Abstract
MIC methodology was used to test the antibacterial activity of XRP 2868, a new oral combination of two semisynthetic streptogramins, RPR 132552A and RPR 202868, compared to activities of other antibacterial agents against pneumococci, Haemophilus influenzae, and Haemophilus parainfluenzae. For 261 pneumococci, XRP 2868 and pristinamycin MICs were similar, irrespective of penicillin G and erythromycin A susceptibilities (MIC at which 50% of isolates were inhibited [MIC50], 0.25 μg/ml; MIC90, 0.5 μg/ml), while quinupristin/dalfopristin had MICs which were 1 to 2 dilutions higher. Single components of both XRP 2868 and quinupristin/dalfopristin had higher MICs. Erythromycin A, azithromycin, clarithromycin, and clindamycin MICs were higher for penicillin G-intermediate and -resistant than -susceptible pneumococci. Against 150 H. influenzae strains, all compounds tested had unimodal MIC distributions. XRP 2868 had an overall MIC50 of 0.25 μg/ml and an MIC90 of 1.0 μg/ml, with no differences between β-lactamase-positive, β-lactamase-negative, and β-lactamase-negative ampicillin-resistant strains. Of note was the similarly low activity of one of its components, RPR 132552A. Pristinamycin and quinupristin/dalfopristin had MICs of 0.125 to 8.0 μg/ml; quinupristin alone had MICs of 8.0 to >64.0 μg/ml, and dalfopristin had MICs of 1.0 to >64.0 μg/ml. Erythromycin A, azithromycin, and clarithromycin had modal MICs of 4.0, 1.0, and 8.0 μg/ml, respectively. MICs of all compounds against H. parainfluenzae were 1 to 2 dilutions higher than against H. influenzae. XRP 2868 showed potent activity against pneumococci and Haemophilus strains irrespective of their susceptibility to other agents.
The major bacterial pathogens responsible for community-acquired respiratory tract infections comprise Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis (6, 7, 9-11, 24). Pneumococcal resistance to penicillin G and other β-lactam and non-β-lactam compounds has increased worldwide at an alarming rate, including in the United States. Major foci of resistance prevalence currently include South Africa, Spain, Japan, Hong Kong, Korea, and Central and Eastern Europe (2, 4, 10, 11). In the United States, a recent survey (4) showed an increase in penicillin G nonsusceptibility from <5% before 1989 (including <0.02% of isolates for which MICs were ≥2.0 μg/ml) to 6.6% in 1991 to 1992 (for 1.3% of isolates, MICs were ≥2.0 μg/ml). In another, more recent survey, 50.4% of 1,476 clinically significant pneumococcal isolates were not susceptible to penicillin G (11). Previous studies have shown that parenteral quinupristin/dalfopristin and oral pristinamycin (available in France) are very potent against pneumococci, irrespective of their β-lactam and erythromycin A susceptibilities (8, 12, 15, 19, 21). It is also important to note the high rates of isolation of penicillin G-intermediate and -resistant pneumococci (approximately 30%) in middle ear fluids from patients with refractory otitis media, compared to other isolation sites (3). The problem of drug-resistant pneumococci is compounded by the ability of resistant clones to spread from country to country and from continent to continent (2, 10, 16).
Although H. influenzae remains a major cause of respiratory tract infections (24), Haemophilus parainfluenzae may also play a role, especially in acute exacerbations of chronic bronchitis (20). The major resistance mechanism of these species is β-lactamase (TEM-1 or ROB-1) production, the prevalence of which is approximately 40% in the United States (11). The incidence of β-lactamase-negative ampicillin-resistant (BLNAR) strains is currently <1% in the United States (11) but is significantly higher in Japan (23). Among members of the macrolide and azalide groups, azithromycin has the lowest MICs against these organisms, followed by ketolides such as telithromycin, erythromycin A, and clarithromycin (1, 5, 6, 10, 14, 17). Of available streptogramins, oral pristinamycin and parenteral quinupristin/dalfopristin have MICs for H. influenzae and H. parainfluenzae which are several dilutions higher than those for pneumococci (8, 12, 15). The exact therapeutic role of the macrolide-azalide group in therapy of H. influenzae infections is unclear (11), and pristinamycins have not been used for this purpose.
