incubated overnight at 37°C with 0.2 mg/ml proteinase K, and then heated for 20 min at 100°C. Serum GXM concentration was determined relative to GXM standards of known concentration (8).
Statistics.
Data were analyzed with statistical software for Macintosh (instat 2.01; graphpda software for science, San Diego) using the unpaired Student’s t test for organ cfu and serum GXM levels and alternative Weltch t tests for animal survival (9). All results were also analyzed by the unpaired Wilcoxon test, which gave similar results.
RESULTS
Effects of mAbs on Lethal C. neoformans Infection in Immunocompetent Mice.
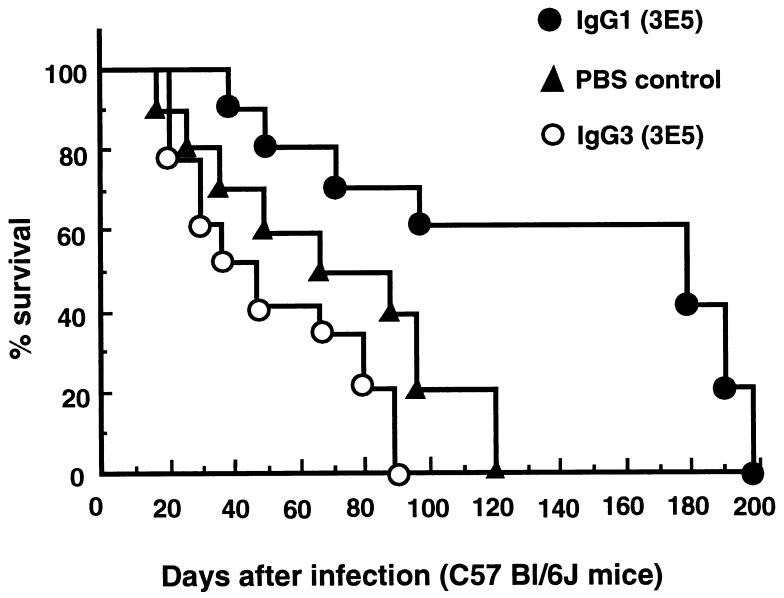
Previous studies on complement-deficient A/J mice showed that the 3E5 IgG3 mAb was not protective against cryptococcal infection (7, 8), whereas its IgG1 switch variant was protective (8). To determine whether these two isotypes have the same effects on immunocompetent complement-sufficient mice, C57BL/6J mice were treated with 3E5 IgG3, 3E5 IgG1, or PBS and then infected. Although there was a trend toward decreased survival for mice given 3E5 IgG3, the results were not significant at P < 0.05 (Fig. 1). However, there was a clear survival benefit for mice given IgG1. Because the 3E5 IgG3 and IgG1 mAbs have the identical antigen binding site (8), this observation underscores the importance of isotype and Fc-mediated functions for antibody efficacy against C. neoformans. It also confirms this effect in the complement-sufficient background strain for most of the genetically immunodeficient mice used in the experiments described below.
Figure 1.
Survival of C57BL/6J mice infected with C. neoformans after administration of mAbs. Average survival times and standard deviations for the IgG1, IgG3, and PBS groups were 131.20 ± 64.68, 50 ± 27.61, and 70.30 ± 38.73 days, respectively. 3E5 IgG1 significantly prolongs survival (P < 0.005), whereas there was no significant reduction in the survival of IgG3-treated mice (P > 0.30).
Effects of mAbs on Lethal C. neoformans Infection in NK Cell-Deficient Beige Mice.
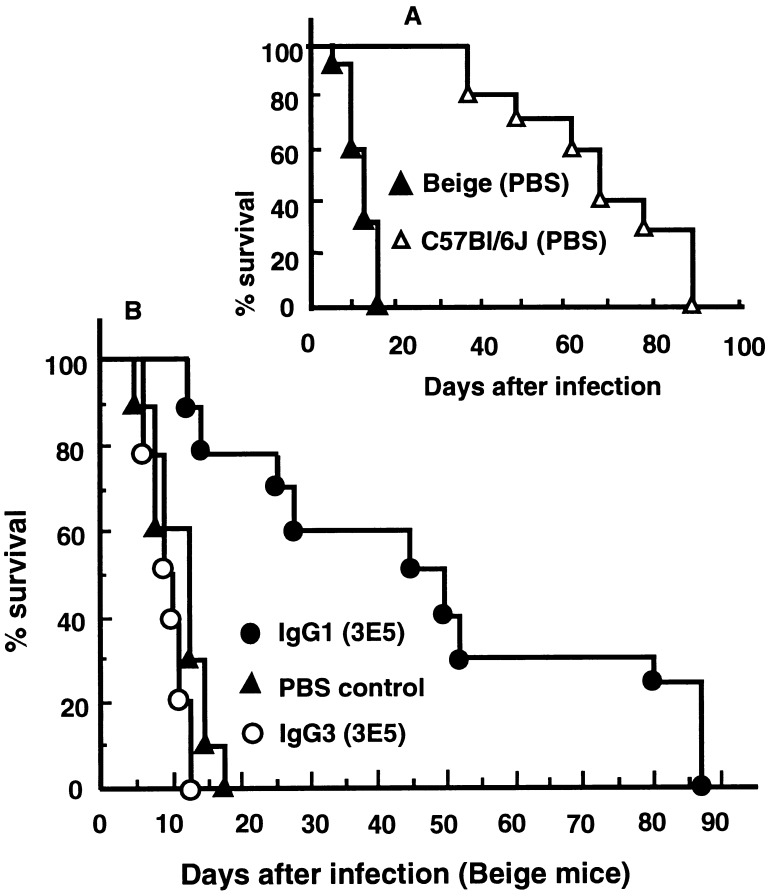
NK cell-deficient beige mice were much more susceptible to cryptococcal infection than the parental C57BL/6J strain (Fig. 2A). Administration of 3E5 IgG1 significantly prolonged animal survival, whereas 3E5 IgG3 did not significantly reduce survival relative to the control (Fig. 2B). Hence, the results of passive antibody experiments in beige mice were similar to those observed with A/J and the C57BL/6J parental strain, suggesting that NK cells are not crucial for the antibody-mediated modulation of cryptococcal infection.
