Abstract
Aims
The aim of this study was to compare the effect profiles of i.v. administered rilmenidine aimed at the same target plasma concentration, but attained with different rates.
Methods
The study was placebo-controlled, randomized, double-blind, double-dummy, three-way, cross-over in nine healthy volunteers. All subjects randomly received either a fast infusion, a slow infusion or a placebo infusion. The target concentration was set at 8 ng ml−1 with a fivefold difference in the time to reach the maximum concentration. Saccadic eye movements, electroencephalography (EEG), blood pressure and heart rate were measured every half hour. Drug plasma concentrations, adverse events, salivary flow and visual analogue scales were obtained every hour.
Results
Changes in systolic/diastolic blood pressure at the end of the infusion were (mean ± s.d.) 13.3 ± 16.4/7.9 ± 7.5 mmHg with the fast infusion and 16.3 ± 12.7/10.2 ± 7.9 mmHg during the slow infusion, compared with 0.0 ± 13.2/1.3 ± 8.3 mmHg for the placebo occasion. Decrease of saccadic peak velocity (SPV) at the end of the infusion was 18.0 ± 5.2% during the fast infusion, 23.0 ± 7.0% with the slow infusion, and 6.1 ± 5.2% with placebo. PK/PD analysis showed similar concentration-dependent linear reduction in SPV and blood pressure up to the maximum observed rilmenidine plasma level for both the fast and the slow infusion.
Conclusions
The rate of infusion of rilmenidine in healthy volunteers does not influence the PK/PD relationship of saccadic eye movements and blood pressure up to the maximum observed rilmenidine plasma concentrations. Rilmenidine causes clear concentration-dependent blood pressure reductions in healthy volunteers.
Keywords: hypertension, pharmacokinetics/pharmacodynamics, rate, rilmenidine
Introduction
Rilmenidine (2-(dicyclopropylmethyl)-amino-2-oxazoline) is a centrally acting antihypertensive drug with binding selectivity to newly described I1 imidazoline receptors (identified in the lateral reticular nucleus in the brainstem and proximal tubular cells in the kidney) over α2-adrenoceptors [1–5]. It has dose-dependent blood pressure lowering effects above 0.5 mg in both healthy and hypertensive subjects. Rilmenidine is registered in several European countries as 1 mg tablets, and the most frequently used dose is one tablet once daily. Its concentration-related side-effects (sedation, xerostomia) are less important in comparison with congeners (e.g. clonidine), and are probably mediated by α2-adrenoceptor stimulation. Recently, the central nervous system effects of rilmenidine 1 and 2 mg orally were studied using saccadic eye movements, electroencephalography (EEG) and auditory evoked responses (AER) [6]. Rilmenidine caused a dose-dependent reduction of saccadic peak velocity (SPV), but little change in the other parameters. These effects were clearly smaller than with lorazepam 2.5 mg. Characterization of concentration-effect relationships for dry mouth and sedation (which were not determined in the previous study) may be helpful in optimizing the clinical dose.
In addition to the plasma concentrations, the rate of administration may also influence the effect. The classic example is provided by Kleinbloesem et al. [7] who demonstrated that a fast nifedipine-infusion did not lead to a blood pressure reduction in healthy volunteers, contrary to slow nifedipine administration. The current study was therefore designed to compare the effect profiles of i.v. administered rilmenidine aimed at the same target plasma concentration, but attained with different rates. The target concentration was set at high concentrations of 8 ng ml−1, i.e. above the therapeutic range [8]. The i.v. infusions were programmed to yield a fivefold difference in the time to reach the maximum concentration.
Methods
Design
This was a placebo-controlled, randomized, double-blind, double-dummy, three-way, cross-over, monocentric study in nine healthy volunteers, with a 1 week wash-out period.
Subjects
Subjects were male or female, healthy as determined during screening, who gave signed informed consent. The study was approved by the Medical Ethics Review Board of Leiden University Medical Center, and performed according to the principles of the Helsinki Declaration.
