The burden of type 2 diabetes
Diabetes was first recognized 3500 years ago by the Ancient Egyptians. One of the first clinical descriptions was by Aretaeus, who practised in Cappadocia around 120 AD. He wrote that the condition was ‘fortunately rare’, but ‘short will be the life of the man in whom the disease is fully developed’ [1].
In modern society, the first statement is far from true. The incidence of diabetes has doubled every 20 years since 1945 [2]. In 1994 the world wide prevalence of type 2 (non-insulin dependent) diabetes was 99 million (1.8% of the population); by 2010 it is estimated that this figure will rise to 215 million (3.8%) [3].
The second statement is as true today as it was almost 2000 years ago. In the West, 44% of patients with type 2 diabetes die within 10 years of diagnosis [4], mostly from macrovascular disease; the incidence of and mortality from cardiovascular disease are 2–3 times greater than in the general population [5]. As the majority of patients develop complications, which are present in up to 50% even at the time of diagnosis [6], type 2 diabetes imposes a significant burden on health services, as well as on the individuals who suffer from this progressive and incurable disease. Currently the 2% of the UK population with diabetes consume 5% of the health service budget; by comparison the 12% with arthritis consume just 1.9% [7]. With the increasing prevalence of the condition, these figures will escalate. Prevention would be the ideal solution, but is currently a remote prospect. In the meantime any way of significantly reducing the burden of diabetes-related complications will have a major impact on patient well-being and on cost effectiveness of management.
The benefits of treatment ?
Until the early 1990s, there was no evidence that our management of diabetes had any beneficial impact on the incidence of vascular complications. On the contrary, the pioneering study of the 1960s, the University Group Diabetes Program (UGDP) [8], suggested that treatment with tolbutamide might be harmful. The study was designed to assess the impact of blood glucose lowering therapies on complications, with patients being randomly allocated to placebo, tolbutamide, phenformin, or insulin. The study was stopped after 8 years because of an increase in cardiovascular deaths in those receiving tolbutamide. However, for many years the design and conduct of the UGDP were subject to fierce debate which was never satisfactorily resolved; uncertainty continued about treatment and glycaemic targets for type 2 diabetes.
The Diabetes Control and Complications Trial (DCCT), published in 1993 [9], showed that intensive glycaemic control (i.e. keeping blood glucose as near to normal as possible) reduces the incidence and progression of microvascular complications (retinopathy, nephropathy and neuropathy) in type 1 diabetes. Whether the same holds true in type 2 diabetes remained uncertain. Intensive treatment often results in hyperinsulinaemia, with weight gain and an increase in hypoglycaemia [9], both of which have theoretical adverse effects on macrovascular disease, the major life threatening complication of type 2 diabetes. Patients with type 2 diabetes frequently have other risk factors for macrovascular disease, such as hypertension and hyperlipidaemia, the former having a prevalence of 40%-60% [10, 11]. Antihypertensive therapy reduces the risk of both cardiovascular and cerebrovascular disease in the general population [12], but to what extent these findings apply to type 2 diabetes was again not clear.
The United Kingdom Prospective Diabetes Study (UKPDS) was conceived to explore these uncertainties and provide clearer guidelines for the management of type 2 diabetes.
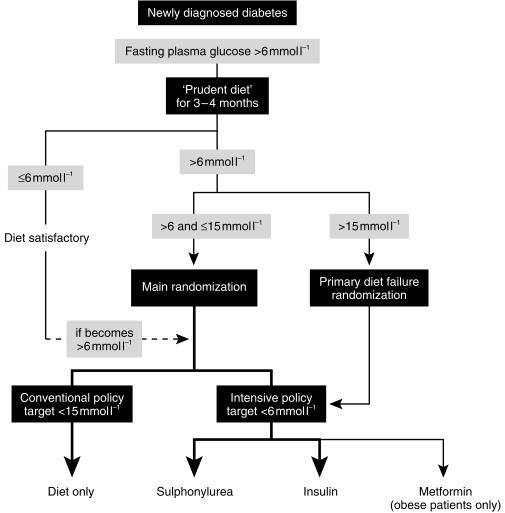
Design of the UKPDS (Figures 1–3)
Figure 1.
