Abstract
Aims
Lamotrigine, an antiepileptic drug, is cleared from the systemic circulation mainly by glucuronidation. The possibility of changes in the pharmacokinetics of lamotrigine in plasma owing to hepatic dysfunction has been evaluated.
Methods
Thirty-six subjects, including 24 patients with various degrees of liver cirrhosis and 12 healthy volunteers received a single 100 mg dose of lamotrgine. Blood samples were taken for 7 days in all subjects, except nine with severe cirrhosis, who had a 29 day blood sampling period.
Results
The pharmacokinetics of lamotrigine were comparable between the patients with moderate cirrhosis (corresponding to Child-Pugh grade A) and the healthy subjects. Plasma oral clearance mean ratios (90% confidence interval) in patients with severe cirrhosis without or with ascites (corresponding, respectively, to Child-Pugh grade B and C) to healthy subjects were, respectively, 60% (44%, 83%) and 36% (25%, 52%). Plasma half-life mean ratios (90% confidence interval) in these two patient groups to healthy subjects were, respectively, 204% (149%, 278%) and 287% (202%, 408%).
Conclusions
Lamotrigine administered as a single oral dose of 100 mg was well tolerated in all groups. Initial, escalation and maintenance doses should generally be reduced by approximately 50 or 75% in patients with Child-Pugh Grade B or C cirrhosis. Escalation and maintenance doses should be adjusted according to clinical response.
Keywords: cirrhosis, lamotrigine, pharmacokinetics
Introduction
Lamotrigine is an established antiepileptic drug. Oral absorption of the drug is rapid and complete with the peak concentration reached at about 1–3 h and an absolute bioavailability of 98%. In plasma, lamotrigine is approximately 55% bound to proteins. Oral clearance and apparent volume of distribution average 0.35–0.59 ml min−1 kg−1 and 0.9–1.3 l kg−1, respectively. The mean plasma half-life obtained from various studies ranges from 24 to 37 h. Lamotrigine exhibits linear pharmacokinetics over a single-dose range of 50–400 mg [1, 2].
Lamotrigine is eliminated predominantly by glucuronic acid conjugation and the resulting conjugates are excreted renally. Glucuronidation may be impaired in liver disease depending on its severity. It is relatively preserved in compensated liver dysfunction, probably because of sufficient extrahepatic metabolic reserve. However, in severe liver cirrhosis it may be affected to a clinically significant extent [3] and this might cause an increase in drug exposure.
This trial was designed to compare the pharmacokinetics of lamotrigine in patients with moderate or severe cirrhosis and healthy subjects.
Methods
Study population
In total, 36 subjects participated in the study, including seven patients with severe cirrhosis without ascites, five patients with severe cirrhosis with ascites, 12 patients with moderate cirrhosis, and 12 healthy volunteers. The healthy subjects were matched for gender and age (± 5 years) with those with moderate cirrhosis.
Patients with cirrhosis had biopsy-proven disease which was classified as moderate or severe, depending on biochemical and clinical abnormalities (Table 1). Plasma albumin and bilirubin concentrations and level of prothrombin activity were used as markers of liver function [4]. Clinical evidence of portal-systemic shunting was taken as a specific marker of severe disease. Patients with severe cirrhosis with ascites (> 5 l of fluid) had clinical signs of fluid thrill or shifting dullness [4]. The Child-Pugh score [5] for the severity of cirrhosis was also determined at screening.
Table 1.
Summary of demographic characteristics and inclusion criteria of healthy controls and patients with cirrhosis.
