Abstract
Aims
Accurate recording of medication histories in hospital medical records (HMR) is important when patients are admitted to the hospital. Lack of registration of drugs can lead to unintended discontinuation of drugs and failure to detect drug related problems. We investigated the comprehensiveness of medication histories in HMR with regard to prescription drugs by comparing the registration of drugs in HMR with computerized pharmacy records obtained from the community pharmacy.
Methods
Patients admitted to the general ward of two acute care hospitals were included in the study after obtaining informed consent. We conducted an interview on drugs used just prior to hospitalization and extracted the medication history from the HMR. Pharmacy records were collected from the community pharmacists over a 1 year period before the admission. Drugs in the pharmacy records were defined as possibly used (PU-drugs) when they were dispensed before the admission date and had a theoretical enddate of 7 days before the admission date or later. If any PU-drug was not recorded in the HMR, we asked the patient whether they were using that drug or not.
Results
Data were obtained from 304 patients who had an average age of 71 (range 40–92) years. The total number of drugs according to the HMR was 1239, 43 of which were not used. When compared with the pharmacy records we found an extra 518 drugs that were not recorded in the HMR but were possibly in use. After verification with the patients, 410 of these were indeed in use bringing the total number of drugs in use to 1606. The type of drugs in use but not recorded in the HMR covered a broad spectrum and included many drugs considered to be important such as cardiovascular drugs (n = 67) and NSAIDs (n = 31). The percentages of patients with 0, 1, 2, 3, 4, 5–11 drugs not recorded in the HMR were 39, 28, 16, 8, 3.6 and 5.5, respectively. Of the 1606 drugs in use according to information from all sources, only 38 (2.4%) were not retrievable in the pharmacy records when the complete year prior to hospitalization was evaluated.
Conclusions
The medication history in the hospital medical record is often incomplete, as 25% of the prescription drugs in use is not recorded and 61% of all patients has one of more drugs not registered. Pharmacy records from the community pharmacist can be used to obtain more complete information on the medication history of patients admitted to the hospital.
Keywords: general internal ward, hospital, medical records, medication histories, pharmacy records
Introduction
The prescribing of medication is an integral part of daily clinical care. In order for physicians to prescribe medication safely it is necessary that they have a complete description of the drugs a patient uses. This is particularly important when patients are concurrently or sequentially treated by several physicians. Inaccuracies in the medication history may lead to duplication of drugs, unwanted drug interactions, discontinuation of medication use, and to the failure to detect drug related problems. In outpatients, some of these problems, like double medication and unwanted drug interactions, may be filtered out by the community pharmacist, if a patient gets his drugs from a single pharmacy. Risks are increased when a patient is admitted to the hospital, because of the loss of the community pharmacy filter and because patients are often unable to report accurately the drugs they are taking [1], even though they are requested to bring their medication to the hospital [2].
Studies on the completeness of hospital medical records with respect to the drugs a patient uses directly prior to hospital admission are scarce and have several limitations. The completeness of hospital medical records may be evaluated by comparison with questionnaire information only [3], by comparison with computerized files of dispensed prescriptions in community pharmacies [4, 5] and indirectly by comparison of community pharmacy records with hospital pharmacy records [6]. Questionnaire information might be hampered by recall bias and the comparison with community pharmacy records is limited to one or a small number of drug classes [4, 5].
Recently we showed that in the Netherlands community pharmacy records were virtually complete with regard to the prescription drugs when drugs found at a patient's home were taken as the gold standard [7]. We therefore performed a study into the completeness of medication histories in hospital medical records of patients admitted to general internal medicine wards by comparing these records with computerized pharmacy records obtained from the community pharmacy.