UKPDS–the principal questions.
Figure 3.
Design of UKPDS.
The UKPDS was set up in the late 1970s, by Dr Robert Turner and colleagues in Oxford. Over 7600 subjects at 23 centres across the UK were considered for inclusion; 5102 took part. It was the largest and longest study ever undertaken in diabetes; median follow-up was 10 years. As well as attempting to resolve unanswered clinical issues, the study generated a huge epidemiological database, comprising over 20 million data items.
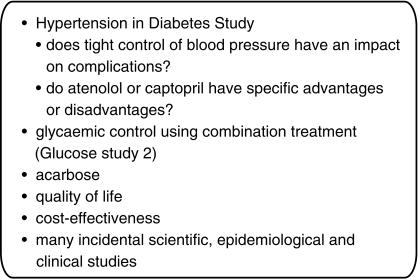
The primary aim was to determine the effect of intensive glycaemic control on the incidence of complications; the secondary aim was to assess whether there were differences between treatments (Figure 1). Protocol amendments were made to add topics not originally included. These strengthened the study by broadening its scope, but at the cost of complicating the treatment allocation, conduct and analysis of the study. Numerous substudies were embedded (Figure 2), the most notable being the Hypertension in Diabetes Study. Over 30 papers have been published from the UKPDS database, and many more are in preparation or planned.
Figure 2.
UKPDS–embedded studies.
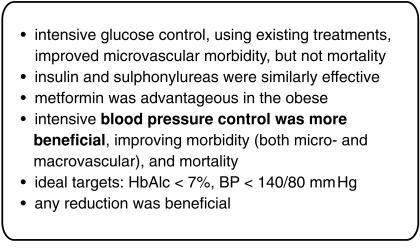
Key points (Figure 4)
Figure 4.
Key points.
Glucose control studies [13, 14]
Subjects were randomized to receive ‘conventional’ or ‘intensive’ therapy. In the former, the intention was to keep patients aymptomatic, with a fasting plasma glucose less than 15 mmol l−1; in the latter, the target fasting glucose was 6 mmol l−1. When diet failed to achieve these targets, subjects were randomized to sulphonylureas, insulin or metformin, the latter in obese patients only. When single treatments failed, combinations were used.
The results were primarily expressed in terms of aggregate end points: ‘any diabetes related end point’, which included both microvascular and macrovascular events, and ‘diabetes related death’. Twenty-one single end points were also defined. The emphasis on aggregate end-points allowed the study outcomes to be presented in a clinically meaningful way, i.e. overall risk. Their use also reduced the number of treatment comparisons, thus minimizing the chances of false-positive results, but had the disadvantage of concealing the magnitude of effects on individual end points.
Intensive glucose control significantly reduced any diabetes-related end point, but had no effect on mortality. The predominant effect of tighter control was a reduction of microvascular disease by a quarter, largely due to a reduction in laser photocoagulation. There was also a trend, just short of statistical significance, towards a reduction in macrovascular disease. No threshold was seen, i.e. any improvement in glycaemic control is beneficial. These findings are similar to those of the DCCT and a more recent study in Japanese patients with type 2 diabetes, in whom 6 years’ intensive therapy with insulin reduced the incidence of microvascular complications [15]. That the reduced occurrence of myocardial infarction was not significant may be due to type 2 statistical error. The study was set up to detect a 15% difference in events over the 10 years’ study period, and a larger number of macrovascular than microvascular events occurred, but the separation of HbA1c between intensive and conventionally treated groups was disappointingly low: 0.9% (half that in the DCCT). Had the separation of HbA1c between groups been greater, a significant effect of intensive control on macrovascular disease might have been demonstrated.