There is an urgent need for oral compounds for outpatient treatment of otitis media and other respiratory tract infections caused by penicillin G-intermediate and -resistant pneumococci (7) as well as H. influenzae. Available groups include β-lactams, macrolides, and quinolones. Oral pristinamycin is not available in the United States, and quinupristin/dalfopristin can be administered only parenterally.
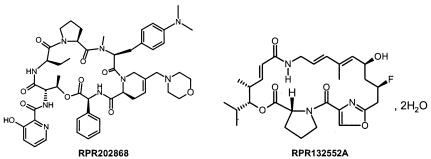
XPR 2868 is a new investigational oral streptogramin, being a 70/30 ratio of RPR 132552A and RPR 20868 (Fig. 1). The present study tested (i) the activities of XPR 2868, RPR 132552A, RPR 20868, pristinamycin, quinupristin/dalfopristin, quinupristin, dalfopristin, erythromycin A, azithromycin, clarithromycin, and clindamycin against 261 pneumococci by agar dilution MIC testing and (ii) the activities of all of the latter compounds except clindamycin against 150 H. influenzae and 26 H. parainfluenzae strains by microdilution MIC testing. This is the first journal publication on this compound of which we are aware.
FIG. 1.
Structures of the components of XRP 2868. XRP 2868 consists of a 30/70 combination of RPR 202868 (a pristinamycin IA derivative) and RPR 132552A (a pristinamycin IIB derivative).
MATERIALS AND METHODS
Bacteria.
Pneumococci comprised 86 penicillin G-susceptible (MICs, ≤0.06 μg/ml), 81 penicillin G-intermediate (MICs, 0.125 to 1.0 μg/ml), and 94 penicillin G-resistant (MICs, 2.0 to 16.0 μg/ml) strains. Of these, 120 were erythromycin resistant (MICs, ≥1.0 μg/ml); 65 had erm(B), 32 had mef(A), 1 had erm(B) and mef(A), 19 had mutations in L4, and 3 had mutations in 23S rRNA (A2059G). These macrolide-resistant strains were relatively recent clinical isolates (1998 to 2002) with previously defined phenotypes and genotypes from our collection.
One hundred fifty H. influenzae and 26 H. parainfluenzae strains were tested. H. influenzae strains comprised 146 recent untypeable isolates and 4 type b strains from our collection. β-Lactamase testing was performed by the Cefinase (BBL Microbiology systems, Cockeysville, Md.) disk method.
Antibacterials and MIC testing.
All drug substances were obtained from Aventis Pharma, Romainville, France. The agar dilution method, as used in our laboratory for many years (10, 11, 13, 17, 21, 22), was performed for pneumococci by using Mueller-Hinton agar (BBL Microbiology Systems, Cockeysville, Md.) supplemented with 5% sheep blood. Standard quality control strains, including S. pneumoniae ATCC 49619 (18), were included in each run of agar dilution MICs. Plates were incubated in air for 20 to 24 h.
For Haemophilus strains, MICs were determined by the NCCLS microdilution method (18) using commercially prepared frozen panels (TREK, Inc., Cleveland, Ohio) using freshly prepared Haemophilus test medium. Inocula were prepared from chocolate agar plates incubated a full 24 h by the direct colony suspension method as recommended by the NCCLS. Standard quality controls were used on each day of testing. Inoculum checks were also performed, and only trays yielding 3 × 105 to 7 × 105 CFU/ml were used. Trays were covered and incubated overnight at 35°C in ambient air (11).
RESULTS
Results of agar dilution MICs with pneumococcal strains classified by penicillin G susceptibility are summarized in Table 1, and results for strains classified by erythromycin A susceptibility are found in Table 2. XRP 2868, pristinamycin, and quinupristin/dalfopristin had low MICs irrespective of the strain's penicillin G or erythromycin A susceptibility status, with MICs ranging from 0.06 to 1.0 μg/ml (XRP 2868), 0.125 to 1.0 (pristinamycin), and ≤0.06 to 1.0 (quinupristin/dalfopristin) μg/ml. The two components of XRP 2868 and quinupristin/dalfopristin were without significant activity. Streptogramin MICs for macrolide-resistant strains were not influenced by erythromycin A resistance mechanisms. Macrolide MICs for ribosomal mutants were higher than those for the wild type, as published previously (13). However, streptogramin MICs were uninfluenced by macrolide susceptibility status or resistance mechanisms.