Treatments and measurement times
Infusions were performed with a volumetric infusion pump (Sigma 6000 +, Stöpler Instrumenten & Apparaten BV, Utrecht, The Netherlands) with a constant infusion rate of 0.25 ml min−1 over the first 4 h followed by a constant infusion rate of 1.0 ml min−1 over 1 h. The total volume infused was 120 ml. Infusion rates were determined after simulation using PK data from previous studies [17].
All subjects randomly received the following treatments:
Fast infusion: NaCl 0.9% over 4 h followed by rilmenidine infusion (1.8 mg h−1) over 1 h resulting in a total administered dose of 1.8 mg.
Slow infusion: rilmenidine (0.52 mg h−1) over 5 h resulting in a total administered dose of 2.6 mg.
Placebo infusion: NaCl 0.9% over 5 h.
Blood samples were obtained hourly for the first 6 h, with more frequent measurements around the end of the infusion (seven samples in the 4–6 h period), and at increasing time intervals for 24 h. Pharmacodynamic measurements were performed at half-hour intervals for 6 h and at decreasing frequency after the end of the infusion.
Blood pressure
Blood pressure and heart rate were measured with an automated blood pressure monitor (MPV1072, Nihon Kohden, Japan), which displays an average value for two sequential (duplicate) measurements at each time point. All measurements were made after the subject had been sitting in a semirecumbent position for at least 5 min.
Saccadic eye movements
Saccadic eye movements are a sensitive measure for central nervous system effects of rilmenidine and clonidine [6]. Saccadic eye movements were recorded as described previously [9–13] using a microcomputer-based system for data recording (Cambridge Electronics Design, Cambridge, UK), Nihon Kohden equipment for stimulus display, signal collection and amplification (Nihon Kohden Corporation, Tokyo, Japan), and disposable surface electrodes (Medicotest N-OO-S, Olstykke, Denmark). Average values of latency (= reaction time), peak saccadic velocity and inaccuracy (difference between stimulus angle and corresponding saccade in percentage) were calculated for all artifact-free saccades.
Electroencephalography (EEG)
EEG registrations have been used previously to quantify drug effects of rilmenidine and clonidine [7]. EEG registrations of total power for Delta-(< 4Hz), Theta-(4–7.5 Hz), Alpha-(7.5–12.5 Hz) and Beta-(12.5–30 Hz) activity were obtained at leads Fz-Cz and Pz-Oz., as described previously [10, 13].
Visual analogue scales
Visual analogue scales as originally described by Norris [14] were previously used to quantify subjective effects of benzodiazepines [9]. From the set of 16 lines three factors were derived as described by Bond & Lader [15], corresponding to alertness, mood and calmness. These factors were used to quantify subjective drug effects.
Salivary flow
Salivary production was estimated by measuring the weight increase of three dental rolls put into the oral cavity over a period of 3 min. Salivary production was assessed regularly up to 11 h after start of the infusion with an additional 24 h measurement. The dental rolls and accompanying collection tubes used for this measurement were Sarstedt neutral Salivettes7 (Sarstedt, Etten Leur, The Netherlands).
Analyses
Pharmacokinetics
Rilmenidine plasma levels were measured using gas chromatography/mass spectrometry [16]. The limit of detection was 0.3 ng ml−1 and the linearity of the assay has been checked over a range of 0.3–2 ng ml−1. The pharmacokinetics were described using NONMEM version V (NONMEM Project group, UCSF, San Francisco, CA), applying the first order conditional estimation (FOCE) method with the interaction option. Intra-individual error was modelled using a combination a constant (small) standard deviation and a constant coefficient of variation error model.