The secondary aim of the study was to compare the effects of different treatments for diabetes, since some have theoretical advantages and disadvantages. For example, sulphonylureas close myocardial ATP-sensitive potassium channels, which could impair ischaemia induced vasodilatation [16], perhaps explaining the results of the UGDP. In addition, some studies have suggested that hyperinsulinaemic states are atherogenic [17], and the increased incidence of hypoglycaemia with intensive control with insulin could theoretically precipitate a cerebrovascular or cardiovascular event. The UKPDS showed no difference in outcome between treatments, which is at first sight reassuring, but the study was powered to assess the effects of intensive therapy in general and it is unclear whether there is adequate power in this subgroup analysis. In addition, actual therapy often differed from allocated treatment, especially as patients required additional treatment over time. The results of this aspect of the study should therefore be interpreted with caution.
The results of metformin treatment are the most controversial [14]. Metformin use was associated with fewer aggregate end-points (including overall mortality) in obese patients. However the number of patients allocated to metformin was less than 10% of all those randomised. The findings could also be interpreted as indicating that insulin and sulphonylureas are equally harmful in the obese, possibly as a consequence of hyperinsulinaemia.
An unexpected finding was that the addition of metformin to sulphonylureas (in both obese and nonobese patients) was associated with increased mortality. The numbers involved in this subgroup analysis were very small, with few deaths (26 vs 14 in the group treated with sulphonylureas alone) and no difference in the incidence of heart attacks or strokes between the groups, only in the proportion who died. Furthermore, the mortality in the group treated by sulphonylureas alone was unexpectedly low. The authors therefore concluded that this anomalous result was likely to be have been due to chance.
Hypertension in Diabetes Study [18, 19]
One thousand one hundred and forty-eight patients took part. Half the participants were allocated to ‘tight control’ (target blood pressure less than 150/85 mm Hg) and were randomised to either atenolol or captopril, with other agents added as necessary. The remainder were allocated to ‘less tight control’ (target blood pressure less than 180/105 mm Hg); in these patients, drugs other than β-adrenoceptor blockers and ACE inhibitors were used. Mean blood pressure was 144/82 mm Hg in the tight control group, compared with 154/87 mm Hg in the less tight control group. One-third of patients allocated to tight control required three more drugs in the attempt to achieve the target blood pressure.
Tight control of blood pressure reduced both diabetes-related morbidity and mortality. Unlike glycaemic control, there was a significant effect on macrovascular as well as microvascular complications, with strokes and heart failure reduced by a half. Myocardial infarction was reduced by a fifth, but this was not statistically significant. As in the glucose control study, no threshold for risk was seen in the hypertension study. These are very impressive results, establishing that blood pressure control is at least as important as glycaemic control, if not more so, in the prevention of complications in type 2 diabetes.
In the last 2 years, the results of several other studies of hypertension which have included patients with diabetes have been published. These also demonstrated a reduction in macrovascular risk, including myocardial infarction [20, 21]. A variety of agents was used, but blood pressure differences between treatment and control groups were comparable with the UKPDS, and protective effects were observed despite shorter periods of follow up (2–5 years). Thus there is no doubt of the significance of blood pressure control in type 2 diabetes, but there remains the question whether particular drugs have advantages or disadvantages.
The UKPDS compared captopril and atenolol, both drugs having theoretical benefits. In the general population with hypertension, β-adrenoceptor blockers reduce macrovascular events and are specifically cardioprotective, reducing sudden death and further myocardial events in those with prior myocardial infarction [22]. ACE inhibitors improve survival in patients with heart failure [23, 24]; in type 1 diabetes, they reduce the progression of nephropathy [25, 26] and possibly retinopathy [27], but whether ACE inhibitors have specific advantages over other antihypertensive agents in type 2 diabetes is not yet agreed. Recently the ABCD trial showed a reduction in myocardial infarction in diabetic hypertensive subjects treated with an ACE inhibitor compared with a calcium channel blocker [28], but it was not clear whether the ACE inhibitor was especially beneficial or the calcium channel blocker relatively harmful, particularly as the groups were inadequately matched for concomitant medication. The UKPDS found that captopril and atenolol were equally effective as antihypertensive agents, in preventing macrovascular complications and in reducing the progression of retinopathy and albuminuria. The ACE inhibitor was however, better tolerated. These results are again reassuring at first sight, but, as with the glucose control study, type 2 errors cannot be excluded; there was a trend in favour of the atenolol treated group.