TABLE 1.
Agar dilution MICs for 261 pneumococcal strains classified by penicillin susceptibility
| Drug and strain category (n)a | MIC (μg/ml)
|
||
|---|---|---|---|
| Range | 50% | 90% | |
| Penicillin G | |||
| Penicillin S (86) | 0.016-0.06 | 0.03 | 0.03 |
| Penicillin I (81) | 0.125-1.0 | 0.25 | 1.0 |
| Penicillin R (94) | 2.0-16.0 | 2.0 | 4.0 |
| XPR 2868 | |||
| Penicillin S | 0.06-0.25 | 0.125 | 0.25 |
| Penicillin I | 0.06-0.5 | 0.25 | 0.25 |
| Penicillin R | 0.06-1.0 | 0.25 | 0.5 |
| RPR 132552 | |||
| Penicillin S | <0.5-16.0 | 4.0 | 8.0 |
| Penicillin I | ≤0.5-64.0 | 4.0 | 8.0 |
| Penicillin R | ≤0.5->64.0 | 4.0 | 32.0 |
| RPR 202868 | |||
| Penicillin S | ≤0.5->64.0 | 4.0 | 16.0 |
| Penicillin I | 1.0->64.0 | 8.0 | 32.0 |
| Penicillin R | 1.0->64.0 | 16.0 | 64.0 |
| Pristinamycin | |||
| Penicillin S | 0.125-0.5 | 0.25 | 0.25 |
| Penicillin I | 0.125-1.0 | 0.25 | 0.5 |
| Penicillin R | 0.125-1.0 | 0.25 | 0.5 |
| Quinupristin/dalfopristin | |||
| Penicillin S | ≤0.06-1.0 | 0.5 | 0.5 |
| Penicillin I | 0.125-1.0 | 0.5 | 1.0 |
| Penicillin R | 0.125-1.0 | 0.5 | 1.0 |
| Quinupristin | |||
| Penicillin S | ≤0.5-64.0 | 2.0 | 4.0 |
| Penicillin I | ≤0.5->64.0 | 4.0 | 32.0 |
| Penicillin R | ≤0.5->64.0 | 4.0 | 32.0 |
| Dalfopristin | |||
| Penicillin S | 8.0->64.0 | 64.0 | >64.0 |
| Penicillin I | 8.0->64.0 | 64.0 | >64.0 |
| Penicillin R | 16.0->64.0 | >64.0 | >64.0 |
| Erythromycin A | |||
| Penicillin S | 0.016->64.0 | 0.125 | 32.0 |
| Penicillin I | 0.03->64.0 | 0.125 | >64.0 |
| Penicillin R | 0.03->64.0 | >64.0 | >64.0 |
| Azithromycin | |||
| Penicillin S | 0.03->64.0 | 0.125 | 16.0 |
| Penicillin I | 0.06->64.0 | 0.125 | >64.0 |
| Penicillin R | 0.06->64.0 | >64.0 | >64.0 |
| Clarithromycin | |||
| Penicillin S | ≤0.008->64.0 | 0.03 | 8.0 |
| Penicillin I | 0.016->64.0 | 0.06 | >64.0 |
| Penicillin R | ≤0.008->64.0 | 32.0 | >64.0 |
| Clindamycin | |||
| Penicillin S | ≤0.008->64.0 | 0.06 | 0.06 |
| Penicillin I | 0.016->64.0 | 0.06 | >64.0 |
| Penicillin R | 0.016->64.0 | 0.06 | >64.0 |
S, susceptible; I, intermediate; R, resistant.
TABLE 2.