Methods
Design
This was a prospective study from June 1993 to July 1995 in which patients admitted to the general internal medicine ward of two acute care hospitals (Utrecht, the Netherlands) were eligible for inclusion after informed consent was obtained. The protocol was approved by the local research ethics committee. Due to logistical constraints, the maximum number of patients included per working day was three. When three or less elegible patients were admitted, all these patients were included. When there were more than three eligible patients, three patients were included, selected randomly from the admission files. Patients were eligible if they were 40 years or older, had a planned stay of more than 2 days, and if verbal contact was possible within 24 h of admission and was sufficient to conduct an interview. Patients admitted because of a suicide attempt were excluded. During the study period 840 admissions were evaluated for inclusion in the study. Some 439 patients were not eligible because of various reasons; 219 patients had a planned stay of no more than 2 days, 104 patients were too young, 6 patients were admitted because of autointoxication, in 83 patients verbal contact was not possible within 24 h, and in 27 admissions the patient was already included in the study on an earlier admission, leaving 401 patients eligible for inclusion. Thirty-two patients refused to participate in the study, leaving 369 patients in the main study. Furthermore, patients registered with a general practice with its own pharmacy practice (10), of whom the community pharmacy could not be retrieved (2), who were transferred to another department within 2 days after hospital admission (10), who did not use any drugs (28), of whom the medication history was not available from their community pharmacy in time (8), and patients of whom the questionnaire was regarded as inaccurate (8) were excluded from this study, leaving 304 evaluable patients. (In one patient both the questionnaire was inaccurate and the medication history was not available from the community pharmacy).
Data collection and coding
All patients were interviewed to solicit information concerning all medication used before hospitalization and medication as listed in the hospital medical records was extracted. The interviews were conducted by the main researcher or by a pharmacy research student who received sufficient instruction to conduct the interview. A structured form was used to guide the interview and to note down the answers. The interviews were conducted mostly on the day after the admission at the bedside of the patient, or if so requested, in a private room. For every medication listed in the medication history of the hospital record and for any additional medication mentioned during the interview, we asked the patient, whether he or she was using the medication just prior to hospital admission, and the regimen of use. Most patients in the Netherlands are registered with and obtain their prescription drugs from one community pharmacy, and computerized registration of prescription drug use is reasonably complete in community pharmacies [7]. Pharmacy records over a 1 year period before the admission were collected from the community pharmacy where the patient was registered. The goals of the study were explained to the community pharmacists, and a copy of the informed consent was sent to them. The pharmacy records were usually obtained within 24 h by Fax, or otherwise by regular mail. For every prescription in the pharmacy records theoretical enddate of use was calculated based on information on the amount of drug dispensed and the direction for use (prescribed daily dose). When directions for use were not available in the pharmacy records, the defined daily dose (DDD) was used to calculate the theoretical enddate. For dermal, eye and ear, nose and throat (ENT) preparations we assumed a standard length of use of 1 month. In the pharmacy records, a drug was defined as possibly in use at the moment of hospital admission (PU-drug) when it had a dispense date before the admission date and a theoretical enddate of 7 days before the admission date or later. This 7 day period was arbitrarily chosen to take into account noncompliance of drug intake. For any PU-drug in the pharmacy record that was not recorded in the hospital medical record, we went back to the patient and asked whether he or she was using that drug or not at the moment of hospital admission.
All prescription drugs were coded according to the Anatomical Therapeutic Chemical (ATC) classification system [8]. Extemporaneously prepared drugs and drugs that had no ATC code, such as homeopathic drugs, were excluded from the analysis. As Over The Counter (OTC) drug use is not recorded in the community pharmacy records, we also excluded OTC drugs.
We defined three types of errors of registration of medication use in the medication history of the hospital medical record. An omission error was defined as a drug that was not registered in the hospital medical records but was in fact a PU-drug according to the pharmacy records and was in use according to the interview. A commission error was defined as a drug that was registered in the hospital medical record, but was not being used by the patient at the moment of hospital admission. The third error we considered were registration errors, which is the combination of omission and commission errors. Other types of errors such as in dose or in frequency were not considered in our analysis.
