Abstract
Aims
To identify drug usage/withdrawal in surgical patients and the relative risk this imposes on postoperative surgical complications.
Methods
A prospective survey of patients' medicines, oral intake (food/fluids/ medicines) and postoperative complications was carried out in the General Surgical Unit, Dunedin Hospital, Dunedin, New Zealand.
Results
One thousand and twenty-five general surgical patients aged ≥ 16 years, were entered into the study. Half of the patients were taking medicines unrelated to surgery. On average these patients received 9 different drugs (range 1–47) from a selection of 251, of which 21% were released in the last 10 years. The mean number of these drugs taken increased with age, vascular surgery and other major procedures. The majority of patients (53%) were taking drugs for cardiovascular problems. Only 8% of admissions were on the drugs more traditionally recognized to be of importance to the surgery, i.e. steroids and diabetic therapy. With respect to risk, taking a drug unrelated to surgery was associated with an increased relative risk of a postoperative complication by 2.7 (95% C.I. 1.76–4.04) compared with those who were not taking any drug. Cardiovascular drugs contributed significantly to this risk; when they were excluded from analysis, the risk dropped to 1.8 (95% C.I. 1.14–2.93). Death may be more common in those taking ACE inhibitors. Drug withdrawal and complications were analysed and as the time without medicines increased (range 1–42 days) so did the complication rate (χ2 = 14.7, DF = 2, P = 0.007). Of those patients who were taking a cardiovascular medicine and were without their normal medicines for a period of time postoperatively, 12% suffered a cardiac complication.
Conclusions
Many patients admitted to a general surgical ward, are taking medicines unrelated to surgery. Drug therapy unrelated to surgery is a useful predictor for increased postoperative complications and one for which preventive action can be taken. This study provides evidence that withdrawal of regular medicines may add significant risk to the surgery and further complicate outcome. The longer patients were without their regular medicines the more nonsurgical complications they suffered. Reintroduction of patients' regular medicines early in their postoperative course may decrease morbidity and mortality in-patients.
Keywords: complications, drug therapy, drug withdrawal, surgical patients
Introduction
Advances in both surgical and anaesthetic techniques have resulted in more elderly patients undergoing operative procedures and it is projected that in the next 30 years the number of noncardiac surgery operations will increase by 50% as the population over 65 years increases [1]. Many of these people are on drugs and those drugs often improve their general well being at presentation for surgery and this may allow them to be considered for surgery whereas in the past, they might not have been.
Four previous studies have surveyed drug use in surgical patients and up to 44% of patients may be taking medicines unrelated to surgery on admission to hospital, but little is known about the types of drugs and their impact on peri-operative events. There is a need to investigate this impact because of the large numbers of patients presenting for general surgery who are taking potent drugs and in light of the warnings and perceived dangers of their abrupt withdrawal [6–13]. Previous studies have not addressed the implication of the withdrawal of these drugs, nor has there been a systematic/prospective study of the impact of drug withdrawal. When going forward for surgery, the withdrawal of these critical drugs may have significant adverse impact on morbidity. This applies in particular to cardiovascular (CVS) and central nervous system (CNS) drugs and may be of greatest relevance in general surgical patients where the need to be without oral intake is more common.
The aims of this prospective study were to: (i) identify the drug usage profile of a general surgical population (ii) identify those patients at greatest risk of polypharmacy and quantify the relative importance of those drugs to surgical outcome (iii) identify the frequency and duration of drug withdrawal and relate this to the postoperative outcome.
Methods
The General Surgical Unit at Dunedin Hospital admits all adult patients (>16 years) who have a general surgical problem. Over a 7 month period, all consecutive patients admitted for either elective or emergency surgery, were eligible for inclusion, whether or not they were taking drugs prior to their admission. There were no exclusion criteria. Day-stay surgical patients (25% of surgical procedures in this Unit) were not included in this study unless they were subsequently admitted to the General Surgical Unit as in-patients. Ethical approval was obtained from the institution's Ethics Committee which waived the need for written informed consent from each patient. Patient and admission identification was by the unique national patient hospital number and the admission date. As some patients were admitted more than once to the Surgical Unit during the period of the study, calculations were based on admissions rather than patients.
Data were collected on a daily basis by JMK. The sources were: patients, relatives/friends of patients, medical and nursing staff, general practitioners, general practitioners, admission letters, drug charts, medical and nursing notes. Extensive cross checking of the sources listed was carried out to ensure complete records were obtained. Four separate sets of data were collected: the medicine history, the oral intake history, the clinical information, and surgical complications.