Therapeutic implications, study limitations and outstanding questions (Figures 5–7)
Figure 5.
Limitations of the study.
Figure 7.
Therapeutic implications.
The UKPDS demonstrated that any improvement in glycaemic control and blood pressure reduces diabetes-related complications. In trials such as this, patients are selected both by investigators and by themselves. The observation that UKPDS patients had a lower mortality than the general population with type 2 diabetes may be a reflection of this. What was achievable and acceptable to a trial population cannot be necessarily translated to everyone with type 2 diabetes. This must be remembered when applying the results of the study to clinical practice.
Figure 6.
Outstanding questions.
There is no doubt that aggressive management of blood pressure is important, particularly in reducing macrovascular disease, the main cause of morbidity and mortality in these patients. A target blood pressure of less than 140/80 is suggested by the authors. The fact that benefits are achieved within 2 or 3 years means that all patients should be treated irrespective of age. Clearly, achieving this goal will require aggressive follow up (patients in the UKPDS were seen 3 monthly), and this may not be acceptable to all patients. With one third requiring 3 or more agents to maintain target blood pressures, compliance will certainly be a problem in some.
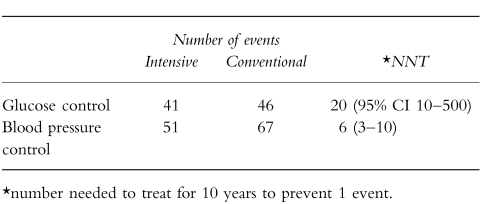
Whether intensive glycaemic control should be routinely introduced in type 2 diabetes is more controversial. Despite achieving statistical significance, the absolute risk reduction from intensive glycaemic control is small, with a reduction of 5 events over 10 years compared with 16 for blood pressure (Table 1). Furthermore, the benefits of glucose reduction did not accrue for several years, unlike intensive blood pressure control. Intensive glycaemic control, particularly with insulin, also leads to morbidity from hypoglycaemia and weight gain. Thus, unlike blood pressure control, intensive glycaemic control is not suitable for all patients, particularly the elderly, or those with existing severe complications. The small absolute risk reduction also needs to be compared with the possible effects of other risk factor interventions, e.g. treatment with aspirin, lipid lowering drugs or antioxidants. Despite these limitations, the UKPDS provides evidence and quantitative guidelines for those in whom intensive control is achievable.
Table 1.
Absolute risk.
The study also assessed effects of intensive treatment on quality of life; no adverse effect was apparent. One scale demonstrated that poor quality of life is related to complications rather than the treatments given [unpublished]. This is reassuring in implementing the results of the study, though the results may not apply equally to an unselected population.
One aspect of management inadequately addressed by the study is the optimal combination of drugs to be used either for glucose or blood pressure control. Different agents seemed equally effective, but the possibility of type 2 errors in these subgroup analyses cannot be excluded, as already discussed. To date, the effectiveness of insulin and oral hypoglycaemic agent combinations is not known, although there are unpublished data from the study on the combination of insulin and sulphonylureas. Data on possible dose-dependent effects of insulin, and the combination of insulin and metformin are lacking. For now, until further information is available, clinical practice should be based on achieving glucose and blood pressure reduction by whatever means best suits an individual patient.
In the study, patients were reviewed 3 monthly, rather than 6–12 monthly as in routine clinical practice, which has considerable resource implications. The reduction in blood pressure [29] and glucose [unpublished] achieved were relatively cheap, £48 and £22 per patient per year, respectively, when the benefits were discounted. These figures are valuable ammunition in the battle to improve services for patients. With 50% of patients presenting with complications, the issue of screening should also be addressed.