Analysis
The completeness of the medication history in the hospital medical record was calculated for the two hospitals separately and combined. For comparison of differences between the hospitals the chi-square test was used for dichotomous variables and the Student's t-test for continuous variables. We assessed the completeness of the hospital medical records in several ways. The total number of drugs registered in the hospital medical records was expressed as a percentage of the total number of drugs in use, obtained when data from the hospital medical record, the pharmacy records and the questionnaire were combined. We also calculated the number of registration errors per patient, for the whole study group and by age categories and sex. For the most commonly used drug groups, we calculated the number and the percentage of errors per drug group. We only present the results of both hospitals combined as the analysis showed no statistically significant differences at the α = 0.05 level between the hospitals with regards to all variables tested.
Results
The 304 patients had an average age of 71.5 (s.d. 12.8) years. Sixty-four percent were female and the average number of drugs per patient registered in the hospital medical records was 4.1 (s.d. 3.0). Forty-one percent of the patients were admitted electively, while 59% were admitted as emergencies. The discharge diagnoses are listed in Table 1. Table 2 shows the completeness, and the number of omission and commission errors in the medication history in hospital medical records when all drugs are considered. According to the hospital medical records 1239 drugs were used at the moment of hospital admission. The questionnaire showed that the number of commission errors was small, as only 43 of these 1239 drugs were not being used. When additional data from the pharmacy records was considered, 518 drugs were found that were possibly in use (PU-drugs) but which were not registered in the hospital medical records. Out of these 518 PU-drugs, 410 (79%) were found to be in use on questioning the patients, which brings the total number of drugs in use to 1606 (1196 + 410). Omission errors (26% of all drugs in use) were far more common than commission errors (2.7% of all drugs in use).
Table 1.
Discharge diagnoses in 304 patients admitted to the general internal ward⋆.
| Category | Number | Percentage |
|---|---|---|
| Gastrointestinal disease | 83 | 27 |
| Malignant tumours | 41 | 13 |
| Cardiovascular disease | 28 | 9.2 |
| Diabetes mellitus | 28 | 9.2 |
| Haematologic disease | 26 | 8.6 |
| Thrombotic disease | 16 | 5.3 |
| Pulmonary disease | 15 | 4.9 |
| Diseases of the urinary tract | 11 | 3.6 |
| Musculoskeletal disease | 8 | 2.6 |
| Hepatic disease | 6 | 2.0 |
| Other | 42 | 13.8 |
To avoid duplicate categorization, all tumours except haematologic tumours were entered in the category ‘malignant tumours’.
Table 2.
Completeness of the medication history, and frequency of omission and commission errors in hospital medical records of 304 patients.
| Total | |
|---|---|
| Number of drugs in HMR | 1239 |
| used according to questionniare | 1196 |
| not used according to questionniare (commission errors) | 43 |
| PU-drugs, not present in HMR | 518 |
| used according to questionniare (omission errors) | 410 |
| not used according to questionniare | 108 |
| Drugs used based on information from all sources⋆ | 1606 |
| Number of omission errors (%) | 410 (26) |
| Number of commission errors (%) | 43 (2.7) |
This is the summation of the drugs in the HMR, used according to the questionnaire and the PU-drugs, not present in the questionnaire, but used according to the questionnaire.
Percentage of drugs used based on information from all sources.