Pharmacokinetic/pharmacodynamic relationships
The observed pharmacodynamic effects were plotted agains the predicted rilmenidine concentrations for each individual. PK/PD modelling was performed using nonlinear mixed effect modelling as implemented in NONMEM. Rilmenidine pharmacokinetics were described using empirical Bayes estimates for the pharmacokinetic parameters. First order conditional estimation was used with an additive residual error. Models with and without a hypothetical effect compartment were used. Concentration-effect parameters for the fast infusion were determined along with parameters estimating the difference between slow and fast infusion. Additive interindividual variability was used on paired (within-subject) data. Only PD data obtained during and after the actual infusion of rilmenidine were used. Nested models were compared on the basis of the change in the minimum value of the objective function. A change of 3.8 (associated with 1 degree of freedom) was considered significant at P = 0.05. Contrast parameters between the slow and fast infusion are reported with approximate 95% confidence intervals calculated using two times the reported standard error.
Statistics
Changes from baseline at the end of the infusion were calculated for the pharmacodynamic parameters and compared between treatments using paired Student's t-tests. Differences are reported with 95% confidence intervals (95%CI). Data are shown as average with standard deviation (mean ± s.d.) unless indicated otherwise. Calculations were performed using SPSS for Windows V9.0.1 (SPSS, Inc., Chicago, IL).
Results
Demographics
All nine (five males, four females) subjects completed the study. Subjects were on average 22.2 years of age (range: 19–26 years). No serious adverse events occurred during the study.
Pharmacokinetics
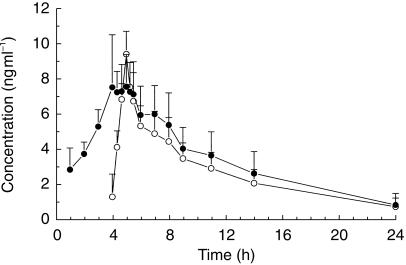
The time-concentration profiles for the two infusion regimens are shown in Figure 1. The maximal concentrations were 9.6 ± 1.0 ng ml−1 with the fast rate infusion, and 8.1 ± 2.4 ng ml−1 after the slow rate infusion. Prior experience with rilmenidine [17] and visual inspection of the individual data clearly indicated the need for a two-compartment model. The average pharmacokinetic parameters with interindividual variation coefficients (CV) were: clearance of 0.53 l min−1 (CV 31%), initial half-life of 15.7 min (CV 21%), terminal half-life of 361 min (CV 23%), and central volume of distribution of 129 l (CV 33%). These results correspond to the pharmacokinetics found in previous healthy volunteer studies after single dose administration [17].
Figure 1.
Time-concentration profiles (mean + s.d.) for slow (•) and fast (○) rilmenidine infusions.
Pharmacodynamics
Table 1 presents differences between the three treatments in changes from baseline at the end of the infusion for pharmacodynamic parameters.
Table 1.
Placebo corrected changes from baseline (95% confidence intervals) in pharmacodynamic parameters at the end of the infusion.