| Healthy subjects (n = 12) | Moderate cirrhosis (n = 12) | Severe cirrhosis without ascites (n = 7) | Severe cirrhosis with ascites (n = 5) | ||
|---|---|---|---|---|---|
| Sex | Female | 4 | 4 | 3 | 1 |
| Male | 8 | 8 | 4 | 4 | |
| Age | Mean±s.d. | 50 ± 8.9 | 49 ± 8.9 | 51 ± 11.8 | 53 ± 6.7 |
| (years) | Median (range) | 53 (35–59) | 52 (37–59) | 55 (31–61) | 53 (46–61) |
| Height | Mean±s.d. | 171 ± 7.5 | 169 ± 7.6 | 168 ± 9.2 | 167 ± 8.3 |
| (cm) | Median (range) | 171 (158–180) | 168 (152–185) | 168 (155–180) | 170 (155–176) |
| Weight | Mean±s.d. | 71.2 ± 9.9 | 78.4 ± 15.2 | 67.1 ± 14.6 | 69.9 ± 12.8 |
| (kg) | Median (range) | 71.1 (55.0–88.2) | 79.5 (46.0–105.0) | 65.0 (50.0–92.0) | 73.0 (53.5–84.0) |
| Child-Pugh Score | Median | 5 | 9 | 12 | |
| at screening | Min–Max | 5–5 | 7–10 | 10–13 | |
| – Prothrombin activity | 375% | 355% | < 55% | < 55% | |
| Biological | – Serum bilirubin | ≤ 22 µmol l−1 | ≤ 60 µmol l−1 | > 60 µmol l−1 | > 60 µmol l−1 |
| criteria | – Serum albumin | ≥ 40 g l−1 | ≥ 28 g l−1 | < 28 g l−1 | < 28 g l−1 |
| – Biopsy-proven cirrhosis | No | Yes | Yes | Yes | |
| Clinical criteria | – History of ascites or hepatic encephalopathy | No | No or | Yes or Yes* | |
| – Recent gastrointestinal haemorrhage | No | No | Yes or | Yes or | |
| – Portal hypertensive gastropathy | No | No | Yes or | Yes or | |
| – Oesophageal varices | No | No | Yes | Yes |
> 5 l of ascitic fluid with clinical signs of fluid thrill or shifting dullness.
All subjects were included after having given written informed consent. The study was approved by the Committee for Protection of Human Subjects in Biomedical Research at Bicêtre Hospital (Le Kremlin Bicêtre, France).
Study design
This study was a multicentre, open design in parallel groups of subjects with chronic liver cirrhosis and in healthy subjects (control group). Following an overnight fast, subjects received a single oral dose of 100 mg lamotrigine with 200 ml of water.
For healthy subjects, subjects with moderate cirrhosis and the first three subjects with severe cirrhosis, blood was sampled before treatment (t0) and at 1, 2, 3, 4, 6, 8, 10, 24, 34, 48, 72, 96 120, 144 and 168 h after lamotrigine administration. For the nine remaining subjects with severe cirrhosis, blood was sampled before treatment (t0) and at 1, 2, 3, 4, 6, 8, 10, 24, 34, 48, 72, 120, 168, 240, 336, 408, 504, 576 and 672 h post dosing. At each time point, a 10 ml blood sample was drawn into a heparin tube and centrifuged. Plasma was immediately separated and stored at −20 °C until analysis.
Lamotrigine analysis
Plasma concentrations of lamotrigine were assayed using an h.p.l.c. method, with u.v. detection [6]. Plasma (400 µl) was automatically mixed with 100 µl monochloroacetic acid. This mixture was dialysed against potassium phosphate buffer, pH 7.0 and the resulting dialysate injected onto a Hypersil ODS cartridge. After washing the cartridge with 10% acetonitrile in water (v/v) to remove interfering compounds, the analyte was subjected to gradient h.p.l.c. using a Kromasil C8 column with u.v. detection at 270 nm. The lower limit of quantification of lamotrigine in plasma was 40 ng ml−1.
Pharmacokinetic analysis
The pharmacokinetic parameters of lamotrigine were determined using noncompartmental methods. The observed maximum plasma concentration (Cmax) and the time to reach the maximum concentration (tmax) were taken directly from the raw data. The area under the plasma concentration vs time curve from zero to the last measurable plasma concentration (AUC(0,t)) was calculated using a combination of linear (for rising concentrations) and logarithmic (for declining concentrations) trapezoidal methods. The area under the plasma concentration-time curve from zero to infinite time (AUC(0,∞)) was calculated by extrapolating the AUC(0,t) to infinity by the addition of Ct/λz where Ct is the last quantifiable concentration at time t and λz is the elimination rate constant as determined by log linear regression of the terminal phase concentration-time profile.