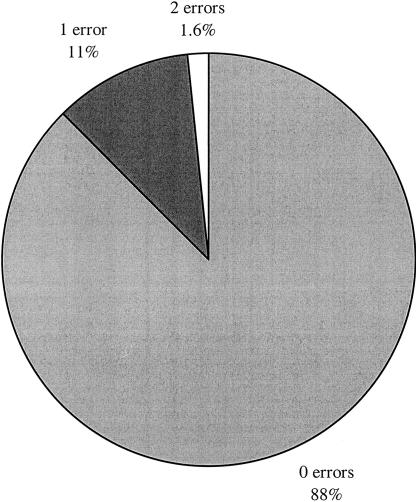
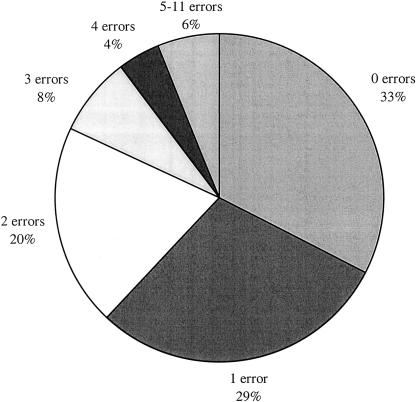
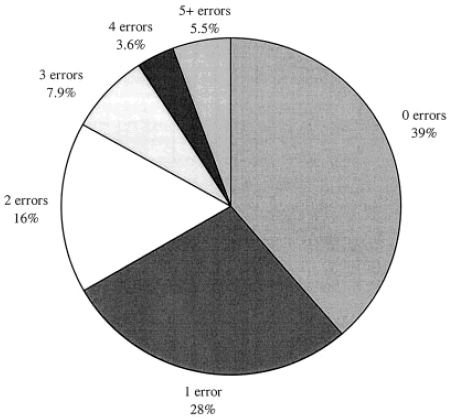
Figures 1 and 2 show the distribution of omission and commission errors per patient, respectively. Sixty-one percent of all patients had one or more omission errors, while 17% had three or more omission errors. As was noted earlier, commission errors were far more rare, as 87.5% of all patients had no commission errors, while 11% and 1.6% had one and two commission errors, respectively. Figure 3 shows the distribution of registration errors (omission and commission errors combined). The percentage of patients with no registration errors in the medication history was 33%, while 67% had one or more registration errors and 18% had three or more registration errors. In Table three the distribution of registration errors is given according to age category and sex. There is no clear relation between the distribution of registration errors and age categories. Women are more likely to have registration errors in the hospital medical records than men, as only 28% of women have no registration errors against 40% of men.
Figure 1.
Distribution of number of omission errors per patient in the hospital medical records of 304 patients.
Figure 2.
Distribution of number of commission errors per patient in the hospital medical records of 304 patients.
Figure 3.
Distribution of number of registration errors per patient in the hospital medical records of 304 patients.
Table 3.
Distribution of registration errors in the hospital medical records of 304 patients, by age category and sex.
| 0 errors per patient | 1 error per patient | ≥ 2 errors per patient | ||||
|---|---|---|---|---|---|---|
| Category | n | % | n | % | n | % |
| Age category (years) | ||||||
| 40–49 | 9 | 32 | 11 | 39 | 8 | 29 |
| 50–59 | 13 | 41 | 7 | 22 | 12 | 38 |
| 60–69 | 20 | 39 | 11 | 22 | 20 | 39 |
| 70–79 | 25 | 25 | 33 | 32 | 44 | 43 |
| 80–89 | 27 | 33 | 27 | 33 | 28 | 34 |
| 90–99 | 5 | 56 | 0 | 0 | 4 | 44 |
| Sex | ||||||
| Male | 44 | 40 | 30 | 28 | 35 | 32 |
| Female | 55 | 28 | 59 | 30 | 81 | 42 |
Table 4 shows the most commonly used drugs and drug categories and the number and percentage of registration errors in a given drug or drug category. Because the patients use many different drugs, the number of registration errors within each drug or drug category is relatively small.
Table 4.
Most commonly used medications and frequency and percentage of registration errors in 304 patients.
