Abstract
Imaging-related medications (contrast agents) are commonly utilized to improve visualization of radiographic, computed tomography (CT), and magnetic resonance (MR) images. While traditional medications are used specifically for their pharmacological actions, the ideal imaging agent provides enhanced contrast with little biological interaction. The radiopaque agents, barium sulfate and iodinated contrast agents, confer “contrast” to x-ray films by their physical ability to directly absorb x-rays. Gadolinium-based MR agents enhance visualization of tissues when exposed to a magnetic field. Ferrous-ferric oxide–based paramagnetic agents provide negative contrast for MR liver studies. This article provides an overview of clinically relevant information for the imaging-related medications commonly in use. It reviews the safety improvements in new generations of drugs; risk factors and precautions for the reduction of severe adverse reactions (i.e., extravasation, contrast-induced nephropathy, metformin-induced lactic acidosis, and nephrogenic fibrosing dermopathy/nephrogenic systemic fibrosis); and the significance of diligent patient screening before contrast exposure and appropriate monitoring after exposure.
Imaging-related medications are commonly utilized to improve visualization of radiographic, computed tomography (CT), and magnetic resonance (MR) images. Until recently, pharmacists had little interaction with radiology or special imaging departments. Imaging-related products routinely fell under the auspices of a radiologist and were historically not even considered to be “medications.” These agents effectively had been excluded from the pharmacist's purview. Imaging-related medications are designated as prescription drugs in accordance with Food and Drug Administration (FDA) regulations and are subject to the investigational new drug and new drug application processes (1). In 2004, the Joint Commission confirmed that imaging-related medications are considered drugs and clarified medication management standard 4.10—“All prescriptions or medications orders are reviewed for appropriateness”—to include contrast agents, diagnostic agents, and radioactive agents.
This article begins by discussing two types of radiopaque agents: barium sulfate and iodinated contrast. X-rays readily pass through most body tissues, with the exception of bones. Radiopaque agents are utilized to enhance x-ray and CT scans by blocking x-ray transmission. Unlike barium sulfate agents, which are limited to oral and rectal administration, organic iodinated compounds can be administered by a variety of routes (e.g., oral, rectal, intravenous, intravesicular, intravertebral, and intrasplenic). One iodinated compound, iohexol, is FDA approved for intrathecal administration. After discussing radiopaque agents, the article reviews the more complex paramagnetic agents that enhance image contrast upon exposure to a strong magnetic field (2).
BARIUM PREPARATIONS
Barium sulfate is employed for radiologic imaging and other diagnostic procedures of the gastrointestinal tract. Its value is based not on its pharmacologic effects but rather on its inherent radiopaque nature. Barium sulfate is administered only by the oral or rectal route. It is neither absorbed nor metabolized in patients with a normal gastrointestinal tract and is excreted unchanged in the feces. Barium sulfate improves the visualization of the gastrointestinal tract in an x-ray image. The area where barium localizes will appear white on the x-ray film, creating distinctive definition and visual contrast between an organ and the surrounding tissues. The onset, duration, and degree of visualization of specific regions of the gastrointestinal tract are dependent upon many factors: normal versus diseased gastrointestinal tract, rate of peristalsis, method of administration, product formulation, and dosage and concentration of barium sulfate. Orally ingested suspensions provide sufficient contrast for visualization of the esophagus and stomach immediately. The small intestine may be visualized within 15 to 90 minutes. Rectally administered suspensions provide sufficient contrast of the colon immediately (3).
Safety issues
Adverse reactions with barium sulfate are infrequent, mild, and self-limiting. Cramping from distention of the intestine may occur as well as nausea and vomiting. Constipation or intestinal obstruction due to colon impaction may occur frequently in cystic fibrosis patients or those who are dehydrated. Although rare, mild allergic reactions (generalized pruritus, erythema, or urticaria) will respond to an antihistamine. More serious reactions include laryngeal edema, bronchospasm, or hypertension. Due to the increased likelihood of allergic reactions in atopic patients, a complete history must be obtained, including known or suspected allergies in addition to allergy-like symptoms (e.g., rhinitis, bronchial asthma, eczema, and urticaria), prior to any procedure (3).
Safe use of barium sulfate during pregnancy has not been established, as elective radiography of the abdomen is considered to be contraindicated during pregnancy due to fetal risk. Barium sulfate should be used in pregnant women only if the possible benefits outweigh the potential risks. Barium sulfate does not pass into breast milk and has not been reported to cause problems in breastfed babies (3).
IODINATED CONTRAST AGENTS
The most significant attribute of iodinated contrast agents is their iodine content. The relatively high atomic weight of iodine provides radiodensity and allows for radiographic contrast with surrounding tissues. Iodinated contrast agents do not differ significantly from one another in their resultant imaging capabilities. The degree of opacity produced is directly proportional to the total amount of iodine in the path of the x-rays. When similar concentrations, volumes, and administration rates are utilized, the radiographic image produced is very similar. The biggest difference in iodinated contrast agents is their adverse-reaction profiles (2, 4–6).
The first-generation contrast agents were all high-osmolar ionic monomers. High-osmolar contrast media (HOCM) have an osmolality 5 to 8 times that of blood. These agents are associated with high rates of adverse reactions when administered by the intravascular route due to the biological effects of high osmolality. For this reason, HOCM have fallen out of favor for routine intravascular injection and have been replaced by newer moieties with improved tolerability and safety profiles. Selected older agents are still commonly utilized in gastrointestinal procedures or retrograde urological procedures because they provide excellent imaging at a lower cost (6).
The second-generation contrast agents were developed to circumvent the problems associated with the first-generation HOCM. These nonionic monomers have water-soluble molecules that do not further dissociate in solution, allowing for a lower-osmolality product. Second-generation low-osmolality contrast media (LOCM) are associated with considerably fewer adverse reactions and improved intravascular tolerability. The first-generation ionic contrast agents could not be used for myelography due to neurotoxicity, so the discovery of a suitable nonionic agent in 1974 (metrizamide) revolutionized this procedure. Ten years later, the development of iohexol set the gold standard for nonionic imaging agents. Iohexol could be utilized in myelography with a neurotoxicity rate even lower than that of metrizamide (6, 7).