Figure 2.
Survival of NK cell-deficient beige mice infected with C. neoformans after administration of mAbs. (A) Beige mice were more susceptible than the parental C57BL/6J strain (P < 0.0001). (B) Average survival times and standard deviations for the IgG1, IgG3, and PBS groups were 40.40 ± 28.12, 8.00 ± 1.70, and 9.80 ± 2.25 days, respectively. The 3E5 IgG1 mAb significantly prolonged survival (P < 0.001), whereas IgG3 did not alter the course of cryptococcal infection (P > 0.05).
Effects of mAbs on Lethal C. neoformans Infection in SCID Mice.
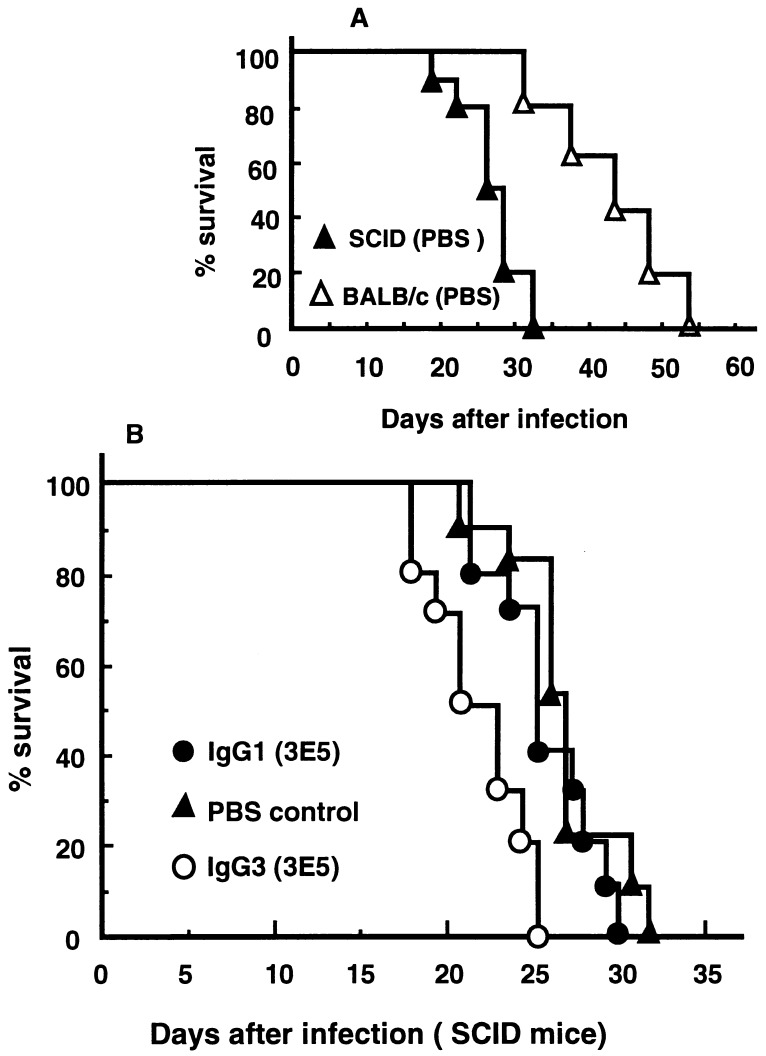
T cells are important in the resistance of immunocompetent individuals and animals to C. neoformans (16, 32, 33). SCID mice that lack antigen receptor genes and do not have mature T and B cells (27) are more susceptible to cryptococcal infection than immunocompetent BALB/c mice, the parental strain of SCID mice (Fig. 3A). Consistent with the C57BL/6J experiment described above, survival times of immunocompetent BALB/c mice treated with 3E5 IgG3, PBS, and 3E5 IgG1 were 32.4 ± 5.4, 46.7 ± 8.5, and 94.2 ± 15.7 days, respectively. Thus, in BALB/c mice, 3E5 IgG3 also produced a trend toward reduced survival that did not achieve significance at the P < 0.05 level, whereas its IgG1 switch variant significantly prolonged survival (P < 0.003). In contrast, in SCID mice, 3E5 IgG1 was no longer protective against C. neoformans (Fig. 3B), whereas the administration of IgG3 reduced survival relative to the control (P < 0.001, Fig. 3B).