The apparent oral clearance CL/F, apparent volume of distribution Vz/F and elimination half-life t1/2 were calculated from the following equations:
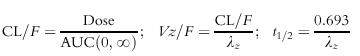 |
CL/F and Vz/F were further normalized by weight.
Relationships between pharmacokinetic parameters of lamotrigine and the severity of the liver cirrhosis were investigated by visual examination of plots of pharmacokinetic parameters vs the Child-Pugh score and by linear regression analysis where a relationship was suspected.
Statistical analysis
Pharmacokinetic parameters, except tmax, were compared by analysis of variance (anova) including gender and age as covariates to ensure that healthy subjects were matched with respect to these parameters to those with moderate cirrhosis. All parameters except tmax were log-transformed before analysis. For all log-transformed parameters, results were expressed as geometric least square (LS) mean ratios between each hepatic disease group and healthy subjects, together with their 90% confidence intervals (CI). tmax was compared between each hepatically impaired group and the healthy subjects using the Wilcoxon rank sum test. Estimates of the median difference between groups were calculated together with their 90% CI [7].
Results
Subjects
Demographic parameters are summarized in Table 1. There were 12 healthy subjects (eight males, four females, aged 35–59 years), 12 subjects with moderate cirrhosis (eight males, four females, aged 37–59 years), and 12 subjects with severe cirrhosis (eight males, four females, aged 31–61 years, seven without ascites and five with ascites). The demographic characteristics were similar among all groups. In the study population, the moderate disease group corresponds to Child-Pugh grade A, the severe disease without ascites group roughly corresponds to Child-Pugh grade B and the severe disease with ascites group to Child-Pugh grade C liver cirrhosis.
Pharmacokinetics
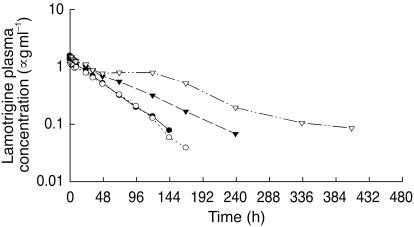
Pharmacokinetic parameters for lamotrigine are summarized in Table 2. The median plasma concentration vs time curves for lamotrigine are shown in Figure 1.
Table 2.
Results of analysis of variance for lamotrigine pharmacokinetic parameters in healthy individuals and patients with cirrhosis following a single 100 mg oral dose.
| Moberate cirrhosis(n = 12) | Severe cirrhosis without ascites(n = 12) | Severe cirrhosis without ascites(n = 12) | |||||
|---|---|---|---|---|---|---|---|
| Parameter (CI90%) | Control (n = 12)Geometric LSmean | Geometric LSmean | Geometric LSmean ratio (CI 90%) | Geometric LSmean | Geometric LSmean ratio° (CI 90%) | Geometric LSmean | Geometric LSmean ratio (CI 90%) |
| Cmax | 1.70 | 1.40 | 83%** | 1.58 | 93% | 1.56 | 92% |
| (µg ml−1) | (74%, 93%) | (81%, 106%) | (79%, 107%) | ||||
| tmax## | 1 | 1 | 0 | 1 | 0 | 2 | 1 |
| (h) | (0; 1) | (−1; 0) | (0; 5) | ||||
| AUC(0,∞) | 66.5 | 76.3 | 115% | 120 | 180%** | 197 | 297%*** |
| (µg ml−1 h) | (85%, 155%) | (127%, 255%) | (200%, 441%) | ||||
| CL/F | 0.36 | 0.29 | 81% | 0.22 | 60%* | 0.13 | 36%*** |
| (ml min−1 kg−1) | (61%, 106%) | (44%, 83%) | (25%, 52%) | ||||
| Vz/F | 0.98 | 1.06 | 109% | 1.21 | 123%** | 1.01 | 103% |
| (l kg−1) | (98%, 120%) | (109%, 139%) | (90%, 118%) | ||||
| t1/2 | 31.7 | 42.5 | 134%* | 64.5 | 204%*** | 90.9 | 287%*** |
| (h) | (103%, 175%) | (149%, 278%) | (202%, 408%) | ||||
median
median difference for tmax.