The UKPDS provides management guidelines for selected patients, but leaves many questions unanswered. The advantages of good care have been more clearly defined than ever before, but the huge gulf between the benefits achieved in the study and the many frustrations of everyday practice remains. In most centres, there are large numbers of patients with poor control of both blood glucose and blood pressure. Type 2 diabetes must at least be taken more seriously.
References
- 1.Reed JA. Aretaeus, the Cappadocian. Diabetes. 1954;3:419–421. doi: 10.2337/diab.3.5.419. [DOI] [PubMed] [Google Scholar]
- 2.Barnett T. Epidemiology, complications and costs of diabetes mellitus. In: Barnett Tony., editor. The insulin treatment of diabetes: a practical guide. London: E-map healthcare; 1998. pp. 6–9. [Google Scholar]
- 3.McCarty D, Zimnet P. Bayer: Leverkusen; 1994. Diabetes 1994–2010: global estimates and projections; pp. 1–46. [Google Scholar]
- 4.Panzam G. Mortality and survival in type II (non-insulin dependent) diabetes mellitus. Diabetologia. 1987;30:123–131. doi: 10.1007/BF00274216. [DOI] [PubMed] [Google Scholar]
- 5.Garcia MJ, McNamara PM, Gordon T, Kannell WB. Morbidity and mortality in diabetics in the Framingham population. Sixteen year follow-up study. Diabetes. 1974;23:105–111. doi: 10.2337/diab.23.2.105. [DOI] [PubMed] [Google Scholar]
- 6.UK Prospective Diabetes Study (UKPDS) Group. UK prospective diabetes study VIII. study design, progress and performance. Diabetologia. 1991;34:877–890. [PubMed] [Google Scholar]
- 7.Leese B. Economic evaluations of Type II diabetes. In The social and cost implications of Type II diabetes. In: Bengt Jönsson H, Krans MJ, editors. PharmacoEconomics 8. Suppl. Vol. 1. 1995. pp. 23–27. [DOI] [PubMed] [Google Scholar]
- 8.University Group Diabetes Programme. A study on the effects of hypoglycaemic agents on vascular complications in patients with adult-onset diabetes. Diabetes. 1976. pp. 1129–1153. [DOI] [PubMed]
- 9.The Diabetes Control and Complications Trial Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. 1993;329:977–986. doi: 10.1056/NEJM199309303291401. [DOI] [PubMed] [Google Scholar]
- 10.Hypertension in Diabetes Study Group HDS. 1. Prevalence of hypertension in newly presenting type 2 diabetic patients and the association with risk factors for cardio-vascular and diabetic complications. J Hypertens. 1993;11:309–317. doi: 10.1097/00004872-199303000-00012. [DOI] [PubMed] [Google Scholar]
- 11.Prescott-Clarke P, Primatesa P. Health Survey for England 1995. London: HMSO; 1997. [Google Scholar]
- 12.Collins R, Macmahon S. Blood pressure, antihypertensive drug treatment and the risks of stroke and coronary heart disease. Br Med J. 1994;50:272–298. doi: 10.1093/oxfordjournals.bmb.a072892. [DOI] [PubMed] [Google Scholar]
- 13.UK Prospective Diabetes Study (UKPDS) Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33) Lancet. 1998;352:837–853. [PubMed] [Google Scholar]
- 14.UK Prospective Diabetes Study (UKPDS) Group. Effect of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes (UKPDS 34) Lancet. 1998;352:854–865. [PubMed] [Google Scholar]
- 15.Ohkubo Y, Kishikawa H, Araki E, et al. Intensive insulin therapy prevents the progression of diabetic microvascular complications in Japanese patients with non-insulin dependent diabetes mellitus: a randomised prospective 6-year study. Diabet Res Clin Pract. 1995;28:103–117. doi: 10.1016/0168-8227(95)01064-k. [DOI] [PubMed] [Google Scholar]