Figure 3.
Survival of SCID mice infected with C. neoformans after the administration of mAbs. (A) SCID mice were more susceptible than the parental BALB/c strain (P < 0.001). (B) Average survival times and standard deviations for the IgG1-, IgG3-, and PBS-treated groups were 25.40 ± 2.50, 21.10 ± 2.47, and 26.80 ± 2.70 days, respectively. The 3E5 IgG1 mAb failed to protect SCID mice (P > 0.25), whereas the IgG3 mAb decreased survival (P < 0.001).
CD4+ T Cells Are Required for IgG1-Mediated Protection.
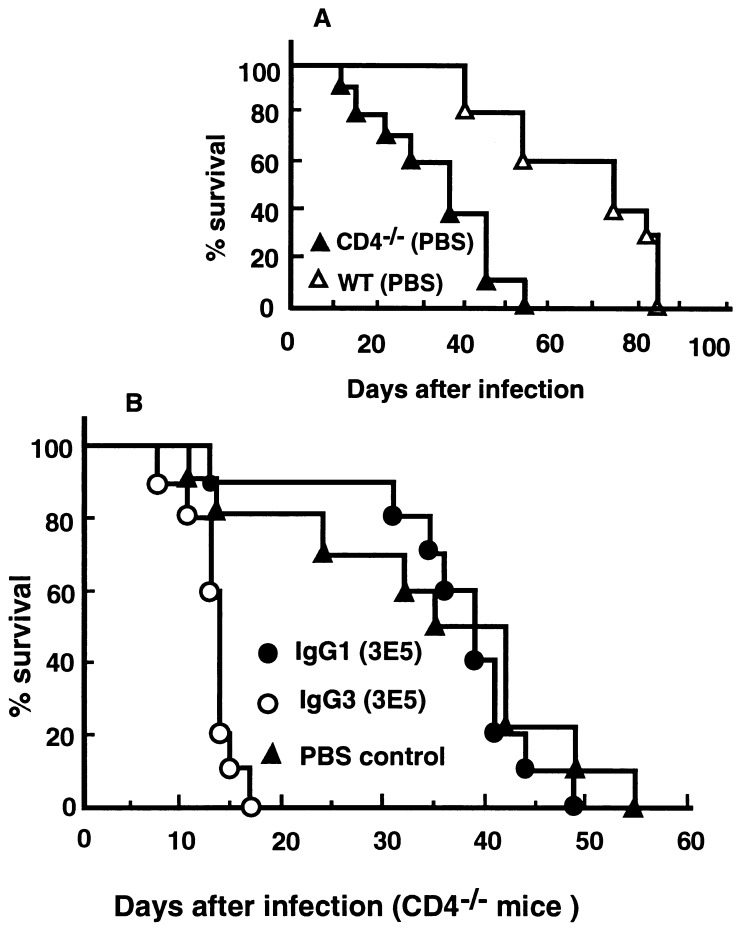
Antibody depletion studies have shown that CD4+ T cells play an important role in the inflammatory response to C. neoformans and help control the dissemination of the organism in immunocompetent mice (19, 20, 32). Fig. 4A shows that CD4−/− C57BL/6J mice are more susceptible to cryptococcal infection than the parental strain. Administration of 3E5 IgG1 to CD4−/− mice did not prolong survival relative to PBS-treated controls (Fig. 4B), indicating that CD4+ T cells are required for the IgG1-mediated protection of the immunocompetent parental strain (Fig. 1). In contrast to the lack of protection or enhancement of infection by 3E5 IgG3 in the immunocompetent C57BL/6J mice (Fig. 1), the survival of CD4−/− mice treated with IgG3 was decreased compared with the PBS control (Fig. 4B).
Figure 4.
Survival of CD4−/− mice infected with C. neoformans after administration of mAb. (A) CD4−/− mice were more susceptible than the C57BL/6J parental strain (P < 0.002). (B) Average survival times and standard deviations for the IgG1-, IgG3-, and PBS-treated groups were 38.30 ± 10.54, 13.30 ± 2.41, and 31.30 ± 14.35 days, respectively. 3E5 IgG1 failed to protect CD4−/− mice (P > 0.23), whereas IgG3 administration decreased animal survival (P < 0.007). Although the difference between the average survival of the IgG3- and PBS-treated animals is quite large, the large SD in the PBS control group makes it impossible to determine whether the enhancement in the CD4−/− mice is significantly greater than that in the SCID mice.