The only third-generation agent, iodixanol, was FDA approved in 1996. Iodixanol further improves upon the second-generation agents with its unique molecular structure. Iodixanol is an iso-osmolar, nonionic dimer that retains sufficient hydrophilic properties. An iso-osmolar agent is preferable for any procedure that exposes the patient to central nervous system, cardiovascular, or renal insult. It has found its niche for use in patients at high risk of contrast-induced nephrotoxicity. Because the general population has a low risk of developing nephrotoxicity and because of iodixanol's high cost (relative to the second-generation agents), its use is currently reserved only for high-risk patients (8–10).
Structural and physical characteristics
The basic building block of iodinated contrast agents is a benzene ring with three iodine molecules attached at positions 2, 4, and 6. Side chains (at positions 3 and 5) are modified with hydroxyl groups or other molecules that further define an agent's properties. The agents may exist as monomers (one benzene ring) or dimers (two benzene rings). Three defining physical characteristics of iodinated contrast agents—ionicity, osmolality, and viscosity—play a distinct role in the tolerance and adverse reaction profiles (8).
Ionicity
Ionicity is an important characteristic of iodine-containing agents. Compounds are classified as either ionic or nonionic. The ionic compounds dissociate in solution and therefore have a high osmolality. The anion is the radiopaque portion of the molecule, but both the anion and cation are osmotically active. Compared with nonionic LOCM, ionic HOCM tend to have more adverse hemodynamic effects, particularly in patients with coronary artery disease. The nonionics are water soluble but do not dissociate in solution. This is an advantageous quality, as nonionic agents will have a lower osmolality because there are fewer particles in solution. The nonionic compounds are more hydrophilic than ionic agents, resulting in lower osmolality, reduced protein binding, reduced tissue binding, and a reduced tendency to cross cell membranes. The potential biological effects of increased ionicity may explain deleterious effects on hemodynamic status and cardiac rhythm and function (8–11).
Osmality
Closely related to the property of ionicity is osmolality. (Osmolality is the number of moles of osmotically active particles present in solution per kilogram of solvent.) Contrast agents are classified into three groups. High-osmolar (≥1400 mOsm/kg) agents include the ionic monomers. Low-osmolar (780–800 mOsm/kg) agents include nonionic monomers. Iso-osmolar agents (approximately 300 mOsm/kg) include the nonionic dimers (8).
Osmolality is an important characteristic. As the osmolality of agents is reduced towards iso-osmolality, tolerability and safety profiles improve. At the level of patient comfort, patients report an increased incidence of pain or warmth sensations when higher-osmolar contrast agents are administered. When a high-osmolar load is injected intravascularly, water may be pulled from the interstitium into the vascular system, resulting in blood volume expansion. Patients with impaired cardiac function may become decompensated because of right heart volume overload (8, 12). These untoward effects are significantly reduced when iso-osmotic agents are used. Another deleterious effect of a high-osmolar load may be the physical effects on red blood cells. In a high-osmotic environment (>280–300 mOsm), water can also be drawn from red blood cells, resulting in a deformed and rigid cell that may not be able to pass easily through capillary beds. Thrombosis or ischemia may occur, especially in the brain and myocardium (10).
An iso-osmolar contrast agent may be preferable in any vascular territory where the endothelium is sensitive to the osmolality, such as the brain, heart, and kidneys. Studies show that iso-osmolar contrast agents affect the blood-brain barrier to a lesser degree than LOCM. The rhythm and the function of the heart may also be influenced to a lesser degree by iso-osmolar agents than by LOCM (9). Based on available literature, LOCM are associated with an overall lower risk of contrast-induced nephropathy than HOCM. Nonionic, iso-osmolar contrast agents are the least nephrotoxic and are better tolerated by patients during intravenous injection (2, 11).
Viscosity
The viscosity of a contrast agent merits considerable attention because viscosity affects the rate of intravascular injection. The goal is to provide sufficient iodine content at the site of scanning to optimize visualization. The rate of injection, sometimes a limiting factor due to high viscosity, may limit optimal scanning opportunities. While warming the contrast agent to body temperature decreases the viscosity and allows for a more rapid injection rate, higher flow rates have increased physiochemotoxic reactions and adverse reactions. In some cases, it is a delicate balance of timing—delivering adequate iodine to a location in a timely manner to allow for optimal scanning while maintaining minimal risk of adverse reactions. Highly concentrated agents may be an alternative since they provide large iodine loads with low flow rates. However, due to their high viscosity, the contrast agent may not mix well with the patient's blood and the final contrast enhancement may vary. Physiological factors such as blood volume and circulation time may also have an impact on enhancement (12, 13).
Clinical pharmacology and indications
Diagnostic enteral radiopaque agents have few known pharmacological effects. Oral administration is utilized for evaluation of the esophagus, stomach, or proximal small intestine. Rectal administration provides examination of the colon. A mild laxative effect is attributable to high osmolarity.
Intravenous administration is utilized in various studies: angiocardiography, aortography, selective renal arteriography, excretory urography, contrast enhancement in CT head and body imaging, and central or renal venography. Intravesical instillation may be used in bladder examination or hysterosalpingography. Intravertebral disk or spleen injection is performed with diatrizoate meglumine only. Selected iohexol concentrations are appropriate for intrathecal administration (14).
Absorption, onset, duration, metabolism, excretion, and time to peak opacification
When administered by the oral or rectal route, absorption of diagnostic enteral iodinated contrast agents is very poor. For this reason, enteral administration has few known pharmacological effects or adverse reactions. Excretion is through the fecal route and is dependent on gastrointestinal transit time (14).
Intravascularly administered agents are immediately diluted in the circulating blood volume and rapidly distributed throughout extracellular fluid. Protein binding is very low, and there appears to be no significant deposition in tissues. No significant metabolism, deiodination, or biotransformation occurs. Elimination is primarily renal. In patients with normal renal function, 95% to 100% of the intravenous dose is renally excreted;1% to 2% is excreted via biliary elimination and possibly via the intestinal mucosa. In patients with severe renal function, up to 20% of the administered dose is recovered in the feces within 48 hours. Iodinated contrast agents are completely dialyzable in two to three sessions. The half-life in normal renal function is 30 to 60 minutes but is delayed to 20 to 140 hours in patients with severe renal function impairment (7, 14, 15).