- 16.Ashford ML, Bond CT, Blair TA, Adelman JP. Cloning and functional expression of a rat heart K-ATP channel. Nature. 1994;370:456–459. doi: 10.1038/370456a0. [DOI] [PubMed] [Google Scholar]
- 17.Stout RW. Insulin and atherosclerosis. In: Stout RW, editor. Diabetes and Atherosclerosis. Dordrecht, The Netherlands: Kluwer Academic publishers; 1992. –165.pp. 201 [Google Scholar]
- 18.UK Prospective Diabetes Study Group. Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38. Br Med J. 1998;317:703–713. [PMC free article] [PubMed] [Google Scholar]
- 19.UK Prospective Diabetes Study Group. Efficacy of atenolol and captopril in reducing risk of macrovascular and microvasvular complications in type 2 diabetes: UKPDS 39. Br Med J. 1998;317:713–720. [PMC free article] [PubMed] [Google Scholar]
- 20.Curb JD, Pressel SL, Cutler JA, et al. Effect of diuretic-based antihypertensive treatment on cardiovascular disease risk in older diabetic patients with isolated systolic hypertension. Systolic hypertension in the Elderly Program Cooperative Resaerch Group. JAMA. 1996;276:1886–1892. [PubMed] [Google Scholar]
- 21.Hansson L, Zanchetti A, Carruthers SG, et al. HOT Study Group. Effects of intensive blood-pressure lowering and low-dose aspirin in patients with hypertension: principal results of the Hypertension Optimal Treatment (HOT) randomised trial. Lancet. 1998;351:1755–1762. doi: 10.1016/s0140-6736(98)04311-6. [DOI] [PubMed] [Google Scholar]
- 22.Yusef S, Peto R, Lewis J, Collins R, Sleight P. Beta-blockade during and after myocardial infarction; an overview of the randomised trials. Progr Cardiovascular Dis. 1997;30:335–371. doi: 10.1016/s0033-0620(85)80003-7. [DOI] [PubMed] [Google Scholar]
- 23.CONSENSUS Trial Study Group. Effects of enalapril on mortality in severe congestive heart failure. New Eng J Med. 1987;316:1429–1435. doi: 10.1056/NEJM198706043162301. [DOI] [PubMed] [Google Scholar]
- 24.SOLVD Investigators. Effect of enalapril on mortality and the development of heart failure in asymptomatic patients with reduced left ventricular ejection fractions. New Eng J Med. 1992;327:685–691. doi: 10.1056/NEJM199209033271003. [DOI] [PubMed] [Google Scholar]
- 25.Björck S, Mulec H, Johnsen SA, Norden G, Aurell M. Renal protective effects in diabetic nephropathy. Br Med J. 1992;304:339–343. doi: 10.1136/bmj.304.6823.339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lewis EJ, Hunsicker LG, Bain RP, Rhode RD. for the Colloborative Study Group. The effect of angiotensin-converting enzyme inhibition on diabetic nephropathy. New Engl J Med. 1993;329:1456–1462. doi: 10.1056/NEJM199311113292004. [DOI] [PubMed] [Google Scholar]
- 27.Chaturvedi N, Sjolie AK, Stevenson JM, et al. Effect of lisinopril on progression of retinopathy in normotensive people with type 1 diabetes. The EUCLID Study Group. EURODIAB Controlled Trial of Lisinopril in Insulin-Dependent Diabetes Mellitus. Lancet. 1998;351:28–31. doi: 10.1016/s0140-6736(97)06209-0. [DOI] [PubMed] [Google Scholar]
- 28.Estacio RO, Schrier RW. Antihypertensive therapy in type 2 diabetes: implications of the Appropriate Blood pressure Control in Diabetes (ABCD) trial. Am J Cardiol. 1998;82:9R–14R. doi: 10.1016/s0002-9149(98)00750-4. [DOI] [PubMed] [Google Scholar]
- 29.UK Prospective Diabetes Study Group. Cost effectiveness analysis of improved blood pressure control in hypertensive patients with type 2 diabetes: UKPDS 40. Br Med J. 1998;317:720–726. [PMC free article] [PubMed] [Google Scholar]