Agar dilution MICs for 261 pneumococcal strains classified by erythromycin A susceptibility
| Drug and strain category (n)a | MIC (μg/ml)
|
||
|---|---|---|---|
| Range | 50% | 90% | |
| Penicillin G | |||
| Erythromycin S (141) | 0.016-4.0 | 0.125 | 2.0 |
| Erythromycin R (120) | 0.016-16.0 | 1.0 | 4.0 |
| XRP 2868 | |||
| Erythromycin S | 0.06-0.25 | 0.125 | 0.25 |
| Erythromycin R | 0.06-1.0 | 0.25 | 0.5 |
| RPR 132552 | |||
| Erythromycin S | ≤0.5-16.0 | 4.0 | 8.0 |
| Erythromycin R | ≤0.5->64.0 | 4.0 | 32.0 |
| RPR 202868 | |||
| Erythromycin S | ≤0.5-32.0 | 4.0 | 8.0 |
| Erythromycin R | 2.0->64.0 | 16.0 | 64.0 |
| Pristinamycin | |||
| Erythromycin S | 0.125-0.5 | 0.25 | 0.25 |
| Erythromycin R | 0.125-1.0 | 0.25 | 0.5 |
| Quinupristin/dalfopristin | |||
| Erythromycin S | ≤0.06-1.0 | 0.5 | 0.5 |
| Erythromycin R | 0.25-1.0 | 0.5 | 1.0 |
| Quinupristin | |||
| Erythromycin S | ≤0.5-8.0 | 2.0 | 4.0 |
| Erythromycin R | 1.0->64.0 | 8.0 | 64.0 |
| Dalfopristin | |||
| Erythromycin S | 8.0->64.0 | 64.0 | >64.0 |
| Erythromycin R | 8.0->64.0 | >64.0 | >64.0 |
| Erythromycin A | |||
| Erythromycin S | 0.016-0.25 | 0.06 | 0.125 |
| Erythromycin R | 1.0->64.0 | >64.0 | >64.0 |
| Azithromycin | |||
| Erythromycin S | 0.03-0.25 | 0.125 | 0.125 |
| Erythromycin R | 1.0->64.0 | >64.0 | >64.0 |
| Clarithromycin | |||
| Erythromycin S | ≤0.008-0.125 | 0.03 | 0.06 |
| Erythromycin R | 0.25->64.0 | >64.0 | >64.0 |
| Clindamycin | |||
| Erythromycin S | ≤0.008-0.125 | 0.06 | 0.06 |
| Erythromycin R | 0.016->64.0 | 1.0 | >64.0 |
S, susceptible; R, resistant.
MICs of erythromycin A, azithromycin, clarithromycin, and clindamycin for pneumococci rose with those of penicillin G. Lower clindamycin MICs for erythromycin A-resistant strains reflected the presence of mef genes and ribosomal protein mutations; such strains were clindamycin susceptible. Complete cross-resistance occurred between erythromycin A, azithromycin, and clarithromycin.
Of the 150 H. influenzae strains, 79 produced β-lactamase. Of the 26 H. parainfluenzae strains, 8 were β-lactamase positive. Twenty-one of the 71 β-lactamase-negative H. influenzae strains were ampicillin resistant (MICs, ≥1.0 μg/ml) and were classified as BLNAR. Microdilution MICs are presented in Tables 3 and 4. There were no significant differences in MICs based upon β-lactamase production, ampicillin resistance, or serotype. MICs of all compounds had a unimodal distribution, with MICs at which 50% of strains were inhibited (MIC50s) and MIC90s (in micrograms per milliliter) as follows: XRP 2868, 0.25 and 1.0; RPR 132552A, 0.25 and 0.5; RPR 202868, >64.0 and >64.0; pristinamycin, 1.0 and 2.0; quinupristin/dalfopristin, 2.0 and 4.0; quinupristin, 32.0 and >64.0; dalfopristin, 2.0 and 8.0; erythromycin A, 4.0 and 8.0; azithromycin, 1.0 and 2.0; clarithromycin, 8.0 and 16.0. MICs of all compounds for H. parainfluenzae were generally 1 to 2 dilutions higher than those for H. influenzae, and unimodal distributions were observed.
TABLE 3.