During intracavity or intravesical instillation, contrast agents are rapidly absorbed into the surrounding tissue and eliminated primarily by the kidneys. Small amounts may be absorbed through the bladder with subsequent renal elimination. Exams of the uterus (hysterosalpingography) and bladder (voiding cystourethrography) involve the almost immediate drainage of contrast medium from the cavity upon conclusion of the radiographic procedure (14).
Intrathecal administration is currently limited to only one nonionic contrast agent approved by the FDA for such use: iohexol. In the mid-1980s, specific concentrations of iohexol were approved for intrathecal administration: Omnipaque180, -240, and -300. Iohexol proved to be significantly less neurotoxic than the first-generation ionic agents. Slow diffusion of iohexol takes place throughout the cerebrospinal fluid with subsequent absorption into the bloodstream and renal elimination (14).
Many radiological contrast agents are neurotoxic. Misadministration of ionic contrast media intrathecally can result in serious adverse reactions: “death, convulsions, cerebral hemorrhage, coma, paralysis, arachnoiditis, acute renal failure, cardiac arrest, seizures, rhabdomyolysis, hyperthermia, and brain edema” (16). Immediate recognition of the mistake and prompt aggressive treatment may lessen the likelihood of harm or death (7). In 1994, the FDA required manufacturers of iodinated contrast agents other than iohexol to place warnings on each vial, package, and package insert of the serious adverse reactions resulting from intrathecal administration (7).
Time to peak opacification is dependent on the route of administration. In angiography, time to peak opacification is immediate after intravenous administration. In urography, renal parenchyma, including the renal cortex, is visible 1 minute after rapid injection. Optimal opacification is directly dependent on the final urinary iodine concentration, urine volume within the respective regions of the urinary tract, and kidney glomerular filtration rate. Calyces, pelves, and ureters are visualized 10 to 15 minutes after bolus injection (14).
Pregnancy category and breast-feeding
Most iodinated contrast agents are classified as pregnancy category B. Diatrizoate meglumine and diatrizoate meglumine sodium are listed as category C. Before administration of the drug to women of childbearing potential, the benefit to the patient should be carefully weighed against the possible risk Intravenous to the fetus (14, 17).
For oral and rectal solutions, studies with diatrizoates have not been done in humans. Elective contrast radiography of the abdomen is usually not recommended during pregnancy because of the risks to the fetus from radiation exposure. Studies in animals have not shown that diatrizoate sodium causes adverse effects in the fetus.
For parenteral solutions, studies with diatrizoates have not been done in humans or animals. Intravenous products cross the placenta, probably by simple diffusion, and are evenly distributed in fetal tissues. Intra-amniotic injection of diatrizoates has been reported to suppress the fetal thyroid gland (14).
Only a small amount of an orally or rectally administered iodinated contrast dose is absorbed by the mother. One percent of that dose is excreted in breast milk, of which 2% is absorbed by the baby. Intravenously administered diatrizoate salts are excreted unchanged in human milk. Although the risk to nursing infants is low, package inserts for iodin ated contrast media recommend discarding breast milk for 24 hours after exposure and substituting bottle feedings (8, 14).
Laboratory test interactions
When thyroid function tests are indicated, it is recommended that they be performed prior to the administration of any iodinated agent. Studies that are dependent on iodine estimations will not accurately reflect thyroid function for up to 16 days after exposure. However, thyroid function can be evaluated after the use of these agents by using T3 resin uptake or total or free thyroxin T4 assays, as they are not affected (15, 18).
Product overview
The iodinated contrast agents are summarized in Table 1. For all agents, information in the most current product inserts should supersede all other information. FDA-approved indications for the same product are concentration specific.
Table 1.
Iodinated contrast agents used in computed tomography
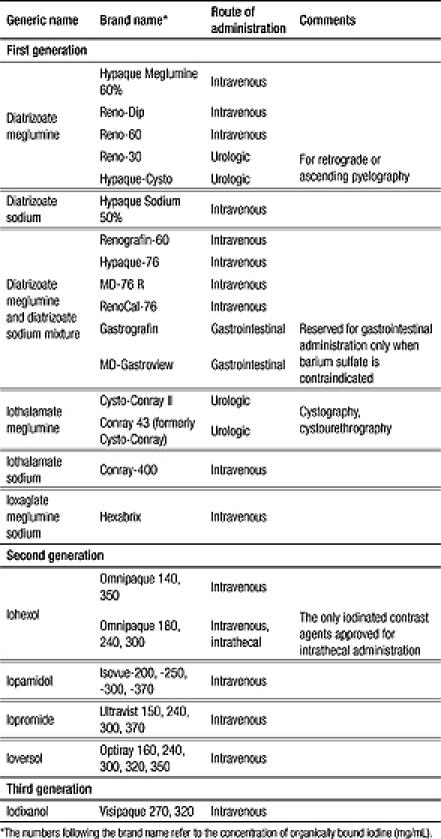
First-generation ionic agents have limited usage now that lower-osmolality products are available. The diatrizoate products are used for organ and tissue enhancement in CT, x-ray, and fluoroscopy. Since high osmolality is not a major concern in nonvascular procedures, selected products are reserved for retrograde cystourethrography when intravenous excretion urography is contraindicated. Several products are restricted to oral administration and are used as alternatives when a viscous agent such as barium sulfate (which is not water soluble) is contraindicated.
The second-generation nonionic monomers are used for angiocardiography, arteriography of cerebral arteries, CT of the head, digital subtraction angiography, intravenous pyelography, and peripheral angiography. Orally administered iohexol produces good visualization of the gastrointestinal tract and may be advantageous when barium sulfate is contraindicated (i.e., in patients with suspected bowel perforation). Selected concentrations of iohexol (Omnipaque−180, −240, or −300) are approved for intrathecal administration (14).
