Abstract
Aims
To determine whether a medicine review and education programme influences the compliance and knowledge of older people in general practice.
Methods
Older people taking at least three medicines were randomly allocated to a control or intervention group. Both groups received three visits from a clinical pharmacist:
Visit 1: Assessment and patients' medicines rationalized in intervention group.
Visit 2: Intervention group given medicines education.
Visit 3: Knowledge and compliance in both groups assessed by structured questionnaire
Results
Compliance in the intervention group was 91.3%, compared with 79.5% in the control group (P < 0.0001). The number of intervention group patients correctly understanding the purpose of their medicines increased from 58% to 88% on the second visit, compared with 67% to 70% in the control group (P < 0.0005).
Conclusions
A general practice based medication review and education programme improved medicine compliance and knowledge of older people in the short term.
Keywords: clinical pharmacist, education, elderly, general practice, medication compliance, medication knowledge
Introduction
Older people form 16% of the population [1], but consume 43% of prescribed medicines in England and Wales [2]. In common with younger patients, they do not always take their medicines as prescribed. This may be intentional or unintentional or a combination of both [3]. This often results in poor disease control, drug wastage and can also be a contributing factor to hospital admissions [4, 5]. The extent is difficult to quantify, but successive reviews estimate medication compliance to be approximately 50% [6–8]. It is difficult to specify the level of compliance necessary to benefit from treatment. However, in older people on complex therapy a figure of 85% has been suggested [9, 10].
Various strategies have been suggested to improve compliance. These include simplifying medication regimens [11], written and verbal information [10, 12] and more appropriate packaging of drugs [13]. A hospital based self-medication scheme, which combined all the above, has been shown to improve patient medicine compliance and knowledge 10 days after discharge [14]. However, the majority of older people are treated in general practice. This study investigated whether such a combined strategy could also be applied successfully to patients in primary care.
Methods
The study took place in a general practice in a suburban area of Leeds. A clinical pharmacist (the investigator) was based in the practice for the duration of the study. We recruited patients who were 65 years or older and taking three or more drugs. Patients were excluded if they:
lived in nursing or residential care
were totally dependent on another person to administer their medicines
had a terminal illness with a life expectancy of less than 1 year.
A list of patients in the practice who were 65 years or older (1477) was produced. Patients fulfilling the inclusion criteria were recruited sequentially from this list and randomly allocated to the intervention or control group, until the required number derived from the power calculation was passed. Altogether 181 patients were invited to take part and randomised to either the control or intervention group, 20 of these patients declined to take part. We received approval from the Local Research Ethics Committee and informed consent was obtained from the patients.
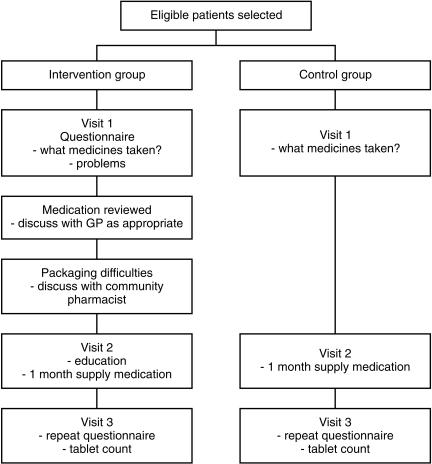
The study procedure is outlined in Figure 1.
Figure 1.
Study procedure.
Visit 1
The investigator visited patients at home and interviewed them about their medicines using a structured questionnaire. She asked patients what medicines they actually took, and their understanding of the purpose of each medicine. Control group patients were asked no further questions. The investigator assessed the ability of the intervention group patients to read labels, open containers and use nonoral medication and devices. She also rationalized the medication of these patients with their doctor as appropriate, aiming to reduce dose frequencies and discontinue unnecessary medication. The investigator liaised with the community pharmacist if patients needed modification to their medicine containers.
Visit 2
The investigator delivered 1 months supply of medication (from their usual pharmacy) to the patient. Other prescribed medication was removed with the patients' permission. There was no further involvement with control group patients. The investigator discussed the medication regimen with intervention patients and explained any changes. She discussed the correct way to take their medication and explained its purpose. The information was summarized on a hand written drug reminder chart (based on a previously described computer-generated chart [10]).
Visit 3
All patients were visited again 3 weeks after visit 2 and given a further 1 months supply of medication. The investigator asked patients to describe the medicines they took and their understanding of its purpose. She counted the number of tablets or capsules remaining from those medicines delivered at the previous visit.