MICs for H. influenzae
| Drug | MIC (μg/ml)
|
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| β-Lactamase-negative strains (n = 50)
|
β-Lactamase-positive strains (n = 79)
|
BLNAR strains (n = 21)
|
All strains (n = 150)
|
|||||||||
| Range | 50% | 90% | Range | 50% | 90% | Range | 50% | 90% | Range | 50% | 90% | |
| XRP 2868 | ≤0.06-1.0 | 0.25 | 0.5 | ≤0.06-1.0 | 0.25 | 1.0 | ≤0.06-1.0 | 0.25 | 0.5 | ≤0.06-1.0 | 0.25 | 1.0 |
| RPR 132522 | 0.12-1.0 | 0.25 | 0.5 | 0.12-1.0 | 0.25 | 0.5 | 0.12->8.0 | 0.25 | 0.5 | 0.12->8.0 | 0.25 | 0.5 |
| RPR 202868 | 2.0->64 | >64 | >64 | 2.0->64 | >64 | >64 | 2.0->64 | >64 | >64 | 2.0->64 | >64 | >64 |
| Pristinamycin | 0.5-2.0 | 1.0 | 2.0 | 0.12-4.0 | 1.0 | 2.0 | 0.25-4.0 | 1.0 | 1.0 | 0.12-4.0 | 1.0 | 2.0 |
| Quinupristin/dalfopristin | 1.0-8.0 | 2.0 | 4.0 | 0.25-8.0 | 4.0 | 4.0 | 1.0-8.0 | 2.0 | 4.0 | 0.25-8.0 | 2.0 | 4.0 |
| Quinupristin | 16->64 | 32 | >64 | 8.0->64 | 32 | >64 | 16->64 | 64 | >64 | 8.0->64 | 32 | >64 |
| Dalfopristin | 1.0-8.0 | 2.0 | 8.0 | 1.0-32 | 4.0 | 8.0 | 1.0->64 | 2.0 | 4.0 | 1.0->64 | 2.0 | 8.0 |
| Erythromycin | 2.0-16 | 4.0 | 8.0 | 0.5-16 | 4.0 | 8.0 | 1.0-16 | 4.0 | 8.0 | 0.5-16 | 4.0 | 8.0 |
| Azithromycin | 0.5-2.0 | 1.0 | 2.0 | 0.12-2.0 | 1.0 | 2.0 | 0.5-8.0 | 1.0 | 2.0 | ≤0.12-8.0 | 1.0 | 2.0 |
| Clarithromycin | 4.0-32 | 8.0 | 16 | 1.0-64 | 8.0 | 8.0 | 4.0-16 | 4.0 | 16 | 1.0-64 | 8.0 | 16.0 |
TABLE 4.
MICs for H. parainfluenzae
| Drug | MIC (μg/ml)
|
||||||||
|---|---|---|---|---|---|---|---|---|---|
| β-Lactamase-negative strains (n = 18)
|
β-Lactamase-positive strains (n = 8)
|
All strains (n = 26)
|
|||||||
| Range | 50% | 90% | Range | 50% | 90% | Range | 50% | 90% | |
| XRP 2868 | 0.12-2.0 | 1.0 | 2.0 | 0.12-4.0 | 1.0 | 1.0 | 0.12-4.0 | 1.0 | 2.0 |
| RPR 132552 | 0.06-2.0 | 0.5 | 2.0 | 20.06-4.0 | 1.0 | 1.0 | ≤0.06-4.0 | 0.5 | 2.0 |
| RPR 202868 | >64->64 | >64 | >64 | >64->64 | >64 | >64 | >64->64 | >64 | >64 |
| Pristinamycin | 0.5-8.0 | 4.0 | 4.0 | 1.0-8.0 | 4.0 | 4.0 | 0.5-8.0 | 4.0 | 4.0 |
| Quinupristin/dalfopristin | 1.0-16 | 8.0 | 16 | 2.0-32 | 8.0 | 16 | 1.0-32 | 8.0 | 16 |
| Quinupristin | 32->64 | >64 | >64 | 32->64 | >64 | >64 | 32->64 | >64 | >64 |
| Dalfopristin | 1.0-32 | 8.0 | 16 | 1.0-32 | 8.0 | 16 | 1.0-32 | 8.0 | 16 |
| Erythromycin | 1.0-8.0 | 2.0 | 4.0 | 1.0-8.0 | 4.0 | 4.0 | 1.0-8.0 | 2.0 | 4.0 |
| Azithromycin | 0.25-2.0 | 0.5 | 1.0 | 0.25-1.0 | 0.5 | 1.0 | 0.25-2.0 | 0.5 | 1.0 |
| Clarithromycin | 2.0-16 | 4.0 | 8.0 | 2.0-16 | 8.0 | 16 | 2.0-16 | 4.0 | 16 |
DISCUSSION