The only third-generation iodinated contrast agent currently approved in the USA is iodixanol (Visipaque). The product has the advantage of delivering twice the iodine of other nonionic contrast agents in an iso-osmotic product. High-risk patients may be less likely to develop adverse effects or contrast-induced nephropathy when exposed to iodixanol. However, since iodixanol is more expensive than iohexol and other conventional iodinated contrast agents, its use is currently limited to high-risk patients (16).
ADVERSE REACTIONS TO IODINATED CONTRAST AGENTS
Most adverse reactions following exposure to iodinated contrast agents are mild to moderate and self-limiting. HOCM induce mild adverse reactions (nausea, vomiting, and injection pain) with a frequency of >10%. More severe reactions (bronchospasm, edema, hypotensive shock, and renal dysfunction) occur infrequently (<2%). Serious, life-threatening, and fatal reactions occur immediately or within 20 minutes of exposure. These reactions have been linked not only to the drugs’ high osmolality but also to their ability to bind calcium. Regardless of the specific contrast agent used, serious adverse reactions occur more often during angiocardiography than during other procedures (4, 6, 14).
For the diatrizoate compounds, the sodium salts are associated with a higher degree of toxic effects. Especially susceptible are patients vulnerable to high sodium loads, such as those with cardiac, hepatic, or renal disease. Peripheral vasodilation and other side effects increase when the sodium concentration increases. The meglumine salt is less toxic but carries its own problems due to its increased viscosity. This is why the two diatrizoate compounds, the sodium salt and the meglumine salt, are often mixed to reach a compromise between toxicity and viscosity (10).
Clotting has been reported when blood remains in contact with syringes containing nonionic contrast media. It has been observed that nonionic iodinated contrast media cause this problem less frequently in vitro than ionic contrast media. Meticulous intravascular administration technique is required to minimize thromboembolic events, particularly during angiographic procedures (14).
Respiratory effects include milder symptoms (coughing, laryngitis, rhinitis) progressing to bronchospasm, dyspnea, and pulmonary edema (14).
Effect of route of administration
The route of administration influences the risk of adverse reactions. Adverse effects associated with oral/rectal administration are limited because gastrointestinal absorption is very poor. Transient diarrhea and abdominal cramping may be reported, especially when large volumes and high concentrations of contrast are given. Injection into a joint for arthrography is commonly associated with transient discomfort, pain, and swelling. Severe pain often results from undue use of pressure in a large-volume injection and is due to the procedure itself, rather than from exposure to the contrast agent. Reactions associated with renal instillation may occasionally include transient proteinuria and, rarely, oliguria or anuria. The intravascular route is associated with more serious adverse events. Localized reactions include minor pain, a sensation of warmth (vasodilation), vein cramping, and thrombophlebitis. Systemic reactions range from mild to severe. Neurological effects can range from mild dizziness, headache, and vertigo to vision disturbances and seizures. More severe neurological reactions are seen with cerebral arteriography procedures. Cardiovascular adverse effects include angina, hypotension, and arrhythmias. The effects of contrast agents on calcium ions may play a larger role than osmolality in cardiac adverse effects due to the ability of ionic contrast agents to reduce the availability of extracellular calcium to the myocardium. These calcium decreases have been associated with adverse cardiovascular effects (14).
Nonanaphylactoid, anaphylactoid, and delayed adverse reactions
Three categories of adverse reactions are associated with iodinated contrast agents: nonanaphylactoid, anaphylactoid, and delayed.
Common nonanaphylactoid reactions are usually self-limiting and include nausea, vomiting, diarrhea, headache, and dizziness. Transient diarrhea and abdominal cramping may be reported if administration is by the oral or rectal route— especially when high concentrations and large volumes of contrast are administered. One common complaint during intravenous administration is discomfort (pain/warmth sensation) at the injection site. Less common, but severe, reactions include cardiac arrhythmias, pulmonary edema, seizure, and renal failure (8, 14).
Although a contrast agent reaction may resemble an anaphylactic reaction, the term “anaphylactoid” is assigned because contrast reactions do not have a classic anaphylactic presentation. The reaction is not caused by an immunoglobulin E–mediated immune response. A patient can experience one of these reactions the first time they are exposed to a contrast agent. This is unlike the classic anaphylactic reactions that require prior exposure to the antigen and a buildup of immunity. Anaphylactoid reactions include urticaria, facial and laryngeal edema, bronchospasm, and circulatory collapse (8, 14). An estimated 5% of patients will experience some type of anaphylactoid response, with a predicted 1 in 40,000 fatality rate (10).
Most adverse reactions to injectable contrast appear within 1 to 3 minutes after the start of injection, but delayed reactions may also occur. Delayed reactions may occur up to 6 hours after exposure to contrast and include fever, chills, rash, pruritus, flushing, arthralgias, nausea and vomiting, and headache (2, 8, 14). Of interest, some studies have reported that late allergic skin reactions may be more commonly associated with the administration of an iso-osmolar contrast agent (12). Infrequently, “iodism” (salivary gland swelling) from organic iodinated compounds may appear up to 2 days after exposure; it subsides by the sixth day (14).
Risk factors for adverse events
Risk factors for adverse events include a history of major allergies, asthma, and prior reaction to contrast agent and/or renal impairment. Patients sensitive to iodine or other iodinated contrast agents may be sensitive to these agents also. Patients with a known clinical hypersensitivity (asthma, hay fever, food allergies) have a twofold higher risk than the general population. Patients with a history of previous reaction to iodine per se or a history of previous reaction to a contrast medium are three times more susceptible to adverse reactions than the general population. Sensitivity to contrast does not appear to increase with repeated examinations. A reported seafood “allergy” is not a sufficient contraindication to the use of iodinated contrast material, as 85% of patients will not experience an adverse reaction to iodinated contrast. Suspicion of seafood allergy is often based more on medical myth than fact. For patients who report “allergies” to iodine-containing topical antiseptics (povidone-iodine), there is no evidence that adverse skin reactions to these products are of any specific relevance to administration of intravenous contrast material. These adverse effects are usually local (19, 20).