Assessment of patients' compliance and knowledge of medication
We used a structured questionnaire to assess patient's understanding of the purpose of their medication, which was based on one used in a previous study [14]. The numbers of patients correctly describing the purpose of all their medicines at visits 1 and 3 was compared. Compliance was measured by tablet count and patient report. The number and variety of medicines taken in this type of population meant that these were the only practical methods available. A compliance score was calculated for each regularly scheduled oral medicine.
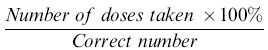 |
An overall mean compliance score was calculated for each patient.
A sample size of 160 was calculated to give 80% power to detect a 0.45 difference in confidence score, with P < 0.05. This effect size is equivalent to a difference between groups of around 10%, assuming a common standard deviation of 20%. The groups were compared for overall mean compliance score using the Mann–Whitney U-test. The numbers of patients who knew the purpose of the drugs at the assessment and follow-up visits were compared using the Chi-squared test.
Results
There were 161 patients recruited, 77 in the intervention group and 84 in the control group. Nine patients dropped out (five control and four intervention); six were admitted to hospital, two failed to comply with study conditions and one refused to continue at the second visit. Patients who dropped out were comparable with those who completed the study with respect to age, sex, social circumstances and number of medicines taken. The remaining 152 patients comprised 73 in the intervention group and 79 in the control. The two groups were well matched for age, sex, social circumstances and number of regularly scheduled medicines (see Table 1).
Table 1.
Details of patients in intervention and control groups.
| Detail | Intervention n = 77 | Control n = 84 |
|---|---|---|
| Mean age (range) | 77.5 (65–96) | 75.0 (65–88) |
| Number of men | 25 (33%) | 28 (33%) |
| Number living with spouse or relative | 42 (55%) | 48 (57%) |
| Mean number of regularly scheduled medicines (range) | 4.1 (2–8) | 3.9 (1–10) |
The mean number of medicines taken by intervention group patients was 4.1 (95% confidence interval 3.8–4.5). A change to the medicine regimen occurred in 34 (47%) patients resulting in a fall in the mean number taken to 3.9 (3.5–4.2). The mean difference in the number of medicines taken was −0.26 (95% confidence interval −0.43 to −0.10); P = 0.003, Wilcoxon signed rank test).
The mean compliance score for intervention patients was 91.3% (95% confidence interval 88.7% to 93.9%) and control group 79.5% (74.7% −84.3%); P < 0.0001. At the first visit 45/77 (58%) intervention group patients correctly described the purpose of their medicine compared with 56/84 (67%) of control group patients. At the third visit the figures were 64/73 (88%) and 55/79 (70%), respectively. The overall change in knowledge for both groups between the first and third visit was (with Yates' correction highly significantly different between the two groups using the Chi-square test (P = 0.0001).
Discussion
Our study shows that medication review and patient education in the community can significantly improve patient knowledge of and compliance with medication in the short term. These findings were similar to our hospital based self-medication programme [14], in which there was an improvement in patients' medication knowledge and compliance at 10 days after discharge. The improvement due to changes in medicine presentation and regime rationalization may be maintained in the longer term, but educational aspects would need to be regularly reinforced.
We found that patients did not comply with their medication for a variety of reasons, which the structured questionnaire was able to identify. Having identified reasons the pharmacist was able to negotiate the medicine regimen with the patient and doctor. This type of ‘therapeutic partnership’ was proposed by a recent working party on patient compliance [15]. Our intervention included aspects of both of the two main approaches to promote medication compliance: educational and behavioural. Patients were given appropriate information about their medicines, their regimen is simplified and the medication packaging individualized to their particular needs.
In our study the same person intervened and assessed the outcome. Two steps were taken to minimize bias; firstly a structured questionnaire was used for all three visits and secondly an independent observer reviewed the record of patient responses to questions. The response rates to the study were good, with only 20 patients refusing to participate.
The medicine regimen of the intervention group was changed in approximately half the patients. The amount of medicine education needed by patients varied considerably and reflected wide variations in baseline knowledge. This reinforces the point that older people are not an homogeneous group and should be treated as individuals. Furthermore, the investigator was unable to predict which patients would need help from a review of the case notes alone. The structured questionnaire proved to be an effective means of identifying these problems.
Older people, as a group, are the largest recipients of medication and so should be able to gain the greatest benefit. This is not always the case and one of the main contributing factors is lack of medication review [16]. By combining a medication review with in-depth medicine education, our programme offers a way of maximizing the benefits patients can receive from their medicines. If the programme were adapted for normal use most patients would be ambulant and able to attend the surgery or community pharmacy. After an initial assessment only those patients judged to need additional support would need to be followed up.