XPR 2868 is a new oral streptogramin composed of two semisynthetic synergistic components in a 70/30 (wt/wt) association: RPR 132552A (group A streptogramin) and RPR 202868 (group B streptogramin). The antibacterial spectrum of XPR 2868 includes gram-positive cocci, fastidious gram-negative rods involved in respiratory tract infections, and anaerobes. As with all other streptogramins (19), the compound is rapidly bactericidal, with a postantibiotic effect against pneumococci of 0.05 to 4.35 h, depending upon MIC and exposure time. XPR 2868 also selects for resistant mutants of Staphylococcus aureus in vitro at lower rates than other compounds tested (J. C. Barriere, E. Bacque, N. Berthaud, G. Dutruc-Rooset, G. Doerflinger, and G. Puchault, Abstr. 41st Intersci. Conf. Antimicrob. Agents Chemother., abstr. F-359, 2001; N. Berthaud, N. Diallo, B. Prevost, S. Lannier-Bonnamour, A. De Usatorre, and J. Hodgson, Abstr. 41st Intersci. Conf. Antimicrob. Agents Chemother., abstr. F-360, 2001; S. Dutka Malen, N. Berthaud, V. Boisrobert, F. Efremenko, A. M. Gouin, J. Martin, J. Rousseau, and J. Hodgson, Abstr. 41st Intersci. Conf. Antimicrob. Agents Chemother., abstr. F-361, 2001; S. Dutka Malen, N. Berthaud, O. Sergent, and J. Hodgson, Abstr. 41st Intersci. Conf. Antimicrob. Agents Chemother., abstr. F-362, 2001; L. M. Kelly, M. R. Ednie, A. Jacobs, A. Bryskier, C. Couturier, and P. C. Appelbaum, Abstr. 42nd Intersci. Conf. Antimicrob. Agents Chemother., abstr. F-1667, 2002). The MICs for both pneumococci and H. influenzae with XPR 2868 obtained in this study were similar to those reported above in preliminary studies.
Previous studies (8, 12, 15) have documented excellent activity of quinupristin/dalfopristin against macrolide-susceptible and -resistant pneumococci, with MICs similar to those obtained in the present study. Neither component of the combination alone had significant antipneumococcal activity. Approximately 10 years ago, an oral streptogramin, RPR 106972, was briefly evaluated but was not further developed. In preliminary studies (22), RPR 106972 MICs were similar to those of XRP 2868, with no significant activity of the two constituent components of either compound. Pristinamycin was also very active against all groups of pneumococci (22). As has been reported by others (11), macrolide resistance, and to a lesser extent clindamycin resistance, increased with that of penicillin G in our study. MICs of XRP 2868 and pristinamycin were usually 1 to 2 dilutions lower than those of quinupristin/dalfopristin.
Our results show that XRP 2868 had low MICs (≤1.0 μg/ml) for all H. influenzae strains tested, with slightly higher MICs for H. parainfluenzae. It is noteworthy that RPR 132552A, one of the two components of XRP 2868, alone was as effective as the combination against all strains. In all susceptible species, the two components of XRP 2868 act synergistically (Barriere et al., 41st ICAAC; Berthaud et al., 41st ICAAC; Dutka Malen et al., 41st ICAAC, abstr. F-361; Dutka Malen et al., 41st ICAAC, abstr. F-362; Kelly et al., 42nd ICAAC; A. Bryskier, personal communication). Quinupristin/dalfopristin and pristinamycin had MICs which were 2 to 3 dilutions higher than those of XRP 2868 and RPR 132552A (8, 15), while the macrolides yielded their usual unimodal distributions (11).