The results of the survival studies in CD4−/− mice were supported by determining cfu and the serum GXM level 6 days after infection. Table 1 shows that brain cfu and serum GXM levels in 3E5 IgG1-treated CD4−/− mice were nearly identical to mice treated with PBS, although there was a small increase in lung cfu in IgG1-treated mice. In contrast, mice treated with 3E5 IgG3 had many more organisms in their lungs and a smaller, although statistically significant, increase in cfu in the brain compared with PBS-treated controls or IgG1-treated mice (Table 1). The IgG3-treated mice also had higher levels of circulating GXM, a result consistent with a greater fungal load. These results indicate CD4+ T cells are required for IgG1-mediated protection but not for the enhancing effects of the IgG3 antibody.
Table 1.
Organ cfu and serum GXM in CD4−/− mice 6 days after cryptococcal infection
| Lung cfu, × 105 | P ≤ | Brain cfu, × 105 | P ≤ | GXM*, mg/ml | P ≤ | |
|---|---|---|---|---|---|---|
| No IFN-γ therapy | ||||||
| PBS | 12.2 ± 0.9 | 0.0220† | 26.0 ± 1.6 | 0.507† | 1.4 ± 0.1 | 0.109† |
| IgG1 | 20.7 ± 2.6 | 0.0001‡ | 25.0 ± 2.7 | 0.001‡ | 1.5 ± 0.1 | 0.0001‡ |
| IgG3 | 111.8 ± 14.1 | 0.0001§ | 34.2 ± 2.6 | 0.001§ | 2.5 ± 0.3 | 0.0001§ |
| IFN-γ therapy | ||||||
| PBS | 11.5 ± 1.8 | 0.012† | 12.8 ± 2.6 | 0.001† | 1.2 ± 0.2 | 0.0005† |
| IgG1 | 8.0 ± 0.9 | 0.0002‡ | 5.4 ± 1.8 | 0.0001‡ | 0.5 ± 0.2 | 0.0001‡ |
| IgG3 | 33.6 ± 4.3 | 0.0001§ | 29.4 ± 3.7 | 0.0001§ | 2.3 ± 0.3 | 0.0003§ |
Value is expressed as mean ± SD.
PBS vs. IgG1.
IgG1 vs. IgG3.
IgG3 vs. PBS (unpaired Student’s t test).
IFN-γ Is Required for IgG1-Mediated Protection.
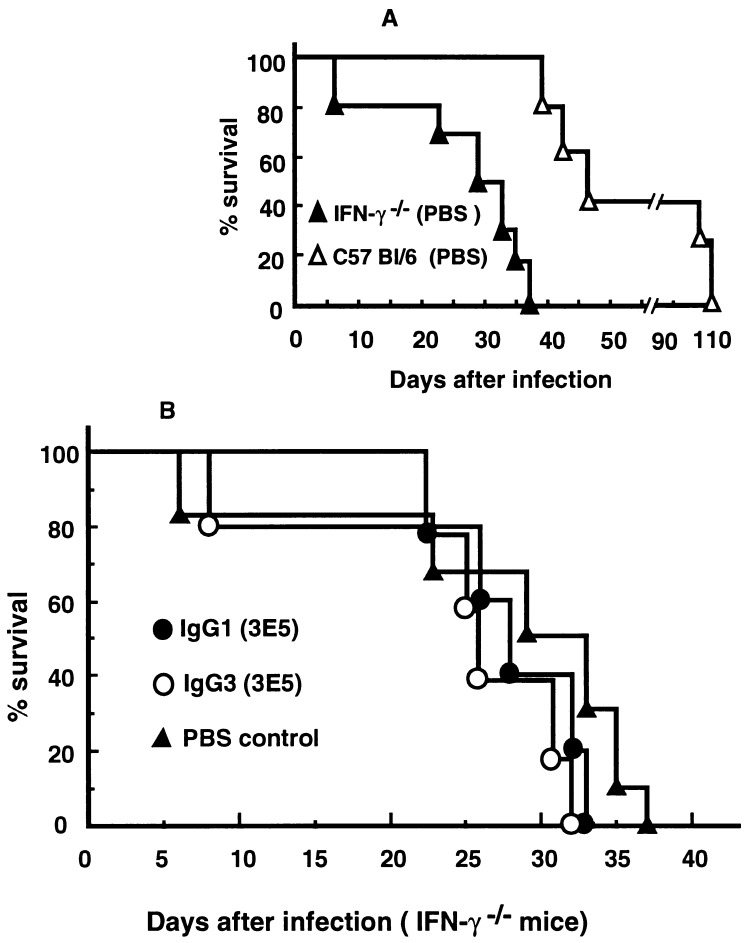
Given that IFN-γ stimulates the phagocytic and fungicidal activity of effector cells such as macrophages (21, 34) and that IFN-γ is produced by CD4+ cells (35), we examined whether IFN-γ was involved in the modulation of antibody efficacy by CD4+ T cells. Fig. 5A shows that IFN-γ−/− mice (29) challenged with C. neoformans had decreased survival times compared with the parental strain. 3E5 IgG1 did not prolong survival in IFN-γ-deficient mice (Fig. 5B), indicating that IFN-γ is required for the IgG1-mediated protection. In addition, IFN-γ-deficient animals treated with IgG3 did not manifest the shorter survival seen in CD4−/− mice (Fig. 5B), demonstrating that IFN-γ is also involved in the IgG3-mediated enhancement of infection.