A positive history of allergies or hypersensitivity does not arbitrarily contraindicate the use of a contrast agent when a diagnostic procedure is considered essential. Precautions should be taken to minimize an anticipated adverse reaction, including limitation of contrast dose, hydration, and premedication (14, 21). For scheduled cases, patients with a history of major allergies, asthma, or a prior reaction to contrast should receive steroids the day before contrast exposure along with diphenhydramine immediately prior to the exam. If the case is urgent, initiation of intravenous steroids 6 hours before the exam (i.e., hydrocortisone 200 mg every 4 hours) is recommended. The use of steroids prior to contrast exposure has been documented to decrease adverse events. The efficacy of diphenhydramine, although commonly used, is not as well documented in the literature (8).
Special precautions are recommended with the intrathecal use of iodinated contrast agents. For scheduled cases, it is recommended that medications that have the potential to lower the seizure threshold should be discontinued at least 48 hours before and for at least 24 hours after the procedure. The final decision should be based upon physician evaluation of potential benefits and potential risks of discontinuation. Most literature reports of major motor seizures were associated with phenothiazine derivatives, monoamine oxidase inhibitors, tricyclic antidepressants, central nervous system stimulants, analeptics, tranquilizers, and antipsychotics. Medications may be resumed 24 hours after the procedure. Patients who are receiving anticonvulsants should be maintained on therapy. Should a seizure occur, intravenous diazepam or phenobarbital sodium is recommended. In patients with a history of seizure activity who are not maintained on anticonvulsant therapy, premedication with barbiturates should be considered. Intrathecal administration of corticosteroids with Omnipaque is contraindicated (14).
Contrast-induced nephropathy
The renal effects of contrast agents have attracted increased attention over the last decade. Contrast-induced nephropathy manifests itself as an abrupt decline in renal function. There is no standard for defining contrast-induced nephropathy. One commonly accepted definition is a relative increase of serum creatinine of at least 25% from baseline or a >0.5 mg/dL rise in serum creatinine within 72 hours of exposure to contrast. Patients commonly remain asymptomatic. The serum creatinine rises within the first 24 hours, peaks 3 to 5 days after exposure, and then returns to baseline within 7 to 10 days. The pathogenesis of contrast damage to the kidneys is unclear and probably has multiple mechanisms. Contrast agents may be directly toxic to the renal tubular cells or possibly mediate renal hemodynamic changes (vasoconstriction in the glomeruli). Red blood cell deformity has also been implicated (8, 19, 22).
The risk of contrast-induced nephropathy is minimal in patients with normal renal function. In patients with preexisting elevated serum creatinine, the effects appear to be related primarily to dose. Risk factors identified by Byrd and Sherman are age 70 or older, dehydration (including diuretic use), preexisting renal insufficiency (serum creatinine >1.5 mg/dL), diabetes mellitus, cardiovascular disease, myeloma, hypertension, and hyperuricemia. Patients with both preexisting renal insufficiency and diabetes are at highest risk (8, 22). The careful selection of a contrast agent and dose limitation may be instrumental in reducing risk. A 2003 study noted a lower incidence of contrast-induced nephropathy with the use of isotonic, nonionic dimers (i.e., iodixanol) compared with nonionic monomers (iohexol) in patients with preexisting elevated serum creatinine (22). The incidence also appears to be associated with the route of administration, appearing more frequently with arterial injections (7%–8%) than with venous injections (2%–5%) (4, 8).
Patients should be diligently screened for preexisting renal dysfunction prior to contrast exposure. The use of serum creatinine has definite limitations as an accurate measure of renal function primarily because renal function is influenced by the patient's gender, muscle mass, nutritional status, and age. Normal serum creatinine levels are maintained until the glomerular filtration rate is reduced to nearly 50%; impaired renal function may exist even when serum creatinine levels appear to be within normal limits. Direct measurement of glomerular filtration rate is impractical. The sensible alternative is to estimate creatinine clearance using the Cockcroft-Gault equation, which incorporates the patient's gender, age, and ideal body weight. Screening patients using an estimated creatinine clearance is a better indication of renal status than a serum creatinine determination (22).
The significance of contrast-induced nephrotoxicity is evidenced by the attention now given to ways to attenuate or prevent renal impairment after contrast exposure. Dose limitation (reduction of total osmotic load) and hydration are two methods to reduce the risk. Urine output should be monitored and should be at least 150 mL/h (23). Several hydration regimens are in current use; however, their beneficial effects remain controversial. One of the common regimens is an isotonic (154 mEq/L) sodium bicarbonate intravenous infusion of 3 mL/kg for the first hour before contrast administration and 1 mL/kg per hour for 6 hours after contrast exposure. The renoprotective effects of bicarbonate are thought to be due to urinary alkalinization, which creates an environment less amenable to the formation of harmful free radicals (8, 24).
Some data support the use of N-acetylcysteine for prevention of contrast-induced nephrotoxicity, although there is no consensus for dosing and some meta-analyses indicate that the benefit is marginal. N-acetylcysteine is frequently prescribed since it is not associated with serious adverse effects and remains inexpensive (23). A 2000 New England Journal of Medicine article promotes either N-acetylcysteine 600 mg orally two times a day beginning the day before exposure or 150 mg/kg per hour intravenously for 30 minutes before exposure, then 50 mg/kg per hour over 4 hours (25). Other protocols call for two doses (600–1200 mg) orally every 12 hours prior to contrast exposure and for two doses after exposure (23). Intravenous fenoldopam mesylate is mentioned in the literature but has not proven to offer significant advantages over saline hydration due to the expense and need for monitoring in a critical care setting (1).
An additional measure to reduce risk is awareness of recent use of iodinated contrast agents. Further contrast studies should be delayed, if possible, to avoid reinsulting the kidneys. The patient's medication profile should be closely monitored. The patient's current medication regimen should be reviewed for potentially nephrotoxic medications. These medications should be used cautiously, placed on hold, or switched to a suitable alternative that is less nephrotoxic until renal function stabilizes. Medications requiring dose adjustment in renal dysfunction should be closely monitored (1).