The medicine history recorded the name of each medicine, route of administration, stop and start dates. Each medicine was assigned an eight-digit drug code based on the American Hospital Formulary Service (AHFS) Pharmacological Therapeutic Classification coding system, modified for local usage. Medicines were also distinguished by whether they were used as part of the patients' regular therapies or part of their surgical care. Regular medicine was defined according to the definition used by Wyld & Nimmo [3], i.e. the patient had been taking the drug for more than 2 weeks prior to admission to hospital.
The oral intake record identified the time periods during which the patients were strictly nil by mouth for food and fluids (nbm), and when drugs were strictly nil by mouth (ndm), the timing of which were entirely at the discretion of each of the clinical teams. It also identified if drugs were continued and if so, the alternative routes used.
The clinical record was a consultant surgeon-verified summary from the Surgical Audit. This included patient demographics, presenting pathology, the duration, type, and magnitude of the operative procedure, wound classification, and complications. Operative procedures were categorized into four groups according to the magnitude of the surgery (Table 1).
Table 1.
Operative procedures categorized according to the magnitude of the surgery.
| Major 1 | Abdominal aortic aneurysm repair, panproctocolectomy,liver resection |
| Major 2 | Right hemicolectomy, sigmoidectomy,thyroidectomy, mastectomy |
| Intermediate | Appendicetomy, hernia repair, varicoseveins surgery |
| Minor | Angiography, excision of moles, colonoscopy |
Complications were derived from two sources: the Surgical Audit and from case studies. The Surgical Audit is medical staff driven and all complications of sufficient clinical relevance are recorded. These complications were recorded independently of this drug study and this database was used in the analysis of complications. These complications are comprehensive and cover minor complications to major events (Table 2). Complications include both those related to the surgical procedure and those of a nonsurgical nature (Table 3). Complications are coded both as a group and individually, allowing for instance, all cardiac complications as a group to be analysed, or specific complications such as cardiac dysrhythmias to be determined. In the analysis, complications were divided into the two categories: (a) those related specifically to the surgical procedure (b) nonsurgical/clinical complications and which may have been attributable to drug withdrawal.
Table 2.
Examples of complication categories and specific complications.
| Examples of complication | Examples of specific complication |
|---|---|
| Categories | |
| Death | Septicaemic, cardiac, vascular, respiratory, renal, advanced cancer death |
| Cardiac | Endocarditis, myocardial infarction, myocardial ischaemia, cardiac dysrhythmia, congestive heart failure, stroke |
| Wound | Infection, haematoma/seroma, dehiscence, incisional hernia |
| Renal | Urinary tract infection, oilguria/renal failure, urinary retention |
| Pulmonary | Chest infection/bronchopneumonia, consolidation/atelectasis, pulmonary embolus, pulmonary oedema, pneumothorax |
| Haematological | Haemorrhage, septicaemia, deep vein thrombosis, thrombophebilits, disseminated intravascular coagulopathy |
| Central nervous system | Confusion, depression, delerium tremens, psychiatric disorder unspecified |
| Gastrointestinal | Diarrhoea, peptic ulcer(perforated/haemorrhage), jaundice, noninfective diarrhoea, faecal impaction/constipation |
| Technical | Catheter-related sepsis, anaesthetic complications, nerve damage, vascular damage, recurrence/incomplete excision |
Table 3.
Examples of surgical and non-surgical complications.
| Examples of surgical complications |
| Haematoma/seroma, dehiscence, incisional hernia catheter-related sepsis, anaesthetic complications, nerve damage, vascular damage, recurrence/incomplete excision, anastomotic leak, ileus/gastric dilatation, bile leak, infection of graft, acute thombosis/embolus/gangrene |
| Examples of non-surgical complications |
| Septicaemic death, advanced cancer death, myocardial infarction, congestive heart failure, urinary tract infection, oliguria/renal failure, consolidation/atelectasis, pulmonary embolus, deep vein thrombosis, thrombophebilits, confusion, depression infective diarrhoea, jaundice, faecal impaction/constipation |
Case studies detailing incidents in which complications thought to be related specifically to drug withdrawal were recorded. To be documented, these studies had to fulfil the following criteria: medical attention was required for the complication, the patient needed alternative treatment to their normal medications or normal medications were reinstated to control their condition, and any other reasons responsible for the complication, other than drug use/withdrawal, such as inadequate pain control, could be excluded.
Data analysis
Analysis was undertaken using the package SPSS-X (Statistical Package for Social Scientists) for tabulations and GLIM (Generalized Linear Interactive Models) for logistic regression analysis. All files were validated for data completion. Initially univariate analyses for association between the various complications and possible risk factors were performed with two by two contingency tables using SPSS-X. These tests were conducted without regard for confounding factors such as age, duration of hospital stay, time the patients were without their normal medications by the oral route. For subsequent logistic regression analysis, GLIM was used. By using this method of analysis, the issues of confounding and synergism were taken into account.