| Fast infusion | Slow infusion | Fast minus slow infusion | |
|---|---|---|---|
| Systolic BP (mmHg) | −13.3 (−23.3/−3.3) | −16.3 (−24.3/−8.4) | 3.0 (−9.6/15.6) |
| Diastolic BP (mmHg) | −6.6 (−11.8/−1.3) | −8.9 (−15.0/−2.8) | 2.3 (−5.8/10.5) |
| Heart rate (beats min−1) | −4.0 (−13.1/5.1) | −7.2 (−13.0/−1.5) | 3.2 (−3.9/10.4) |
| Saccadic peak velocity (% change) | −11.9 (−17.5/−6.2) | −16.9 (−22.6/−11.1) | 5.0 (−2.2/12.2) |
| EEG Delta Pz-Oz (% change) | 28.8 (11.4/46.1) | 28.7 (16.0/41.3) | −3.3 (−21.9/15.4) |
| EEG Beta Fz-Cz (% change) | 21.5 (−1.5/44.4) | 15.6 (−1.0/32.1) | 0.8 (−26.0/27.7) |
| VAS alertness (% change) | −11.9 (−29.0/5.1) | −13.9 (−29.4/1.6) | 2.0 (−13.5/17.4) |
| Salivary flow (% change) | −78.8 (−120.5/−37.1) | −82.3 (−122.4/−42.2) | 3.5 (−16.0/23.1) |
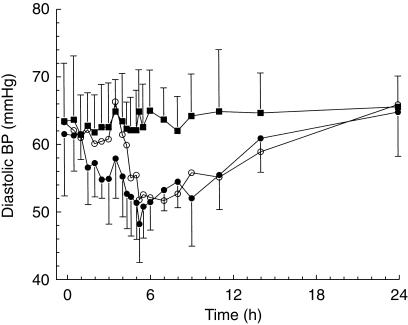
Blood pressure and heart rate
The average time effect curves for diastolic blood pressure are shown in Figure 2, and similar profiles were seen for systolic blood pressure. At baseline, blood pressure was similar for all three treatments. Changes in systolic/diastolic blood pressure at the end of the infusion were 13.3 ± 16.4/7.9 ± 7.5 mmHg with the fast infusion and 16.3 ± 12.7/10.2 ± 7.9 mmHg during the slow infusion, compared with 0.0 ± 13.2/1.3 ± 8.3 mmHg for the placebo occasion. Blood pressure decreased significantly compared with placebo, but no significant differences were observed between the slow and fast infusions (Table 1). Heart rate decreased slightly during slow but not fast rilmenidine infusion. At the end of the rilmenidine infusions, blood pressures slowly returned to normal, without apparent differences between the fast and slow rate infusions.
Figure 2.
Time-effect profiles (mean + s.d.) for diastolic blood pressure for placebo (▪), slow (•) and fast (○) rilmenidine infusions.
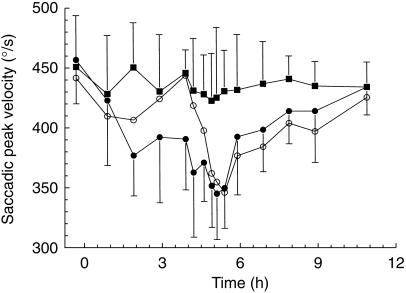
Saccadic eye movement
The average time profiles for the saccadic peak velocity (SPV) is shown in Figure 3. Decrease at the end of the infusion was 18.0 ± 5.2% during the fast infusion, 23.0 ± 7.0% with the slow infusion, and 6.1 ± 5.2% with placebo (Table 1). No significant differences were found in saccadic inaccuracy (as defined in the method section) and saccadic latency between the two active treatments.
Figure 3.
Time-effect profiles (mean + s.d.) for saccadic peak velocity for placebo (▪), slow (•) and fast (○) rilmenidine infusions.
Electroencephalography (EEG)
Delta Pz-Oz activity increased significantly during both slow and fast rilmenidine infusion compared with placebo, with a similar trend for EEG Beta Fz-Cz power (Table 1). There were no significant differences between the two active treatments. No significant differences were observed for any of the other EEG parameters.
Visual analogue scales (VAS)
Decrease in VAS scores of alertness at the end of the infusion was 13.6 ± 21.5% during the fast infusion and 15.6 ± 12.6% with the slow rate infusion, compared with 1.7 ± 11.9% with placebo (Table 1). After both infusion regimens, VAS-alertness returned to baseline within about 6 h. There were no significant effects for VAS scores of calmness and mood between the three treatments.