Dialysis patients are still eligible to receive contrast agents. Contrast agents are not protein-bound and possess relatively low molecular weights so are readily cleared by dialysis. LOCM are the preferred agents for dialysis patients, and the dose should be limited when possible. Unless there is significant underlying cardiac dysfunction (due to risk of direct chemotoxicity on the heart and the blood-brain barrier) or large volumes of contrast are utilized, there is no need for emergent dialysis. The current recommendation is for prompt dialysis after contrast exposure, with short intervals between the next two to three dialysis sessions. Two or three dialysis sessions are required to completely eliminate the contrast (4, 8).
Metformin-associated lactic acidosis
Special consideration should be given to patients receiving metformin, due to their increased risk of developing lactic acidosis. There is no direct drug-to-drug interaction between metformin and iodinated contrast agents. The potential adverse effect is the development of metformin-associated lactic acidosis, significant because it is associated with a mortality rate of up to 50%. Ninety percent of an absorbed dose of metformin is excreted unchanged through the kidneys within the first 24 hours. A severe renal insult from iodinated contrast would inhibit excretion of both metformin and lactic acid. Any factors that decrease metformin excretion, decrease metabolism of lactate (liver dysfunction), or increase blood lactate levels can increase the risk of lactic acidosis. An iodinated contrast insult in the presence of preexisting renal dysfunction is a major consideration. Screening patients for metformin use is a priority; however, current use of metformin is not a contraindication to contrast use. Recommendations indicate that metformin should be discontinued at the time of contrast exposure and withheld for at least 48 hours after the procedure. Metformin should be reinstated only after renal function has been reevaluated and found to be normal (4, 8).
Extravasation
Certain patients are at an increased risk of extravasation. When possible, the patient should be adequately educated to immediately report pain or the sensation of swelling at the injection site. Most patients experience stinging and burning at the site of intravenous injection. The incidence may be reduced if iso-osmotic agents are infused. Patients who are unable to report extravasation symptoms should be closely monitored. Those patients with altered or abnormal circulation in the limb to be injected are at higher risk, as are patients with distal intravenous access sites (e.g., hand, wrist, foot, and ankle). When these situations occur, an LOCM should be considered, since extravasation of LOCM is better tolerated than extravasation of HOCM. Hyperosmolar solutions are more likely to cause tissue damage. An initial acute local inflammatory response peaks in 24 to 48 hours, with edema, erythema, and tenderness as common symptoms. Most patients recover without sequelae; others experience ulceration and tissue necrosis. Acute inflammation may progress to a chronic inflammatory response accompanied by fibrosis and adjacent muscle atrophy (4).
There is no clear consensus regarding the most effective treatment for contrast medium extravasation. Elevation of the affected extremity above the level of the heart is recommended. Elevation will decrease capillary hydrostatic pressure, thereby promoting resorption of the contrast media. There is no clear evidence favoring the use of either warm or cold compresses. Surgical consultation should be considered if extravasation of ≥50 mL of HOCM or ≥100 mL of LOCM has occurred. If the wrist, ankle, or dorsum of the hand is involved, a surgical consultation should be considered at lower volumes. An immediate surgical consultation is indicated if any of the following symptoms occur: increased swelling or pain after 2 to 4 hours, altered tissue perfusion as evidenced by decreased capillary refill at any time after the extravasation has occurred, or a change in sensation in the affected limb, skin ulceration, or blistering (4).
AGENTS FOR MR IMAGING
Less than 30 years have passed since the first human MR image, yet the demand for MR imaging is growing—largely because of the noninvasive nature of the exam and the inherent tissue contrast provided. Although MR imaging is usually considered a branch of radiology, it is based upon a magnetic field, not upon x-rays. It is estimated that nearly half of all MR imaging studies are contrast enhanced using iodinated contrast agents, gadolinium, or other paramagnetic agents (23).
The first MR imaging agents were gadolinium-based. These agents provide enhanced visualization by altering the magnetic properties of nearby hydrogen nuclei, unlike iodinated agents that provide contrast due to their radiopaque properties. Gadolinium agents are a complex formed between a chelating agent higher (4). and a paramagnetic ion (gadolinium3+). When exposed to a magnetic field, gadolinium complexes develop a relatively large magnetism due to unpaired f electrons. In areas where gadolinium agents accumulate, hydrogen nuclei (found in water in the surrounding tissue) are altered, causing an increase in signal intensity of those tissues (5, 26).
Osmolality, ionicity, and viscosity need to be considered when reviewing MR agents. However, these factors are not as replacement significant for the MR agents as they are for other contrast agents since MR requires significantly smaller doses: 15 to 20 mL for MR compounds versus 150 mL for iodinated agents. Because of the smaller administration volume and the decreased osmotic load, the physical characteristics of osmolality and ionicity do not play as significant a role in the comfort and safety of the patient during exposure to the product. Viscosity is also not a significant concern at standard doses and injection rates but may be a limiting factor when small catheters and high-flow-rate applications are involved (8, 9).
There is a common misconception that gadolinium-based agents do not cause con-trast-induced nephrotoxicity. These products are every bit as nephrotoxic as iodinated agents, and the use of gadolinium is not without problems. Nevertheless, with the smaller volume administered—the standard dose is 0.1 mmol/kg (approximately 15–20 mL)—the risk of contrast-induced nephropathy is so low that MR agents are considered virtually nonnephrotoxic. When off-label higher doses (0.3 mmol/kg) are utilized, the total osmotic load and the patient risk increase substantially (8).
Distribution and excretion
Gadolinium-based agents are administered intravenously. The major route of excretion is renal. Over three dialysis sessions, hemodialysis will clear gadolinium-based agents from the system. Gadolinium-based agents do not cross the blood-brain barrier unless it is disrupted or abnormal vascularity allows for penetration (26, 27).
Drug and laboratory test interactions
It is not necessary to discontinue met formin prior to gadolinium-enhanced MR studies when the amount of gadolinium administered is in the usual dose range of 0.1 to 0.3 mmol per kg of body weight. Metformin should be discontinued in large-dose cases, such as angiography or CT scanning, where the risk of renal insult is higher (4).