Results
There were 1027 admissions to the General Surgical Unit. Two patients refused the invitation to participate, leaving 1025 admissions for analysis. The age and gender distribution of the patients is shown in Figure 1. When compared with the New Zealand population, where the group older than 60 years of age comprises 20% of the population, 50% of the admissions were older than 60 years of age. The admissions were categorized according to their primary presenting pathology. These were: – ‘vascular’ (17%), ‘cancer’ (18%), ‘inflammatory/infection’ (22%), ‘others’ (22%) and ‘no operation’ (18%). Classification of the operative category and age is shown in Table 4. The average day stay was 9.92 days and the median day stay 6.2 days (range < 1–124 days) and the older the age group, the longer the average day stay was in hospital
Figure 1.
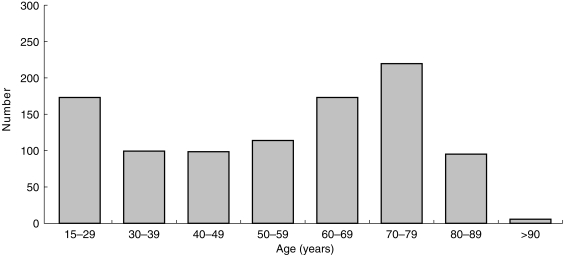
Age distribution of admissions.
Table 4.
Age and operative category distribution of admissions.
| Operation category | |||||
|---|---|---|---|---|---|
| Age group | No operation (n = 234) | Major 1 (n = 89) | Major 2 (n = 295) | Intermediate (n = 281) | Minor (n = 126) |
| < 60 years | 51.4% | 18.7% | 40.7% | 65.9% | 50.6% |
| 60–69 years | 15.0% | 33.3% | 25.1% | 12.1% | 23.6% |
| ≥ 70 years | 33.6% | 48.0% | 34.2% | 22.0% | 25.8% |
In total, 286 different drugs (251 excluding anaesthetic agents) were administered to admissions whilst they were in hospital by a variable number of routes (21% of these drugs were released in the last 10 years). These included regular medicines for conditions unrelated to their surgical conditions, as well as medicines used in the peri-operative period (Figure 2). Only a small group of patients (3%) did not receive any drugs. The majority of admissions received more than one drug (all drugs including anaesthetic drugs; average = 9.38 drugs per admission; range 1–47) whilst in-patients. The mean and median number of drugs per operation category is shown in Table 5.
Figure 2.
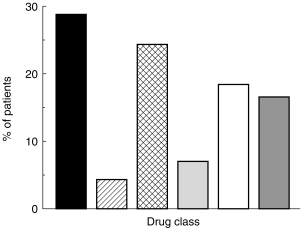
Percentage of patients taking medicines unrelated to their surgery according to major therapeutic group (▪, CVS;  , diuretic;
, diuretic;  , CNS;
, CNS;  , CNS/CVS; □, GI;
, CNS/CVS; □, GI;  , other).
, other).
Table 5.
Mean and median number of drugs per patient, both related and unrelated to surgery per operation category.
| Operation category | |||||
|---|---|---|---|---|---|
| Age group | No operation (n = 334) | Major 1 (n = 85) | Major 2 (n = 289) | Intermediate (n = 264) | Minor (n = 89) |
| Mean | 4.6 | 15.3 | 12.1 | 10.4 | 76.2 |
| Median | 5.4 | 15.5 | 14.0 | 11.3 | 7.6 |
Nearly 50 percent (49%) of admissions were taking medicines unrelated to the surgical admission. The mean number of these drugs (2.4 ± 2.8; mean ± s.d) increased with age (Figure 3), and was greatest for in-patients admitted for vascular surgery (4.0 ± 2.7; P < 0.05) and those undergoing major procedures. Of those patients taking drugs unrelated to surgery the majority (48%) were on drugs for cardiovascular problems (diuretic 4%, cardiovascular 24%, and both 18%) and more than 90% of these admissions were taking 2 or more of these type of drugs (mean 2.4; range 1–7). The most common drugs in this group were frusemide, β-adrenoceptor blockers, and angiotensin converting enzyme (ACE) inhibitors. In addition 45% (n = 224) were taking the CNS drugs, e.g. tranquillisers, antidepressants or hypnosedatives. The other large group comprised drugs acting on the gastrointestinal system (34%) in particular laxatives, H2-receptor antagonists, and antiemetics. Other drugs included anti- asthmatics, antineoplastics and different hormone replacements. Only 8% of admissions were on the drugs more traditionally recognized to be of importance to the surgical team, i.e. steroids and diabetic therapy.