P < 0.10
P < 0.01
P < 0.001 compared with healthy volunteers. LS, least square; C
max, maximum plasma concentration; tmax, time to maximum plasma concentration, AUC∞, area under the plasma concentration-time curve from 0 to infinity; CL/F, apparent total clearance; Vz/F, apparent volume of distribution; t1/2, elimination half-life.
Figure 1.
Median lamotrigine plasma concentration vs time profiles following a single 100 mg oral dose in healthy volunteers (•), patients with moderate cirrhosis (○), patients with severe cirrhosis without ascites (▾) and patients with severe cirrhosis with ascites (▿).
The median plasma concentration-time profiles appeared comparable between the healthy subjects and patients with moderate liver disease (Figure 1). Cmax was 17% lower and t½ 34% longer in patients with moderate cirrhosis than in healthy controls. The other parameters, tmax, AUC, CL/F and Vz/F were all similar between the two groups.
Plasma drug concentrations were much higher in patients with severe cirrhosis, especially in those with ascites (Figure 1). Several pharmacokinetic parameters were statistically different in severe cirrhosis with or without ascites compared with the control group. Oral clearance was 40% less in subjects with severe cirrhosis without ascites and 64% less in severe cirrhosis with ascites compared with the controls. The half-lives were, respectively, twice and almost three times greater in the severe group without and with ascites than in healthy subjects. Consistent with the observations for oral clearance, a statistically significant increase in the mean values of AUC(0,∞) was observed in severe cirrhosis without and with ascites of 80% and 197%, respectively, in comparison to healthy controls. The apparent volume of distribution of lamotrigine was slightly higher in the severe cirrhosis group without ascites compared with controls.
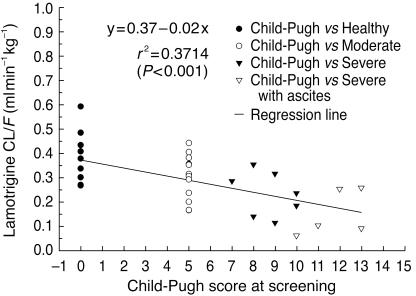
Figure 2 shows a significant correlation between oral clearance and Child-Pugh score at initial screening.
Figure 2.
The relationship between lamotrigine oral clearance (CL/F) and Child-Pugh score
Safety
Lamotrigine, administered as a single oral dose of 100 mg, was well tolerated in all groups. Among the 36 subjects who participated in the study, nine subjects (four healthy subjects, four subjects with moderate liver cirrhosis and one subject with severe liver cirrhosis) reported a total of 11 adverse events. All suffered from mild or moderate disease. Most adverse effects resolved during the day of occurrence and all within 2 days. Two required rescue medication (paracetamol for a headache and omeprazole for an epigastralgia). Two episodes of abdominal pain and one case of diarrhoea were considered as possibly related to lamotrigine. The relationship between the other adverse events and the study medication was unknown in four cases (headaches in three subjects and epigastralgia in another subject, all with liver cirrhosis), and unlikely in four cases.
Discussion
Values for the pharmacokinetic parameters of lamotrigine found in the control group are similar to those previously reported [1].
The pharmacokinetics of lamotrigine were not significantly altered in subjects with moderate cirrhosis. In contrast, subjects with severe cirrhosis with or without ascites showed significantly impaired pharmacokinetics. Thus, the oral clearance was lower, elimination half-life was longer and the AUC(0,∞) was greater than in control subjects, with a trend for an even larger difference in subjects with ascites. The presence of abundant ascites did not change the volume of distribution of lamotrigine, which is consistent with the lipophilic character of the drug (logP = 1.19 at pH 7.6) [8]. Ascites was only a consequence of more serious hepatic disease. The pharmacokinetic results from the severe liver cirrhosis group (7 without and 5 with ascites) should be interpreted carefully because of the small sample size. Despite this, statistically significant differences were found in several parameters between the severely affected groups and the controls.
The efficiency of drug removal by the liver is determined by hepatic blood flow, hepatic enzyme capacity and plasma protein binding [9]. Since lamotrigine is a low extraction ratio drug, metabolism is not influenced to any extent by reduced hepatic blood flow or by shunting. As the free fraction is 0.45, lamotrigine clearance is not affected greatly by plasma protein binding but is mainly determined by enzyme capacity. Since lamotrigine is extensively metabolized by glucuronidation, our results are consistent with previous findings that glucuronidation is little affected in moderate cirrhosis [10], but is impaired in patients with severe cirrhosis [11].