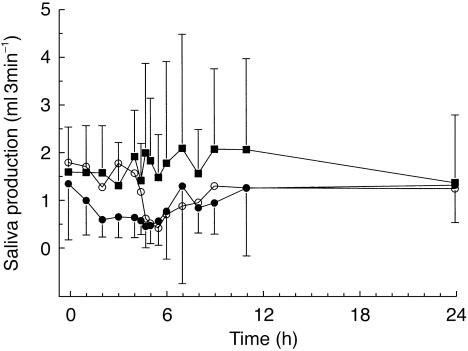
Salivary flow
The average time-effect curves for saliva production are shown in Figure 4. Saliva production decreased significantly to similar levels during both rilmenidine infusions (Table 1). At the end of the infusion, salivary flow had decreased 60.7 ± 13.2% during the fast infusion and 64.2 ± 19.9% during the slow infusion, compared with an increase of 18.1 ± 49.0% with placebo. The production of saliva slowly returned to normal baseline values after the infusions were stopped. No differences between slow and fast infusions were observed.
Figure 4.
Time-effect profiles (mean + s.d.) for saliva production for placebo (▪), slow (•) and fast (○) rilmenidine infusions.
Pharmacokinetic/pharmacodynamic relationships (PK/PD)
Concentration effect relationships between rilmenidine, saccadic peak velocity and diastolic blood pressure were examined. NONMEM parameters of the final models are presented in Table 2. For saccadic peak velocity, a linear concentration-effect model was used with a hypothetical effect compartment. Inclusion of this effect compartment resulted in a significant improvement in fit. Visual inspection of the individual concentration-effect graphs did not suggest the need for a more complex concentration-effect model. For diastolic blood pressure, a linear concentration-effect model was used without a hypothetical effect compartment. Inclusion of this effect compartment did not result in a significant improvement in fit, indicating that no hysteresis loop was observed. Visual inspection of the individual concentration-effect graphs did not suggest the need for a more complex concentration-effect model.
Table 2.
Mean PK/PD parameters for saccadic peak velocity and diastolic blood pressure for fast infusion and difference slow-fast infusion.
| Mean | 95% CI | Interindividual variability (s.d.) | |
|---|---|---|---|
| Saccadic peak velocity1 | |||
| t1/2Ke0 (min) | 5.6 | 1.5/9.7 | 0.0 (fixed) |
| Intercept fast infusion | 445 | 418/472 | 32 |
| Difference in intercept (slow-fast) | 11.8 | −6.9/30.5 | 16 |
| Slope fast infusion | −11.3 | −14.0/−8.6 | 1.3 |
| Difference in slope (slow-fast) | −1.1 | −3.1/0.8 | 0.0 |
| Residual error (s.d.) | 31.2 | ||
| Diastolic blood pressure2 | |||
| Intercept fast infusion | 61.4 | 58.2/64.6 | 3.1 |
| Difference in intercept (slow-fast) | 2.2 | −0.9/5.3 | 0.9 |
| Slope fast infusion | −1.20 | −1.68/−0.72 | 0.13 |
| Difference in slope (slow-fast) | −0.48 | −1.12/0.16 | 0.29 |
| Residual error (s.d.) | 4.29 | ||
units for intercepts in °/s; units for slopes in (°/s)/(ng ml−1).
units for intercepts in mmHg; units for slopes in (mmHg)/(ng ml−1).
Both slopes and intercepts for saccadic peak velocity and diastolic blood pressure did not differ between the slow and fast infusion (Table 2). However, the slope of the concentration-effect curves for diastolic blood pressure after the slow infusion seems to be larger than after the fast infusion. This is supported by the slightly lower concentrations and higher maximum effect on diastolic blood pressure after the slow infusion. The lack of significance could be due to the small population size.