Figure 3.
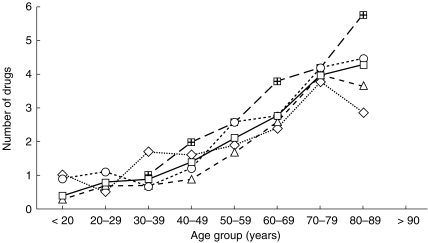
Mean number of drugs unrelated to the surgical admission in each age group according to the specified disease categories. (vascular ( ), n = 167; neoplasms (◊), n = 207; inflammatory (▵), n = 228; others (○) n = 225; all admissions (□)).
), n = 167; neoplasms (◊), n = 207; inflammatory (▵), n = 228; others (○) n = 225; all admissions (□)).
Two hundred and thirty-five patients had 373 complications (Figure 4). Only patients who underwent an operation were included in the analysis. In evaluating the complications, two questions were asked. The first question was, ‘were the drugs unrelated to surgery a predictive factor for developing postoperative complications?’ The second question, was ‘did acute withdrawal of a patient's regular drug therapy made a contribution to their postoperative complications?’ Both univariate and logistic regression analyses were undertaken. Univariate analysis showed digoxin and the calcium antagonists to be associated both with cardiac complications (P < 0.00015) and with deaths (P < 0.006). ACE inhibitors were associated with renal, cardiac complications and deaths (P < 0.004). Death may be more common in those taking ACE inhibitors, when compared with those takingβ-adrenoceptor blockers (Table 6). There were eight serious postoperative complications directly attributable to being on the drugs unrelated to the surgery and these were in patients taking particular drugs which are used less frequently.
Figure 4.
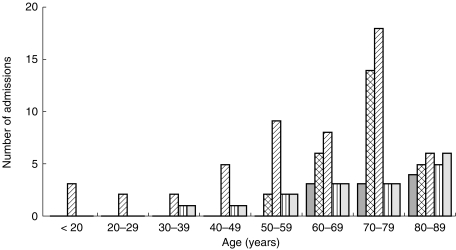
Distribution of complications throughout the age groups ( , death;
, death;  , cardiac;
, cardiac;  , wound;
, wound;  , renal;
, renal;  , central nervous system).
, central nervous system).
Table 6.
Number of deaths occurring among patients admitted to hospital taking either ACE inhibitors or (-adrenoceptor blockers).
| Drug group | Number of patients | Number of deaths |
|---|---|---|
| ACE inhibitors | 79 | 5 |
| β-adrenoceptor blockers | 85 | 0 |
| Whole study | 1025 | 11 |
The question of confounding by factors such as age, magnitude of operation, duration of operation, was taken into account by the use of logistic regression analysis. In using logistic regression analysis, for each independent variable (cardiovascular drug use, age, and duration of operation, the risk relates to a reference group of patients with no cardiovascular drug use, age less than 60 years and duration of operation under 1 h). Logistic regression analysis showed the risk factors for developing any of the clinical complications in order of significance to be: the duration of operation, being on a cardiovascular or CNS drug, postoperatively being without drugs by the oral route >24 h, and the age of the patient. Significant interactions reflect confounding among factors. In the analysis, had there been other significant interactions terms these would have been included. With respect to risk, taking a drug unrelated to surgery was associated with an increased relative risk of a postoperative complication by 2.7 (95% CI 1.76–4.04) compared with those who were not taking any drug. Cardiovascular drugs contributed significantly to this risk. When they were excluded from analysis, the risk dropped to 1.8 (95% CI 1.14–2.93).
Logistic regression analysis was used to determine if acute withdrawal of a patient's regular drug therapy made a contribution to their postoperative complications. There was a significant association between the time the patients were without medicine and the duration of operations (χ2 = 81.6, DF = 6, P < 0.0001), and the operation category (χ2 = 349.7, DF = 8, P < 0.0001). As the time without medicines increased, so did the complication rate (Figure 5) and this was significant (χ2 = 14.7, DF = 2, P = 0.007). Of the patients taking a cardiovascular medicine (n = 127; 12%) and who had drug withdrawal for greater than one day (‘ndm’ for any period of time) 14% (n = 18) suffered a cardiac complication. Of the patients taking a cardiovascular medicine, when they were ‘ndm’ for < 2 days (n = 90) the complication rate for any nonsurgical complication was 12%; of those patients who were taking a cardiovascular medicine and were ‘ndm’ for (2 days (n = 37) the complication rate for any nonsurgical complication was 27% (n = 10) and this approached significance (P = 0.07).