Figure 5.
Survival of IFN-γ knockout mice infected with C. neoformans after the administration of mAb. (A) IFN-γ−/− mice were more susceptible than their parental C57BL/6J strain (P < 0.02). (B) Average survival times and standard deviations for the IgG1, IgG3, and PBS groups were 28.20 ± 4.24, 24.40 ± 9.11, and 25.80 ± 11.58 days, respectively. IFN-γ−/− mice were not protected by 3E5 IgG1 (P > 0.1), and IgG3 did not enhance infection (P > 0.1).
Groups of five mice were injected with IFN-γ and given either mAb or PBS 1 day before infection with C. neoformans. Six days later, lung and brain cfu levels were determined. Consistent with previous reports on immunocompetent mice (21), administration of IFN-γ to CD4−/− mice reduced the organ fungal burden (Table 1, compare PBS controls for brain with and without IFN-γ therapy). CD4−/− mice treated with IFN-γ and 3E5 IgG1 showed an even greater decrease in fungal load both in brain and lungs, as well as decreased levels of serum GXM (Table 1). In contrast, a single injection of IFN-γ resulted in an increase in cfu in the lungs and brain of IgG3-treated CD4−/− animals, confirming that IFN-γ also plays a significant role in the augmented fungal dissemination mediated by IgG3.
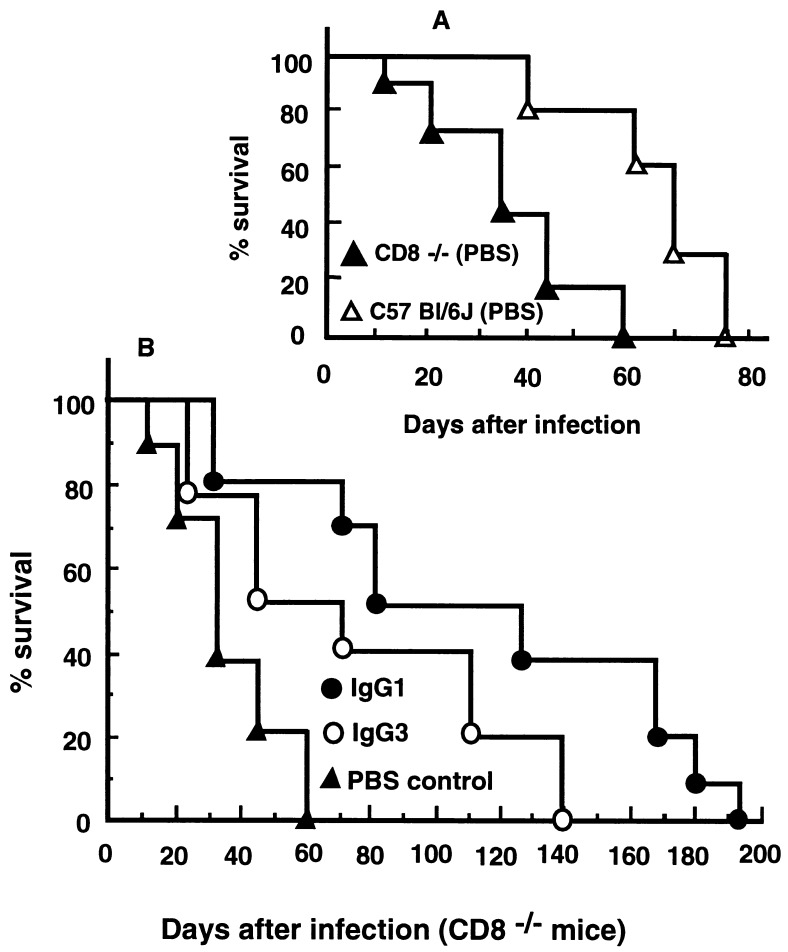
CD8+ T Cells Are Required for IgG3-Mediated Reduction in Survival.
CD8+ T cells contribute to the natural resistance of mice to cryptococcal infection, although their role is less clear than that of CD4+ cells (32, 36–39). The survival time of CD8−/− mice infected with C. neoformans was significantly decreased relative to that of the parental C57BL/6J strain (Fig. 6A). Administration of 3E5 IgG1 to CD8−/− mice significantly prolonged animal survival (P < 0.001) compared with PBS-treated controls (Fig. 6B). In contrast to the effect of IgG3 in CD4−/− mice (where it reduced survival), 3E5 IgG3 was protective in CD8−/− mice and prolonged animal survival significantly (P < 0.03) compared with PBS controls (Fig. 6B). This experiment was repeated three times to ensure that this observation was reproducible, and similar results were also obtained with β2-microglobulin knockout (impaired CD8+ T cell function) mice (data not shown). These results strongly suggest that IgG3-mediated enhancement of cryptococcal infection requires CD8+ T cells.