Gadolinium agents interfere with the laboratory test to determine calcium levels. The most common assay for serum calcium uses a colorimetric assay. Sometimes the effect is so exaggerated that the laboratory reports serious hypocalcemia. This effect is common with higher doses; renal insufficiency increases the risk. Education is essential to avoid the potential for incorrect diagnosis and initiation of inappropriate calcium (8, 9). In addition, transient changes in laboratory tests for serum iron, calcium, copper, and zinc parameters have been observed; however, the significance in unknown (26).
Pregnancy and breast-feeding
All five gadolinium-based contrast agents are classified as pregnancy category C. Optimark product information indicates that nursing should be discontinued and breast milk discarded up to 72 hours after injection. The American College of Radiology Manual on Contrast Media 5.0 (2004) states: “The available data suggests that it is safe for the mother and infant to continue breast-feeding after receiving such an agent.” Ultimately, an informed decision to disrupt breast-feeding should be left up to the mother, who should be assured that this disruption need not last longer than 24 hours (assuming normal renal function) (4, 9).
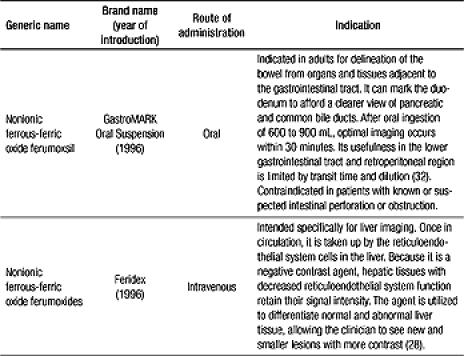
Product overview
Gadolinium-based agents available for MR imaging are summarized in Table 2. Nongadolinium paramagnetic agents are also used in MR imaging (Table 3). Information from the most current product inserts supersedes all other information.
Table 2.
Gadolinium-based agents used in magnetic resonance imaging
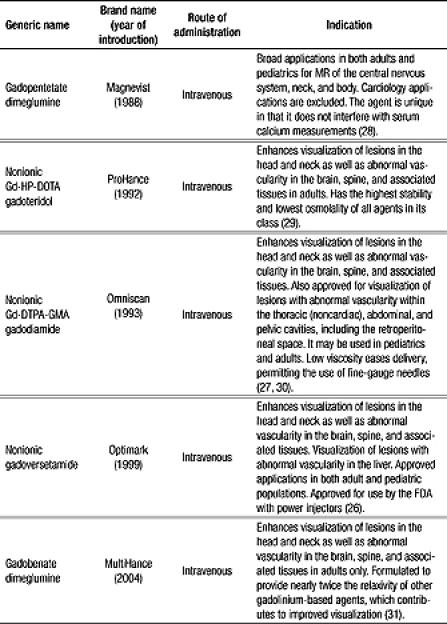
Table 3.
Other paramagnetic agents used in magnetic resonance imaging
ADVERSE REACTIONS TO GADOLINIUM AGENTS
Gadolinium agents tend to have a lower rate of adverse reactions than iodinated contrast agents. Risk factors include a strong history of allergies, a previous reaction to iodinated contrast, or a previous reaction to gadolinium. At-risk patients can be premedicated with the same protocol used for iodinated contrast: hydration, antihistamines, and steroids (8). Most (95.8%) adverse effects are mild and self-limiting. Headache, vasodilation, and taste perversion have an occurrence of <10%; dizziness, nausea, and paresthesia may also occur infrequently. Allergic reactions to gadolinium agents are very rare (<0.1%) (26). The enhancement of magnetism by gadolinium may potentiate sickle erythrocyte alignment, resulting in vaso-occlusive complications in vivo (26).
Nephrogenic fibrosing dermopathy/nephrogenic systemic fibrosis
In 1997, nephrogenic fibrosing dermopathy (NFD) was described—a scleredema-like condition reported in renal failure patients who received gadolinium contrast. Fibrotic changes occur, such as thickening, induration, and tightening of the skin, which could potentially progress to joint contractures and decreased mobility. In June 2006, the FDA issued an alert describing the development of nephrogenic systemic fibrosis (NSF). It was discovered that these same fibrogenic changes could also occur within internal organs, especially lung and heart tissue. This condition was primarily seen with gadodiamide but has occurred with other gadolinium agents.
Since no causal link exists between NFD/NSF and gadolinium, another cofactor may be involved, most likely a major surgery, vascular procedure, or thrombotic event. It is suspected that these events could result in an inflammatory milieu with high levels of circulating fibrocytes. Circulating fibrocytes normally participate in wound healing and scar formation in the setting of tissue injury. It is speculated that free gadolinium may induce the circulating fibrocytes to initiate the fibrotic changes characteristic of NSF. The fibrocytes appear to induce fibrosis in normal tissue in the setting of NSF.
Not every patient with renal failure develops NFD/NSF. In December 2006, the FDA recommended avoiding gadolinium-based agents in patients with moderate to severe renal disease, limiting the dose, and avoiding repeat contrast exposure before the serum creatinine had returned to baseline (23, 33).
References
- 1.Barrs TJ. Establishing safeguards for the use of imaging-related drugs. Am J Health Syst Pharm. 2002;59(15):1449–1453. doi: 10.1093/ajhp/59.15.1449. [DOI] [PubMed] [Google Scholar]
- 2.Borgsdorf LR, et al., editors. Drug Facts and Comparisons 2006. 60th ed. St. Louis, MO: Wolters Kluwer Health; 2005. pp. 2647–2654. [Google Scholar]
- 3.American Society of Health-System Pharmacists, Inc. Barium sulfate [fact sheet in the Med Master Patient Drug Information database] Available at http://www.nlm.nih.gov/medlineplus/druginfo/medmaster/a606010.html; accessed July 4, 2007.
- 4.ACR Committee on Drugs and Contrast Media . Manual on Contrast Media, Version 5.0. Reston, VA: American College of Radiology; 2004. pp. 4–68. [Google Scholar]
- 5.Borgsdorf LR et al, eds. Drug Facts and Comparisons, 61st ed. St. Louis, MO: Wolters Kluwer Health: 2922-2930.