Figure 5.
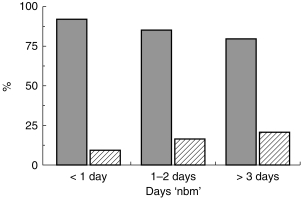
Percentage of admissions with no complications and complications stratified by number of days without oral medicines (no complications  , n = 457; complications
, n = 457; complications  , n = 227 (χ2= 14.7, DF = 2, P = 0.007).
, n = 227 (χ2= 14.7, DF = 2, P = 0.007).
Case studies which had fulfilled the defined criteria confirmed these observations. Thirty-four (5%) of the patients who had undergone surgery suffered postoperative complications directly attributable to withdrawal of their regular medicines (Table 7). These case studies covered patients receiving a variety of classes of drugs, ranging from cardiovascular medicines to treatment of Parkinson's disease. Several patients who were admitted taking cardiovascular drugs and who had undergone major surgery suffered severe hypertension postoperatively, other patients went into congestive heart failure and some suffered life-threatening dysrhythmias. Some of these cases necessitated considerable medical staff attention and time. Clinical depression upon acute withdrawal of regular antidepressants occurred in four patients and affected their postoperative mobilization and recovery. One case of an acute psychosis consumed considerable resources in investigations, family disruption/feuds and lawyers until it was realized this was due to inadvertent benzodiazepine withdrawal. A day after receiving normal nightly nitrazepam dose, the patient was fully lucid and orientated and able to give a full account of her history and events. She had normal mental status and was in full control of her faculties. Withdrawal of usual Sinamet from two patients in the peri-operative period resulted in immobility and chest complications due to Parkinson's disease. In all these cases, all other causes were excluded and each situation resolved as soon as the patients were started back on their admission drugs.
Table 7.
Examples of complications which resolved on re-institution of preadmission medicines.
| Diagnosis/age | Drug withdrawn | Symptoms | Consequences | Resolution |
|---|---|---|---|---|
| Breast cancer with secondary deposits | ||||
| 63 years | Nitrazepam | Psychotic, confused, drowsy | ? cerebral mets, CT scan, lumbar puncture, power of attornery withdrawn permanently, lawyers involved, family rifts | Diazepam started once nitrazepam withdrawal recognized as cause of symptoms, lucid within 12 h. |
| Abdominal aortic aneurysm repair | ||||
| 75 years | Sinemet | Movements difficult during this time | Mobilization delayed and chest complications | Symptoms resolved once Sinemet re-introduced day 9 postop. |
| Aorto-bi-iliac graft | ||||
| 85 years | Doxepin | Tearful, anxious and depressed | Mobilization delayed | Doxepin reintroduced 23 days later and patient much improved |
| Caecopexy | ||||
| 66 years | Sinemet | Movements difficult during this time | Mobilization delayed and chest complications | Symptoms resolved once Sinemet re-introduced. |
| Aorto-bi-iliac graft | ||||
| 63 years | Sotalol, lisinopril | Day 1 postop pulmonary oedema and systolic BP > 200 mmHg despite adequate pain control and other causes eliminated, day 6 started sips, and hypertensive again | Needed prn nifedipine sl to control hypertension | Admission meds re-instated day 6 and became normotensive. |
| Left hemicolectomy/anterior resection | ||||
| 67 years | Captopril, pindolol, bumetanide | Day 2 systolic BP > 200 mmHg despite adequate pain control and other causes eliminated. Also BP became quite labile. Day 7 bp 175/90 mmHg | Intravenous metoprolol given until day 5 and nifedipine sl until day 8 | Captopril restarted day 8, became normotensive |
| Abdominoperineal resection | ||||
| 69 years | Viskaldix | Steady rise in BP. Day 4190/100 mmHg + headache | Still ‘nbm’ but Visaldix recommenced | Normotensive day 4 and fluids introduced day 6. |
| Transverse colectomy | ||||
| 64 years | Cyclopenthiazide, diltiazem | |||
| Day 3 BP 200/130 mmHg | Pain from concurrent osteoarthritis Mobilization a problem because of NSAID withheld | Needed 3 dose of nipedipine to become normotensive Restarted on diltiazem and became normotensive | ||
| Abdominoperineal resection | ||||
| 67 years | Enalapril, nadolol | Hypertensive, 190/120 mmHg (Day 1) 200/116 mmHg (Day 2) 230/120 mmHg (Day 3) | Needed prn nifedipine sl to control hypertension | Admission meds re-instated day 3 and became normotensive. |
| Anterior resection | ||||
| 65 years | Enalapril | Day 3 hypertensive 190/110 mmHg | Re-started admission meds | Admission meds re-instated day 3 and became normotensive |
Discussion
Surgical patients often develop complications peri-operatively and this study asked two questions central to this issue: ‘were the drugs unrelated to surgery a predictive factor for developing postoperative complications?’ and ‘did acute withdrawal of a patient's regular drug therapy make a contribution to their postoperative complications?’ This study also identified the drug usage profile of a general surgical undergoing a comprehensive range of general surgical procedures. Nearly 50% of patients were admitted taking medicines unrelated to the surgery. This is higher than the 24–44% observed in the other studies, the last of which was published in 1991. Half the patients were older than 60 years and the older the patient, the more drugs they were taking, irrespective of type of surgery they underwent. The more major the surgery, the more comorbid disease patients have, as evidenced from their concurrent (often multiple) drug therapy. This observation is not unexpected as it mirrors the pattern in an ageing society as comorbid diseases increase with age, and with the national prescription patterns for the elderly. As in-patients, almost all receive drugs, in addition to those which they are already taking, the range of which encompasses almost the entire pharmacopoeia. Very few patients were taking drugs which surgeons immediately recognize as posing problems for management in the peri-operative period.