In summary, XRP 2868, a new oral streptogramin, had low MICs for all pneumococcal and Haemophilus strains tested, regardless of their susceptibilities to other agents. Pharmacokinetic/pharmacodynamic and toxicity studies are warranted before clinical evaluation of this compound can occur.
Acknowledgments
This study was supported by a grant from Aventis Pharma, Romainville, France.
REFERENCES
- 1.Agouridas, C., A. Bonnefoy, and J. F. Chantot. 1997. Antibacterial activity of RU 64004 (HMR 3004), a novel ketolide derivative active against respiratory pathogens. Antimicrob. Agents Chemother. 41:2149-2158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Appelbaum, P. C. 1992. Antimicrobial resistance in Streptococcus pneumoniae—an overview. Clin. Infect. Dis. 15:77-83. [DOI] [PubMed] [Google Scholar]
- 3.Block, S., C. J. Harrison, J. A. Hedrick, R. D. Tyler, R. A. Smith, E. Keegan, and S. A. Chartrand. 1995. Penicillin-resistant Streptococcus pneumoniae in acute otitis media: risk factors, susceptibility patterns and antimicrobial management. Pediatr. Infect. Dis. J. 14:751-759. [DOI] [PubMed] [Google Scholar]
- 4.Breiman, R. F., J. C. Butler, F. C. Tenover, J. A. Elliott, and R. R. Facklam. 1994. Emergence of drug-resistant pneumococcal infections in the United States. JAMA 271:1831-1835. [PubMed] [Google Scholar]
- 5.Bryskier, A. 2000. Ketolides-telithromycin: an example of a new class of antibacterial agents. Clin. Microbiol. Infect. 6:661-669. [DOI] [PubMed] [Google Scholar]
- 6.Credito, K. L., G. Lin, G. A. Pankuch, S. Bajaksouzian, M. R. Jacobs, and P. C. Appelbaum. 2001. Susceptibilities of Haemophilus influenzae and Moraxella catarrhalis to ABT-773 compared to their susceptibilities to 11 other agents. Antimicrob. Agents Chemother. 45:67-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Friedland, I. R., and G. H. McCracken, Jr. 1994. Management of infections caused by antibiotic-resistant Streptococcus pneumoniae. N. Engl. J. Med. 331:377-382. [DOI] [PubMed] [Google Scholar]
- 8.Fuchs, P., A. Barry, S. Brown, et al. 1998. Provisional quality control parameters and interpretive criteria for testing susceptibility of Streptococcus pneumoniae and Haemophilus influenzae to quinupristin/dalfopristin (RP 59500). Eur. J. Clin. Microbiol. Infect. Dis. 17:197-201. [DOI] [PubMed] [Google Scholar]
- 9.Jacobs, M. R. 1992. Treatment and diagnosis of infections caused by drug-resistant Streptococcus pneumoniae. Clin. Infect. Dis. 15:119-127. [DOI] [PubMed] [Google Scholar]
- 10.Jacobs, M. R., and P. C. Appelbaum. 1995. Antibiotic-resistant pneumococci. Rev. Med. Microbiol. 6:77-93. [Google Scholar]
- 11.Jacobs, M. R., S. Bajaksouzian, A. Zilles, G. Lin, G. A. Pankuch, and P. C. Appelbaum. 1999. Susceptibilities of Streptococcus pneumoniae and Haemophilus influenzae to 10 oral antimicrobial agents based on pharmacodynamic parameters: 1997 U.S. surveillance study. Antimicrob. Agents Chemother. 43:1901-1908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.King, A., J. May, and I. Phillips. 1998. Comparative activity of quinupristin/dalfopristin and RPR 106972 and the effect of medium on in vitro results. J. Antimicrob. Chemother. 42:711-719. [DOI] [PubMed] [Google Scholar]
- 13.Kozlov, R. S., T. M. Bogdanovitch, P. C. Appelbaum, L. Ednie, L. S. Stratchounski, M. R. Jacobs, and B. Bozdogan. 2002. Antistreptococcal activity of telithromycin compared with seven other drugs in relation to macrolide resistance mechanisms in Russia. Antimicrob. Agents Chemother. 46:2963-2968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Leclercq, R. 2001. Overcoming antimicrobial resistance: profile of a new ketolide antibacterial, telithromycin. J. Antimicrob. Chemother. 48(Suppl. T1):9-23. [DOI] [PubMed] [Google Scholar]