Figure 6.
Survival of CD8−/− mice infected with C. neoformans after administration of mAbs. (A) CD8−/− mice were more susceptible than their parental C57BL/6J strain (P < 0.003). (B) Average survival times and standard deviations for the IgG1, IgG3, and PBS groups were 114.30 ± 59.60, 76.90 ± 44.67, and 35.30 ± 16.13 days, respectively. Both IgG1 (P < 0.001) and IgG3 (P < 0.03) mAbs significantly prolong animal survival.
DISCUSSION
We have administered the nonprotective 3E5 IgG3 and the protective 3E5 IgG1 mAbs to immunodeficient mice infected with C. neoformans to identify the cell types and immunological functions that are responsible for their respective properties and to determine whether passive antibody would be useful in preventing or treating cryptococcal infections in immunodeficient individuals. These studies resulted in four major findings. First, NK cells do not appear to be important for the antibody-mediated modulation of cryptococcal infection. Second, CD4+ T cells are required for antibody-mediated protection against cryptococcal infection, and this protective effect requires IFN-γ. Third, IgG3 enhances the dissemination of the organism in the absence of CD4+ T cells, and this effect is also mediated through IFN-γ. Fourth, IgG3 is protective against cryptococcal infection when CD8+ T cells are defective, implicating CD8+ T cells in the IgG3-mediated enhancement of infection observed in several mouse strains.
Deficiencies in NK cells, T cells, and IFN-γ have been shown by others to lead to an increased susceptibility to infection with C. neoformans (16–18, 32, 33). Because we were already administering anti-cryptococcal antibodies, we chose to use mice with inherited immunological defects rather than mice made immunodeficient by antibody-mediated depletion of T cells, NK cells, and IFN-γ. Although each of the genetically defective mouse strains has a particular primary defect introduced by the genetic disruption, these mice are also abnormal in many other traits that depend on the defective cell or lymphokine. This is also true of patients who have acquired or inherited defects, including patients with AIDS who are deficient in CD4+ T cells and have abnormal CD4/CD8 ratios. Nevertheless, our results are consistent with prior studies and confirm the important roles for CD4+ and CD8+ T cells and IFN-γ in host defenses against C. neoformans.
T cells have been reported to have widely different effects on cryptococcal infection (16, 20, 36, 38, 39). A complex combination of non-antibody-dependent and antibody-activated direct and indirect effects could be responsible for the different outcomes with the IgG3 and IgG1 mAbs. Nevertheless, the inability of IgG1 to confer protection in the SCID, CD4−/−, and IFN-γ-deficient mice, and the restitution of IgG1-mediated protection when IFN-γ was administered to the CD4−/− mice, focuses attention on Th1 T cells and their role in activating macrophages and other effector cells. Other cytokines such as interleukins 2, 10, 12, and 13; transforming growth factor β; and granulocyte/macrophage colony-stimulating factor play important roles in regulating the activation of immune effector cells in cryptococcal infection (40–42). Nevertheless, IFN-γ alone administered at the beginning of the infection was sufficient to produce antibody-mediated protection in this model of infection. The loss of CD4+-mediated activation of phagocytic cells through the release of IFN-γ could explain why the IgG1 mAb was not effective against cryptococcal infection in SCID, CD4−/−, and IFN-γ-deficient mice.
The fact that both IgG1 and IgG3 antibodies are protective and prolong survival significantly in mice lacking CD8+ T cells was surprising. CD8+ T cells are heterogeneous in function and could potentially impair (38, 39) or enhance host defense against C. neoformans (32, 36). The development and activation of T cells with suppressive activity could down-regulate the Th1 response either directly or indirectly. The protective efficacy of IgG3 revealed in the CD8−/− mice may be overshadowed in the immunocompetent mice by the activation of the CD8+ cell population. In the absence of CD4+ cells, it is not clear what the target of the CD8+ cells would be, but IgG3 may be acting through effector cells different from those used by IgG1. These studies reveal the importance of the ratio of CD4/CD8 cells in mediating the effects of antibody.
Superimposed on this complexity is the question of why IgG3 and IgG1 mediate such different effects. Our findings are not restricted to the 3E5 isotype switch variant set because other IgG3 antibodies also accelerate infection, whereas none of the IgG1, IgG2a, or IgG2b mAbs do so (6, 9). The receptor for mouse IgG3 differs functionally from the other Fc receptors on macrophages (13–15), but it has not been characterized at the molecular level, and its distribution is not known (43). It is possible that IgG3–Fc receptor-mediated opsonization does not activate effector cells to arrest growth of the organism, thus protecting the organism from other fungistatic or fungicidal effectors and allowing continued replication and dissemination. IFN-γ can increase Fc receptor expression on effector cells and, in the case of the γ3 receptor, could promote more effective phagocytic and fungal protective activity (ref. 21 and unpublished data).