Based on the results of this study, there does not seem to be a need to change the dosage recommendations for patients with moderate liver cirrhosis. However, owing to a lower drug clearance in subjects with severe cirrhosis, dose reduction is recommended in these patients. Initial escalation and maintenance doses should generally be reduced by approximately 50 or 75% in patients with Child Grade B or C cirrhosis although overall adjustment should be done according to clinical response.
Further caution is required when treating patients with cirrhosis in the presence of antiepileptic drugs that induce (carbamazepine, phenytoin, phenobarbitone and primidone) or inhibit (valproate) lamotrigine metabolism [12].
Acknowledgments
We thank the ASTER Institute for the recruitment of healthy volunteers, Clinical Innovations Ltd (UK) for their contribution for the assay of lamotrigine and Roxane Fornacciari for her collaboration.
References
- 1.Goa KL, Ross SR, Chrisp P. Lamotrigine: a review of its pharmacological properties and clinical efficacy in epilepsy. Drugs. 1993;46:1–25. doi: 10.2165/00003495-199346010-00009. [DOI] [PubMed] [Google Scholar]
- 2.Yuen AWC, Peck AW. Lamotrigine pharmacokinetics: oral and i.v. infusion in man. Br J Clin Pharmacol. 1988;26:242. [Google Scholar]
- 3.Kroemer H, Klotz U. Glucuronidation of drugs. A reevaluation of the pharmacological significance of the conjugates and modulating factors. Clin Pharmacokinet. 1992;23(4):292–310. doi: 10.2165/00003088-199223040-00005. [DOI] [PubMed] [Google Scholar]
- 4.George J, Byth K. Influence of clinicopathological variables on CYP protein expression in human liver. J Gastroenterol Hepatol. 1996;11:33–39. doi: 10.1111/j.1440-1746.1996.tb00007.x. [DOI] [PubMed] [Google Scholar]
- 5.Pugh RNH, Murray-Lion IM, Dawson JL, Pietroni MC, Williams R. Transsection of the oesophagus for bleeding oesophageal varices. Br J Surg. 1973;60:289–296. doi: 10.1002/bjs.1800600817. [DOI] [PubMed] [Google Scholar]
- 6.Cooper JDH, Shearsby NJ, Taylor JE, Fook Sheung CTC. Simultaneous determination of lamotrigine and its glucuronide and methylated metabolites in human plasma by automated sequential trace enrichment of dialysates and gradient high-performance liquid chromatography. J Chromatogr B. 1997;702:227–233. doi: 10.1016/s0378-4347(97)00360-5. [DOI] [PubMed] [Google Scholar]
- 7.Conover WJ. Practical Non Parametric Statistics. Wiley & Sons; Confidence interval for the difference between two means; pp. 223–224. [Google Scholar]
- 8.Rambeck B, Wolf P. Lamotrigine. Clin Pharmacokinet. 1993;25:433–443. doi: 10.2165/00003088-199325060-00003. [DOI] [PubMed] [Google Scholar]
- 9.Tegeder I, Lotsch J, Geisslinger G. Pharmacokinetics of opioids in liver disease. Clin Pharmacokinet. 1999;37:17–40. doi: 10.2165/00003088-199937010-00002. [DOI] [PubMed] [Google Scholar]
- 10.Pacifici GM, Viani A, Franchi M, et al. Conjugation pathways in liver disease. Br J Clin Pharmacol. 1990;30:427–435. doi: 10.1111/j.1365-2125.1990.tb03794.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Macdonald JI, Wallace SM, Mahachai V, Verbeeck RK. Both phenolic and acyl glucuronidation pathways of diflunisal are impaired in liver cirrhosis. Eur J Clin Pharmacol. 1992;42:471–474. doi: 10.1007/BF00314852. [DOI] [PubMed] [Google Scholar]
- 12.Miller AA, Sawyer DA, Roth B, et al. New Anticonvulsant Drugs. London: Meldrum & Porter, John Libbey; 1986. Lamotrigine; pp. 165–177. [Google Scholar]