Numerous other studies of prognostic indicators for surgical outcomes have been reported none of which has considered drug therapy. In this study, we would contend that admission drugs are a predictive factor for developing postoperative complications as they mask the predisposing frailty of many of these patients. Univariate analysis showed patients already taking cardiovascular drugs to have more cardiac complications postoperatively and logistic regression analysis confirmed this. This type of analysis took into account that older patients were more likely to be taking drugs and have more major surgery, but still demonstrated that drugs are having an independent effect. Clearly it is not necessarily the drug per se that increases the risk of postoperative complications, but it is clear that being on a drug unrelated to the surgery highlights a risk. This may be by simple association, by reflecting severity of comorbidity or more directly because of the patient's need of the drugs to withstand the stresses of the postoperative period of an operation.
ASA (American Society of Anaesthesiologists) groupings have been shown to correlate reasonably well with postoperative complications. Patients in a higher ASA category might not be considered for some surgical procedures except that their drug therapy for underlying conditions has lowered their ASA category. This artificially lowers risk, and permits the patient to be considered for surgery. Discontinuing these drugs at the time of surgery may unmask their true ASA category and greater operative risk. While taking cardiovascular medicines was almost an inevitable characteristic for those requiring vascular surgery this group of vascular patients accounted for fewer than 20% of admissions who were taking a cardiovascular drug. Clearly cardiovascular disease is prevalent amongst a much wider group of admissions including those requiring cancer surgery. Logistic regression analysis showed that those patients who were admitted already taking medicines were at a greater than two fold risk of developing a postoperative clinical complication, when compared with their drug-free counterparts. That risk dropped if cardiovascular drugs were excluded from the analysis.
For the second question, ‘did acute withdrawal of a patient's regular drug therapy make a contribution to their postoperative complications?’ we would contend that once the predisposing frailty of the patients is unmasked by drug withdrawal, there is an increase in nonsurgical postoperative complications. The stress of the operation superimposes on the underlying pathology, which is now without its normal pharmacological support, thus leading to more complications. While many authors caution against the abrupt withdrawal of medicines, especially cardiovascular and central nervous system drugs, reports also indicate acute withdrawal problems are more likely to occur after about 2 days of stopping of the drug [26–28]. It is acknowledged that withdrawal of some drugs such as sulphonylureas is appropriate or even mandatory peri-operatively and that common sense may require stopping diuretics in a dehydrated patient. However, for the vast majority of drugs this is not so. In this study, of those patients without their regular medicines for 3 or more days, half were over 60 years of age and as shown, more likely to be those on drugs required for maintenance of their cardiovascular stability. Most of these patients were undergoing major surgery and hence exposed to the associated significant cardio-respiratory stress. Consequently it would not be surprising if sudden or prolonged withdrawal of these drugs in these patients added significant risk to their surgery and complicated outcome.
The observation that being ‘ndm’ for > 2 days increased nonsurgical complications is compatible with the interpretation that the complication causes the person to be ‘ndm’ rather than lack of drug causing the complication. We applied the Bradford Hill criteria to determine causation or association [29] and the Bradford Hill criterion of ‘temporality’ can be invoked. It could be argued that patients were unable to take drugs by the oral route because of complications suffered postoperatively. The most obvious complications that would prevent patients from taking anything (food/fluids/medicines) orally, would be an ileus or protracted vomiting. However, brief periods of ileus are generally present but not considered a ‘morbid’ complication. This argument can be discounted because of the 373 complications recorded, there were only six such gastrointestinal complications, < 2% of all complications.