The findings reported here reveal a functional dependence of passive antibody on T cell function in mice infected with C. neoformans. If similar phenomena occur in humans, these findings have important implications for the pathogenesis of human infections and for the development of antibody-based therapies in patients with AIDS. Patients with AIDS have serum antibodies to the cryptococcal polysaccharide (44, 45). In the setting of HIV-associated CD4+ depletion, it is conceivable that some antibodies lose their protective efficacy, whereas others retain or acquire the capacity to enhance infection. Only a minority of AIDS patients with low CD4 counts develop cryptococcal infections despite a high likelihood of frequent exposure to the fungus. Susceptibility to infection may reflect the quantity and quality of the antibody in the circulation in the setting of abnormal CD4/CD8 ratios. Furthermore, our findings suggest that if antibody is to be used for the prevention and treatment of cryptococcal infection in patients with defective CD4+ T cell function, adjunctive therapy with IFN-γ may be necessary.
In addition to their implications for specific therapies, the findings reported here reveal that individual antibodies have very different inherent properties that may be difficult to deduce from their structural characteristics or even their in vitro functions. However, the actual impact of the antibodies in vivo will be determined by the effector cells with which they interact and the state of those effector cells in the host.
Acknowledgments
We thank Drs. B. Diamond, L.-A. Pirofski, B. R. Bloom, and D. Beenhouwer for their comments on the manuscript. We also thank Drs. Tak Mak and Barry Bloom for making various immunodeficient mice available to us. R.R.Y. is supported by a fellowship from the Aaron Diamond Foundation, A.C. is supported by National Institutes of Health Grants AI-33142 and AI-33774 and a Burroughs Wellcome Development Therapeutics Award, and M.D.S. is supported by the Harry Eagle Chair provided by the Women’s Division of the Albert Einstein College of Medicine and by National Institutes of Health Grant R35 CA-39838.
ABBREVIATIONS
- GXM
glucuronoxylomannan
- IFN-γ
interferon γ
- NK
natural killer
- cfu
colony-forming unit(s)
References
- 1.Zuger A, Louie E, Holzman R S, Simberkoff M S, Rahal J J. Ann Intern Med. 1986;104:234–240. doi: 10.7326/0003-4819-104-2-234. [DOI] [PubMed] [Google Scholar]
- 2.Dromer F, Charreire J. J Infect Dis. 1991;163:1114–1120. doi: 10.1093/infdis/163.5.1114. [DOI] [PubMed] [Google Scholar]
- 3.Spitzer E D, Spitzer S G, Freundlich L F, Casadevall A. Lancet. 1993;341:595–596. doi: 10.1016/0140-6736(93)90354-j. [DOI] [PubMed] [Google Scholar]
- 4.Zuger A, Louie E, Holzman R S, Simberkoff M S, Rahal J J. Ann Intern Med. 1986;104:234–240. doi: 10.7326/0003-4819-104-2-234. [DOI] [PubMed] [Google Scholar]
- 5.Casadevall A. Infect Immun. 1995;63:4211–4218. doi: 10.1128/iai.63.11.4211-4218.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mukherjee J, Scharff M D, Casadevall A. Infect Immun. 1992;60:4534–4541. doi: 10.1128/iai.60.11.4534-4541.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mukherjee J, Nussbaum G, Scharff M D, Casadevall A. J Exp Med. 1995;181:405–409. doi: 10.1084/jem.181.1.405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yuan R, Casadevall A, Spira G, Scharff M D. J Immunol. 1995;154:1810–1816. [PubMed] [Google Scholar]
- 9.Nussbaum G, Yuan R, Casadevall A, Scharff M D. J Exp Med. 1996;183:1905–1909. doi: 10.1084/jem.183.4.1905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Briles D E, Claflin J L, Schroer K, Forman C. Nature (London) 1981;294:88–90. doi: 10.1038/294088a0. [DOI] [PubMed] [Google Scholar]
- 11.Greenspan N S, Dacek D A, Cooper L J. J Immunol. 1988;141:4276–4282. [PubMed] [Google Scholar]
- 12.Pollock R R, French D L, Metlay J P, Birshtein B K, Scharff M D. Eur J Immunol. 1990;20:2021–2027. doi: 10.1002/eji.1830200921. [DOI] [PubMed] [Google Scholar]
- 13.Diamond B, Yelton D E. J Exp Med. 1981;153:514–519. doi: 10.1084/jem.153.3.514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Grey H M, Hirst J W, Cohn M. J Exp Med. 1971;133:289–304. doi: 10.1084/jem.133.2.289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ralph P, Nakoinz I. J Immunol. 1983;131:1028–1031. [PubMed] [Google Scholar]