- 6.Grant KL, Camamo JM. Adverse events and cost savings three years after implementation of guidelines for outpatient contrast-agent use. Am J Health Syst Pharm. 1997;54(12):1395–1401. doi: 10.1093/ajhp/54.12.1395. [DOI] [PubMed] [Google Scholar]
- 7.Institute for Safe Medication Practices. Intrathecal injection of ionic contrast media may be fatal. Medication Safety Alert, November 27, 2003. Available at http://www.ismp.org/Newsletters/acutecare/articles/20031127.asp?ptr=y; accessed July 15, 2007.
- 8.Brown JJ. Implementing medication management standards for contrast media Contrast agents-an overview. Presented at the 41st ASHP Mid-Year Clinical Meeting in Anaheim, California, December 3, 2006. Available at http://symposia.ashp.org/contrast; accessed July 4, 2007.
- 9.Lin SP, Brown JJ. MR contrast agents: physical and pharmacologic basics. J Magn Reson Imaging. 2007;25(5):884–899. doi: 10.1002/jmri.20955. [DOI] [PubMed] [Google Scholar]
- 10.Thomsen HS, Morcos SK. Radiographic contrast media. BJU Int. 2000;86(Suppl 1):1–10. doi: 10.1046/j.1464-410x.2000.00586.x. [DOI] [PubMed] [Google Scholar]
- 11.Lin J, Bonventre JV. Prevention of radiocontrast nephropathy. Curr Opin Nephrol Hypertens. 2005;14(2):105–110. doi: 10.1097/00041552-200503000-00004. [DOI] [PubMed] [Google Scholar]
- 12.Becker C. The impact of new CT technology on clinical practice. C2I2: Controversies and Consensus in Imaging and Intervention. 2005;3(1):4–8. Available at http://www.c2i2.org/vol_iii_issue_1/the_impact_of_new_CT_technology_full_text.asp; accessed July 4, 2007. [Google Scholar]
- 13.Reddinger WL Jr. Contrast Media November 1996. Available at http://www.e-radiography.net/contrast_media/CT_contrast_media.pdf; accessed July 14, 2007.
- 14.Omnipaque (iohexol) injection [product insert] Princeton, NJ: GE Healthcare, May 2006.
- 15.Isovue-M 200 (iopamidol injection 41%); Isovue-M 300 (iopamidol injection 41%) [prescribing information]. Princeton, NJ: Bracco Diagnostics Inc, September 2005.
- 16.Visipaque (iodixanol) injection [prescribing information] Princeton, NJ: GE Healthcare, May 2006.
- 17.Hypaque sodium (Diatrizoate Sodium) powder, for solution [prescribing information] Princeton, NJ: Amersham Health, Inc, August 2004.
- 18.Cysto-Conray II (iothalamate meglumine) injection [prescribing information] St. Louis, MO: Mallinckrodt, March 2002.
- 19.Coakley FV, Panicek DM. Iodine allergy: an oyster without a pearl? AJR Am J Roentgenol. 1997;169(4):951–952. doi: 10.2214/ajr.169.4.9308442. [DOI] [PubMed] [Google Scholar]
- 20.van Ketel WG, van den Berg WH. Sensitization to povidone-iodine. Dermatol Clin. 1990;8(1):107–109. [PubMed] [Google Scholar]
- 21.Hypaque sodium (diatrizoate sodium) injection, solution [prescribing information] Princeton, NJ: Amersham Health Inc, April 2006. Available at http://dailymed.nlm.nih.gov/dailymed/fdaDrugXsl.cfm?id=997; accessed July 14, 2007.
- 22.Contrast Media Osmolality: How Much Does It Matter? GE Healthcare, Ltd, February 2006:3
- 23.Prevention of contrast-induced nephropathy Pharmacist's Letter/Prescriber's Letter. 2007;23(3):230–309. [Google Scholar]
- 24.Merten GJ, Burgess WP, Gray LV, Holleman JH, Roush TS, Kowalchuk GJ, Bersin RM, Van Moore A, Simonton CA, 3rd, Rittase RA, Norton HJ, Kennedy TP. Prevention of contrast-induced nephropathy with sodium bicarbonate: a randomized controlled trial. JAMA. 2004;291(19):2328–2334. doi: 10.1001/jama.291.19.2328. [DOI] [PubMed] [Google Scholar]
- 25.Tepel M, van der Giet M, Schwarzfeld C, Laufer U, Liermann D, Zidek W. Prevention of radiographic-contrast-agent-induced reductions in renal function by acetylcysteine. N Engl J Med. 2000;343(3):180–184. doi: 10.1056/NEJM200007203430304. [DOI] [PubMed] [Google Scholar]
- 26.OptiMARK (gadoversetamide) injection [prescribing information] St. Louis, MO: Mallinckrodt, January 2003.
- 27.Omniscan (gadodiamide) injection [prescribing information] Princeton, NJ: GE Healthcare, June 2007.
- 28.DiIulio R. Secret agents: a product round-up of contrast agents on the market today. Medical Imaging May 2007. Available at http://www.medicalimagingmag.com/issues/articles/2007-05_06.asp; accessed July 14, 2007.
- 29.ProHance (gadoteridol) [prescribing information] Princeton, NJ: Bracco Diagnostics, Inc, May 2007.
- 30.Schwerin E. Breast MRI contrast agent: gadolinium Breast MRI Web Site, 1999. Available at http://www.mrsc.ucsf.edu/breast/gadolinium.html; accessed July 4, 2007.
- 31.MultiHance (gadobenate dimeglumine) injection [prescribing information] Princeton, NJ: Bracco Diagnostics, May 2007.
- 32.GastroMARK (ferumoxsil, oral suspension) [prescribing information] St. Louis, MO: Mallinckrodt, January 2003.
- 33.US Food and Drug Administration. Gadolinium-containing contrast agents for magnetic resonance imaging (MRI): Omniscan, OptiMARK, Magnevist, ProHance, and MultiHance. FDA Alert, December 22, 2006. Available at http://www.fda.gov/medwatch/safety/2006/safety06.htm#Gadolinium; accessed July 4, 2007.