Statistical analysis of the data from this study showed that the longer patients were without their regular medicines, the more nonsurgical complications that arose, regardless of the duration and magnitude of operation and cardiovascular complications in particular, increased with increasing time without regular drug therapy. One of the most compelling pieces of supporting evidence, were the case studies. These were recorded only when all other reasons other than medicine withdrawal could be reasonably discounted as causal factors. In every case, covering a wide spectrum of complications and medicines, the symptoms/complication resolved as soon as the patients' regular medicines were re-instated.
Even though this is one of the largest studies of drug use in surgical patients in that drug withdrawal has significant implications, we concede that prolonged drug withdrawal may simply be associated with more severe procedures in sicker patients. Not until a further study, is undertaken in which complication rates are compared following ‘early’ vs ‘normal time’ of reinstitution of patients' drug therapy will the causal relationship of regular drug therapy with postoperative complications be established. Until then, however, this study shows that being on a drug unrelated to surgery affects outcome. This signals that more attention needs to be paid to a patient's regular drug therapy as part of preoperative assessment and postoperative care in a surgical unit. It would be helpful for the surgical team to be more aware of the impact of their patients' drug therapy unrelated to their surgery. This is in addition to the more well described effects of insulin, warfarin and steroid therapy on surgical management. There may be a special role for the clinical pharmacists to monitor drug withdrawal and alert the surgical team to therapeutic options. Steps to reinstitute early therapy should be considered with early refeeding, possible via the jejunal route.
Both in New Zealand and other countries, the elderly will constitute a larger proportion of the surgical workload in the future. They are generally more frail, on more drugs, and undergoing more major surgery [18, 30]. This study has shown that examination of a patient's drug chart should give the clinician a useful estimate of the patient's added risk of complications in the postoperative period. Particular attention to the need for these drugs, their interactions, possible consequences of sudden withdrawal may reduce risks and improve outcomes and that a thoughtless approach, either continuing or discontinuing drugs is likely to cause problems. By paying attention to the patient's usual drug therapy postoperatively aggravation of this coexisiting conditions may be minimized, hospital stays may well be shortened and the overall postoperative course, less hazardous.
References
- 1.Seymour DG, Vaz FG. A prospective study of elderly general surgical patients: II Postoperative complications. Age Ageing. 1989;18:316–326. doi: 10.1093/ageing/18.5.316. [DOI] [PubMed] [Google Scholar]
- 2.Duthie DKR, Montgomery JN, Spence AA, Nimmo WS. Concurrent drug therapy in patients undergoing surgery. Anaesthesia. 1987;42:305–306. doi: 10.1111/j.1365-2044.1987.tb03045.x. [DOI] [PubMed] [Google Scholar]
- 3.Wyld R, Nimmo WS. Do patients fasting before and after operation receive their prescribed drug treatment? Br Med J. 1988;296:744. doi: 10.1136/bmj.296.6624.744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kluger MT, Owen H. Premedication. An audit. Anaesthesia. 1991;46:224–227. doi: 10.1111/j.1365-2044.1991.tb09415.x. [DOI] [PubMed] [Google Scholar]
- 5.Kluger MT, Gale S, Plummer JL, Owen H. Peri-operative drug prescribing patterns and manufacturers' guidelines. Anaesthesia. 1991;46:456–459. doi: 10.1111/j.1365-2044.1991.tb11682.x. [DOI] [PubMed] [Google Scholar]
- 6.Hansson L, Hunyor SN, Julius S, Hoobler SW. Blood pressure crisis following withdrawal of clonidine (Catapres, Catapresan), with special reference to arterial and urinary catecholamine levels and suggestions for acute management. Am Heart J. 1973;85:605–610. doi: 10.1016/0002-8703(73)90165-8. [DOI] [PubMed] [Google Scholar]