- 16.Huffnagle G B, Yates J L, Lipscomb M F. Infect Immun. 1991;59:1423–1433. doi: 10.1128/iai.59.4.1423-1433.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Marquis G, Montplaisir S, Pelletier M, Mousseau S, Auger P. Infect Immun. 1985;47:288–293. doi: 10.1128/iai.47.1.288-293.1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hidore M R, Murphy J W. J Immunol. 1986;137:3624–3631. [PubMed] [Google Scholar]
- 19.Hill J O. J Exp Med. 1992;175:1685–1695. doi: 10.1084/jem.175.6.1685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hill J O, Aguirre K M. J Immunol. 1994;152:2344–2350. [PubMed] [Google Scholar]
- 21.Kawakami K, Kohno S, Kadota J, Tohyama M, Teruya K, Kudeken N, Saito A, Hara K. Microbiol Immunol. 1995;39:135–143. doi: 10.1111/j.1348-0421.1995.tb02180.x. [DOI] [PubMed] [Google Scholar]
- 22.Devi S J, Schneerson R, Egan W, Ulrich T J, Bryla D, Robbins J B, Bennett J E. Infect Immun. 1991;59:3700–3707. doi: 10.1128/iai.59.10.3700-3707.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Spira G, Scharff M D. J Immunol Methods. 1992;148:121–129. doi: 10.1016/0022-1759(92)90165-p. [DOI] [PubMed] [Google Scholar]
- 24.Koller B H, Marrack P, Kappler J W, Smithies O. Science. 1990;248:1227–1230. doi: 10.1126/science.2112266. [DOI] [PubMed] [Google Scholar]
- 25.Rhoder J C. J Immunol. 1979;123:2168–2173. [PubMed] [Google Scholar]
- 26.Rhoder J C, Lohman-Mathese M, Domzig W, Wigzell H. J Immunol. 1979;123:2174–2181. [PubMed] [Google Scholar]
- 27.Bosma G, Custer R P, Bosma M J. Nature (London) 1983;301:527–530. doi: 10.1038/301527a0. [DOI] [PubMed] [Google Scholar]
- 28.Grusby M J, Johnson R S, Papaioannou V E, Glimcher L H. Science. 1991;253:1417–1420. doi: 10.1126/science.1910207. [DOI] [PubMed] [Google Scholar]
- 29.Dalton D K, Pitts-Meek S, Keshav S, Figari I S, Bradley A, Stewart T A. Science. 1993;259:1739–1742. doi: 10.1126/science.8456300. [DOI] [PubMed] [Google Scholar]
- 30.Fung-Leung W P, Schilham M W, Rahemtulla A, Kundig T M, Vollenweider M, Potter J, van Ewijk W, Mak T W. Cell. 1991;65:443–449. doi: 10.1016/0092-8674(91)90462-8. [DOI] [PubMed] [Google Scholar]
- 31.Casadevall A, Scharff M D. J Exp Med. 1991;174:151–160. doi: 10.1084/jem.174.1.151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Huffnagle G B, Lipscomb M F, Lovchik J A, Hoag K A, Street N E. J Leukocyte Biol. 1994;55:35–42. doi: 10.1002/jlb.55.1.35. [DOI] [PubMed] [Google Scholar]
- 33.Levitz S M, North E A, Dupont M P, Harrison T S. Infect Immun. 1995;63:3550–3554. doi: 10.1128/iai.63.9.3550-3554.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mody C H, Tyler C L, Sitrin R G, Jackson C, Toews G B. Am J Respir Cell Mol Biol. 1991;5:19–26. doi: 10.1165/ajrcmb/5.1.19. [DOI] [PubMed] [Google Scholar]
- 35.Mosmann T R, Coffman R L. Annu Rev Immunol. 1989;7:145–173. doi: 10.1146/annurev.iy.07.040189.001045. [DOI] [PubMed] [Google Scholar]
- 36.Mody C H, Paine R R, Jackson C, Chen G H, Toews G B. J Immunol. 1994;152:3970–3979. [PubMed] [Google Scholar]
- 37.Mody C H, Chen G H, Jackson C, Curtis J L, Toews G B. Mycopathologia. 1994;125:7–17. doi: 10.1007/BF01103969. [DOI] [PubMed] [Google Scholar]
- 38.Khakpour F R, Murphy J W. Infect Immun. 1987;55:1657–1662. doi: 10.1128/iai.55.7.1657-1662.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Fidel P L, Murphy J W. Infect Immun. 1988;56:1267–1272. doi: 10.1128/iai.56.5.1267-1272.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Levitz S M, Dupont M P. J Clin Invest. 1993;91:1490–1498. doi: 10.1172/JCI116354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Chen G H, Curtis J L, Mody C H, Christensen P J, Armstrong L R, Toews G B. J Immunol. 1994;152:724–734. [PubMed] [Google Scholar]
- 42.Skeen M J, Miller M A, Shinnick T M, Ziegler H K. J Immunol. 1996;156:1196–1206. [PubMed] [Google Scholar]
- 43.Ravetch J V. Cell. 1994;78:553–560. doi: 10.1016/0092-8674(94)90521-5. [DOI] [PubMed] [Google Scholar]
- 44.Deshaw M, Pirofski L A. Clin Exp Immunol. 1995;99:425–432. doi: 10.1111/j.1365-2249.1995.tb05568.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Houpt D C, Pfrommer G S, Young B J, Larson T A, Kozel T R. Infect Immun. 1994;62:2857–2864. doi: 10.1128/iai.62.7.2857-2864.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]