Discussion
The current study showed clear relationships between the rilmendine concentration and reduction of blood pressure, saccadic peak velocity and salivary flow in normotensive subjects. Concentration-effect relationships were not affected by the rate of infusion per se, contrary to the effects of the calcium channel blocker nifedipine, where blood pressure reduction is larger with slow rate than with fast rate infusion [7]. This difference could be due to the different modes of action of the two antihypertensive agents. Nifedipine acts peripherally, and fast blood pressure reductions are probably rapidly counteracted by the baroreceptor reflex (with tachycardia), whereas slow increases in plasma concentrations allow the baroreceptor reflex to reset downward. Rilmenidine on the other hand acts centrally [18], possibly by reducing the level around which blood pressures fluctuate (without changes in heart rate), and may therefore evade counter-regulatory mechanisms. The central nervous system (CNS) effects of rilmenidine on saccadic peak velocity (SPV) and EEG-Delta- and -Beta-power were also not affected by the infusion rate. Another study where infusion rate-effects were evaluated on the same pharmacodynamic endpoints, was performed with temazepam [13]. This benzodiazepine caused a larger average increase of EEG-Beta activity after fast- than after slow-rate infusion, but this rate-effect was marginal and not observed for SPV or any other CNS-parameter. Thus, CNS-effects of temazepam and rilmenidine were unaffected by infusion rates.
In the current study, rilmenidine reduced SPV, similar to previous reports [6]. The average SPV-reductions at the end of the rilmenidine infusions were 18.0–23.0%. However, it is difficult to interpret these changes clinically. The concomitant occurrence of (statistically nonsignificant) reductions in visual analogue scales of alertness suggests that the SPV-reduction reflects sedation. However, the clinical relevance of these changes is difficult to determine, since saccadic eye movements have not been quantitatively related to clinical effects of centrally acting antihypertensive agents. For benzodiazepines, the clinical correlates of such SPV-changes are well-validated. Isolated SPV-effects at low benzodiazepine levels reflect a larger sensitivity of this biomarker to CNS-depression, than other pharmacodynamic or subjective measures [14]. Other CNS-effects only occur at higher benzodiazepine doses [9, 10]. The clinical relevance of SPV-reductions is not only determined by the size but also by the duration of the effect. The impact of short-lasting effects on daily life is subject to a wide intersubject variability, and strongly influenced by external factors like activities (e.g. demanding circumstances), day time, coffee-intake, etc. Also, the duration of treatment is relevant, since patients may develop tolerance to or become imperceptive of the sedative properties of drugs during prolonged treatment [12]. The current study showed clear concentration-dependent effects of rilmenidine on blood pressure and on the central nervous system. The clinical relevance of these effects remains to be demonstrated during prolonged treatment.
Acknowledgments
This study was funded by the Institut de Recherches Internationales Servier (I.R.I.S).
References
- 1.Ostermann G, Brisgand B, Schmitt J, Fillastre J-P. Efficacy and acceptability of ril menidine for mild to moderate systemic hypertension. Am J Cardiol. 1988;61:76D–80D. doi: 10.1016/0002-9149(88)90470-5. [DOI] [PubMed] [Google Scholar]
- 2.Fillastre J-P, Letac B, Galinier F, Le Bihan G, Schwartz J. A multicenter double-blind comparative study of rilmenidine and clonidine in 333 hypertensive patients. Am J Cardiol. 1988;61:81D–85D. doi: 10.1016/0002-9149(88)90471-7. [DOI] [PubMed] [Google Scholar]