- 7.Kaplan JA, Dunbar RW, Bland JW, Sumpter R, Jones EL. Propranolol and cardiac surgery: a problem for the anesthesiologist? Anesthesia Analgesia. 1975;54:571–578. doi: 10.1213/00000539-197509000-00003. [DOI] [PubMed] [Google Scholar]
- 8.Miller RR, Olson HG, Amsterdam EA, Mason DT. Propranolol-withdrawal rebound phenomenon. N Engl J Med. 1975;293:416–418. doi: 10.1056/NEJM197508282930902. [DOI] [PubMed] [Google Scholar]
- 9.Bruce DL, Croley TF, Lee JS. Preoperative clonidine withdrawal syndrome. Anesthesiology. 1979;51:90–92. doi: 10.1097/00000542-197907000-00024. [DOI] [PubMed] [Google Scholar]
- 10.George CF. Hazards of the abrupt withdrawal of drugs. Prescribers J. 1985;25:31–39. [Google Scholar]
- 11.Fried M, Schwander J. Hypertensive crisis after withdrawal of clonidine and nadolol. Case report and review of the literature. Schweiz Med Wochenschrift. 1987;117:874–878. [PubMed] [Google Scholar]
- 12.Dilsalver SC, Coffman JA. Antipsychotic withdrawal phenomena in the medical-surgical setting. Gen Hosp Psychiatry. 1988;10:438–446. doi: 10.1016/0163-8343(88)90068-0. [DOI] [PubMed] [Google Scholar]
- 13.Musa MN. Sleep apnea following withdrawal of amitriptyline. J Clin Pharmacol. 1988;28:1038–1039. doi: 10.1002/j.1552-4604.1988.tb03126.x. [DOI] [PubMed] [Google Scholar]
- 14.McEvoy GK. American Society of Hospital Pharmacists; 1987. Drug information 1987 edition; p. 2091. [Google Scholar]
- 15.Pettigrew RA, McDonald JR, van Rij AM. Developing a system for surgical audit. Australia NZ J Surgery. 1991;61:563–569. doi: 10.1111/j.1445-2197.1991.tb00295.x. [DOI] [PubMed] [Google Scholar]
- 16.Goldman L. Cardiac risk in noncardiac surgery: an update. Anesth Analg. 1995;80:810–820. doi: 10.1097/00000539-199504000-00028. [DOI] [PubMed] [Google Scholar]
- 17.Nolan L, O'Malley K. Adverse drug reactions in the elderly. Br J Hosp Med. 1989;41:452–457. [PubMed] [Google Scholar]
- 18.Cook L. The growing elderly population. New Zealand Now: 65 plus. 1995:13–25. [Google Scholar]
- 19.Saklad M. Grading of patients for surgical procedures. Anesthesiology. 1941;2:281–284. [Google Scholar]
- 20.Dripps RD, Lamount A, Eckenhoff JE. The role of anaesthesia in surgical mortality. JAMA. 1961;178:261–268. doi: 10.1001/jama.1961.03040420001001. [DOI] [PubMed] [Google Scholar]
- 21.Goldman L, Caldera DL, Nussbaum SR, et al. Multifactorial index of cardiac risk in noncardiac surgical procedures. N Engl J Med. 1977;297:845–850. doi: 10.1056/NEJM197710202971601. [DOI] [PubMed] [Google Scholar]
- 22.Mangano DT. Perioperative cardiac mortality. Anesthesiology. 1990;72:153–184. doi: 10.1097/00000542-199001000-00025. [DOI] [PubMed] [Google Scholar]
- 23.Pettigrew RA, Burns HJG, Carter DC. Evaluating surgical risk: the importance of technical factors in determining outcome. Br J Surg. 1987;74:791–794. doi: 10.1002/bjs.1800740912. [DOI] [PubMed] [Google Scholar]
- 24.Detsky AS, Abrams HB, Forbath N, Scott JG, Hilliard JR. Cardiac assessment for patients undergoing noncardiac surgery: multifactorial clinical risk index. Arch Intern Med. 1986;146:2131–2134. [PubMed] [Google Scholar]
- 25.Vacanti CJ, van Houten RJ, Hill RC. A statistical analysis of the relationship of physical status to postoperative mortality in 68, 388 cases. Anesth Analg. 1970;49:564–566. [PubMed] [Google Scholar]
- 26.Salazar C, Frishman W, Friedman Patel J, et al. (-Blockade therapy for supraventricular tachyarrhythmias after coronary surgery: a propranolol withdrawal syndrome? Angiology. 1979;30:816–819. doi: 10.1177/000331977903001204. [DOI] [PubMed] [Google Scholar]
- 27.Goldman L. Noncardiac surgery in patients receiving propranolol. Case reports and recommended approach. Arch Intern Med. 1981;141:193–196. [PubMed] [Google Scholar]
- 28.Dilsaver S, Greden J. Antidepressant withdrawal phenomena. Biol Psychiatry. 1984;19:237–256. [PubMed] [Google Scholar]
- 29.Bradford Hill SA. The Environment and Disease: association or causation? Proc Roy Soc Med. 1965;57:295–300. doi: 10.1177/003591576505800503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Seymour DG, Vaz FG. Aspects of surgery in the elderly: preoperative medical assessment. Br J Hosp Med. 1987;37:102–112. [PubMed] [Google Scholar]