- 15.Marchese, A., and G. C. Schito. 1999. In vitro activity of quinupristin/dalfopristin against selected bacterial pathogens isolated in Italy. Clin. Microbiol. Infect. 5:488-495. [DOI] [PubMed] [Google Scholar]
- 16.Munoz, R., J. M. Musser, M. Crain, D. E. Briles, A. Marton, A. J. Parkinson, U. Sorensen, and A. Tomasz. 1992. Geographic distribution of penicillin-resistant clones of Streptococcus pneumoniae: characterization by penicillin-binding protein profile, surface protein A typing, and multilocus enzyme analysis. Clin. Infect. Dis. 15:112-118. [DOI] [PubMed] [Google Scholar]
- 17.Nagai, K., T. A. Davies, L. M Ednie, A. Bryskier, E. Palavecino, M. R. Jacobs, and P. C. Appelbaum. 2001. Activities of a new fluoroketolide, HMR 3787, and its (des)-fluor derivative RU 64399 compared to those of telithromycin, erythromycin A, azithromycin, clarithromycin and clindamycin against macrolide-susceptible or -resistant Streptococcus pneumoniae and S. pyogenes. Antimicrob. Agents Chemother. 45:3242-3245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.National Committee for Clinical Laboratory Standards. 2000. Methods for dilution antimicrobial susceptibility tests for bacteria that grow aerobically, 5th ed.; approved standard. NCCLS publication no. M7-A5. National Committee for Clinical Laboratory Standards, Wayne, Pa.
- 19.Pankuch, G. A., M. R. Jacobs, and P. C. Appelbaum. 1994. Study of comparative antipneumococcal activities of penicillin G, RP 59500, erythromycin, sparfloxacin, ciprofloxacin and vancomycin by using time-kill methodology. Antimicrob. Agents Chemother. 38:2065-2072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sethi, S., and T. F. Murphy. 2001. Bacterial infection in chronic obstructive pulmonary disease in 2000: a state-of-the-art review. Clin. Microbiol. Rev. 14:336-363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Spangler, S. K., M. R. Jacobs, and P. C. Appelbaum. 1992. Susceptibilities of penicillin-susceptible and -resistant strains of Streptococcus pneumoniae to RP 59500, vancomycin, erythromycin, PD 131628, sparfloxacin, temafloxacin, Win 57273, ofloxacin, and ciprofloxacin. Antimicrob. Agents Chemother. 36:856-859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Spangler, S. K., M. R. Jacobs, and P. C. Appelbaum. 1996. Activities of RPR 106972 (a new oral streptogramin), cefditoren (a new oral cephalosporin), two new oxazolidinones (U-100592 and U-100766), and other oral and parenteral agents against 203 penicillin-susceptible and -resistant pneumococci. Antimicrob. Agents Chemother. 40:481-484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ubukata, K., Y. Shibasaki, K. Yamamoto, N. Chiba, K. Hasegawa, Y. Takeuchi, K. Sunakawa, M. Inoue, and M. Konno. 2001. Association of amino acid substitutions in penicillin-binding protein 3 with β-lactam resistance in β-lactamase-negative ampicillin-resistant Haemophilus influenzae. Antimicrob. Agents Chemother. 45:1693-1699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zeckel, M. L., K. D. Jacobson, F. J. Guerra, D. G. Therasse, and D. Farlow. 1992. Loracarbef (LY 163892) versus amoxicillin/clavulanate in the treatment of acute exacerbations of chronic bronchitis. Clin. Ther. 14:214-229. [PubMed] [Google Scholar]