- 3.Galley P, Manciet G, Hessel J-L, Michel JP. Antihypertensive efficacy and acceptability of rilmenidine in elderly hypertensive patients. Am J Cardiol. 1988;61:86D–90D. doi: 10.1016/0002-9149(88)90472-9. [DOI] [PubMed] [Google Scholar]
- 4.Mpoy M, Vandeleene B, Ketelslegers J-M, Lambert AE. Treatment of systemic hypertension in insulin-treated diabetes mellitus with rilmenidine. Am J Cardiol. 1988;61:91D–94D. doi: 10.1016/0002-9149(88)90473-0. [DOI] [PubMed] [Google Scholar]
- 5.Beau B, Mahieux F, Paraire M, Laurin S, Brisgand B, Vitou P. Efficacy and safety of rilmenidine for arterial hypertension. Am J Cardiol. 1988;61:95D–101D. doi: 10.1016/0002-9149(88)90474-2. [DOI] [PubMed] [Google Scholar]
- 6.Harron DWG, Hasson B, Regan M, McClelland RJ, King DJ. Effects of rilmenidine and clonidine on the electroencephalogram, saccadic eye movements and psychomotor function. J Cardiovasc Pharmacol. 1995;26(Suppl 2):S48–S54. [PubMed] [Google Scholar]
- 7.Kleinbloesem CH, Van Brummelen P, Danhof M, Faber H, Breimer DD. Rate of increase in the plasma concentration of nifedipine as a major determinant of its hemodynamic effects in humans. Clin Pharmacol Ther. 1987;41:26–30. doi: 10.1038/clpt.1987.5. [DOI] [PubMed] [Google Scholar]
- 8.Dollery CT, Davies DS. Pharmacodynamic effects on the cardiovascular system and acceptability of a single oral dose of S 3341 in the healthy volunteer. 1995 Internal report, Institut de Recherches Internationales Servier (I.R.I.S) [Google Scholar]
- 9.Van Steveninck AL, Schoemaker HC, Pieters MSM, Kroon R, Breimer DD, Cohen AF. A study comparing the sensitivities of adaptive tracking, eye movement analysis, and visual analogue lines to the effects of incremental doses of temazepam in healthy volunteers. Clin Pharmacol Ther. 1991;50:172–180. doi: 10.1038/clpt.1991.122. [DOI] [PubMed] [Google Scholar]
- 10.Van Steveninck AL. Thesis. State University Leiden; 1994. Section V, Conclusions. In Methods of assessment of central nervous system effects of drugs in man. [Google Scholar]
- 11.Van Steveninck AL, Van Berckel BNM, Schoemaker RC, Breimer DD, Van Gerven JMA, Cohen AF. The sensitivity of pharmacodynamic tests for the central nervous system effects of drugs on the effects of sleep deprivation. J Psychopharmacol. 1999;13:10–17. doi: 10.1177/026988119901300102. [DOI] [PubMed] [Google Scholar]
- 12.Van Steveninck AL, Wallnöfer AE, Schoemaker RC, et al. A study of the effects of long term on use individual sensitivity to temazepam and lorazepam in a clinical population. Br J Clin Pharmacol. 1997;44:267–275. doi: 10.1046/j.1365-2125.1997.t01-1-00580.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Van Steveninck AL, Schoemaker RC, Den Hartigh J, et al. Effects of intravenous temazepam (I); saccadic eye movements and EEG following fast and slow infusion to pseudo steady state. Clin Pharmacol Ther. 1994;55:535–545. doi: 10.1038/clpt.1994.67. [DOI] [PubMed] [Google Scholar]
- 14.Norris H. The action of sedatives on brain stem oculomotor systems in man. Neuro Pharm. 1971;10:181–191. doi: 10.1016/0028-3908(71)90039-6. [DOI] [PubMed] [Google Scholar]
- 15.Bond A, Lader M. The use of analogue scales in rating subjective feelings. Br J Med Psychol. 1974;47:211–218. [Google Scholar]
- 16.Ung HL, Girault J, Lefebvre MA, Mignot A, Fourtillan JB. Quantitative analysis of S-3341 in human plasma and urine by combined gas chromatography – negative ion chemical ionization mass spectrometry: 15 month inter-day precision and accuracy validation. Biomed Env Mass Spectr. 1987;14:289–293. doi: 10.1002/bms.1200140608. [DOI] [PubMed] [Google Scholar]
- 17.Institut de Recherches Internationales Servier (IRIS) Rilmenidine (S3341) investigator's brochure, Version 3. January 1994.
- 18.Van Zwieten PA. Central imidazoline receptors as a target for centrally acting antihypertensive drugs. Pharmacy World Science. 1995;17:186–190. doi: 10.1007/BF01870609. [DOI] [PubMed] [Google Scholar]