A practical way of screening older patients who needed help would be to incorporate a short structured questionnaire on medicine taking in the over-75 health check. Nurses are trained in patient assessment and are arguably better placed to undertake such assessments. The General Practitioner Contract of 1990 obliges doctors to offer over 75 year-olds annual health checks, and includes a review of medication [17]. However, the medication review process would still need to be led by a practitioner with in depth knowledge of medicines and the medication review process. Community pharmacists, whilst easily accessible to the public, are currently limited by lack of time and the inability to leave the pharmacy. Another option would be for a practice to contract the services of a clinically trained pharmacist who would be able to liase between all three professions.
It is clear that the challenge presented by the older people in managing their medicines is likely to increase in the general practice setting. A medication review and education programme could be a practical and cost-effective method of helping to meet this challenge.
Acknowledgments
This study was supported by a grant from the Department of Health under the Pharmacy Practice Research Enterprise Scheme. We thank all staff at the Marsh Street and Quarry Hill Surgeries, and the community pharmacists working in Oulton and Rothwell, for their support during this study.
References
- 1.Census Report for Great Britain. London: HMSO; 1991. Office of population census and survey. [Google Scholar]
- 2.A Prescription for Improvement. London: HMSO; 1994. Audit Commission Report. [Google Scholar]
- 3.Cooper JK, Love DW, Raffow PR. Intentional prescription non-adherence (non-compliance) by the elderly. J Am Geriatric Soc. 1982;30:329–333. doi: 10.1111/j.1532-5415.1982.tb05623.x. [DOI] [PubMed] [Google Scholar]
- 4.Williams EI, Fitton F. Br Med J. Vol. 297. 1998. Factors affecting early unplanned readmission of elderly patients to hospital; pp. 784–787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lindly CM, Tully MP, Paramsothy V, Tallis RC. Inappropriate medication is a major cause of adverse drug reactions in elderly patients. Age Ageing. 1992;21:294–300. doi: 10.1093/ageing/21.4.294. [DOI] [PubMed] [Google Scholar]
- 6.Ley P. Communicating with the patient. London: Croom-Helm; 1998. [Google Scholar]
- 7.Stockwell Morris L, Schulz RM. Patient compliance – an overview. J Clin Pharm Ther. 1992;17:283–295. doi: 10.1111/j.1365-2710.1992.tb01306.x. [DOI] [PubMed] [Google Scholar]
- 8.Wright EC. How many aunts has Matilda? Lancet. 1993;342:909–913. doi: 10.1016/0140-6736(93)91951-h. [DOI] [PubMed] [Google Scholar]
- 9.Parkin DM, Herney CR, Quirk J. Deviation from prescribed drug treatment after discharge from hospital. Br Med J. 1976;2:686–688. doi: 10.1136/bmj.2.6037.686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Raynor DK, Booth TG, Blenkinsopp A. Effects of computer generated reminder charts on patients' compliance with drug regimes. Br Med J. 1993;306:1158–1161. doi: 10.1136/bmj.306.6886.1158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Haynes RB. Determinants of compliance: The disease and mechanics of treatment. In: Haynes RB, et al., editors. Compliance in Healthcare. Baltimore: John Hopkins University Press; 1979. pp. 49–62. [Google Scholar]
- 12.MacDonald ET, MacDonald JB, Phoenix M. Improving drug compliance after hospital discharge. Br Med J. 1977;2:618–621. doi: 10.1136/bmj.2.6087.618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rudd P. Medication packaging: Simple solutions to non-adherence problems? Clin Pharmacol Ther. 1979;25:257–265. doi: 10.1002/cpt1979253257. [DOI] [PubMed] [Google Scholar]
- 14.Lowe CJ, Raynor DK, Courtney EA, Purvis J, Teale C. Effects of self-medication programme on knowledge of drugs and compliance with treatment in elderly patients. Br Med J. 1995;310:1229–1231. doi: 10.1136/bmj.310.6989.1229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Partnership in medicine taking: a consultative document. London and Herts: RPSGB & MSD; 1996. Royal Pharmaceutical Society of Great Britain. [Google Scholar]
- 16.Zermansky AG. Who controls repeats? Br J Gen Prac. 1996;46:643–647. [PMC free article] [PubMed] [Google Scholar]
- 17.General Practice in the national health service. A new contract. London: Department of Health and the Welsh Office; 1989. Department of health and the Welsh office. [Google Scholar]