| Medication | Frequency of use | Frequency of errors | % error |
|---|---|---|---|
| Benzodiazepines | 121 | 40 | 33 |
| NSAIDS | 81 | 31 | 38 |
| Frusemide | 68 | 11 | 16 |
| Oral antidiabetics | 68 | 13 | 19 |
| Paracetamol | 60 | 28 | 47 |
| β-adrenoceptor blockers | 57 | 5 | 8.8 |
| Nitrates | 56 | 14 | 25 |
| ACE-inhibitors | 48 | 6 | 13 |
| H2-receptor blockers | 46 | 11 | 24 |
| Diuretics | 43 | 5 | 12 |
| Low-dose acetylsalicylic acid | 43 | 9 | 21 |
| Digoxin | 37 | 5 | 14 |
| β2-sympathomimetics | 37 | 7 | 19 |
| Oral anticoagulants | 33 | 1 | 3.0 |
| Antacids | 32 | 7 | 22 |
| Omeprazole | 29 | 4 | 14 |
| Inhalation corticosteroids | 25 | 5 | 20 |
| Insulin | 24 | 2 | 8.3 |
| Oral corticosteroids | 21 | 6 | 29 |
Registration errors are not restricted to certain drug categories, although the error percentages are higher for drugs that are used to treat pain symptoms such as paracetamol and NSAIDs. Many of the errors concern important drug categories such as cardiovascular and antidiabetic drugs.
Table 5 shows the completeness of the pharmacy records, by classifying drugs that were present in the hospital medical record according to their presence or absence in the pharmacy record. Most of the drugs that were in use according to all sources combined were present in the pharmacy records. Out of 1606 drugs, 1568 (97.6%) were retrievable in the pharmacy records. A minor fraction (8.8%) of the drugs that were retrievable in the pharmacy records were not classified as PU-drugs, while, in fact, they were in use.
Table 5.
Completeness of pharmacy records of 304 patients.
| Number of drugs | %† | |
|---|---|---|
| Drugs in use according to information from all sources⋆ | 1606 | 100 |
| Drugs retrievable in pharmacy records | 1568 | 97.6 |
| Drugs classified as PU-drug | 1427 | 88.9 |
| Drugs not classified as PU-drug | 141 | 8.8 |
| Drugs not retrievable in pharmacy records | 38 | 2.4 |
Summation of the drugs in the HMR, used according to the questionnaire and the PU-drugs, not present in the questionnaire, but used according to the questionnaire.
Percentage of total number of drugs in use according to information from all sources.
Discussion
Our study shows that the medication history in the hospital medical record is often incomplete, as 26% of the prescription drugs in use is not recorded and 67% of all patients has one of more drugs that are either not registered in the hospital medical record or registered but not in use. Our estimate of the completeness of the inpatient medical record is probably conservative as we took into account only errors of omission and commission and did not consider errors in dose or regimen. Our results show that some drugs that were in use according to the medical records were not classified as PU-drugs in the pharmacy records. The most important reason for this discrepancy is that to make comparisons between the medication history in the medical records and in pharmacy records, the theoretical length of use of the drugs in the pharmacy records has to be defined. When the actual use of a drug deviates from the theoretical use, there is an increased likelihood that drugs are misclassified in the pharmacy records. This misclassification is confirmed since not all PU-drugs are in use. On the other hand, some drugs in the pharmacy records could be in use, while they were not classified as PU-drugs. The implication of this misclassification is that our estimate of the number of PU-drugs is conservative and that there are probably more drugs in the pharmacy records that should be considered as possibly in use at the moment of hospitalization.
In some instances the pharmacy records could not be obtained in time to allow us to go back to the patient to ask questions on PU-drugs. This occurred only in 8 out of 312 (2.6%) cases, though.
The applicability of community pharmacy records to get more complete information on the medication history depends on a (virtually) complete registration of medication drug use in the community pharmacy, as is the case in the Netherlands for prescription drugs [7].
The results of our study are comparable with those of Beers et al. [3]. The design of their study was similar to ours with the exception that they did not use pharmacy records, but used an extensive questionnaire with specific questions to identify drugs not recorded in the medical record, thereby introducing the possibility of recall errors by the patient. They found that, with regard to important drugs, 60% of all patients had one or more error, and 18% had three or more. Van Hessen et al. studied the continuation of outpatient medication in 205 patients after admission to the hospital by comparing community-pharmacy records with hospital-pharmacy records [6]. Drugs that were in use according to the community-pharmacy records, but were not retrievable in the hospital-pharmacy records, were categorized by an expert panel as discontinuations that will not cause problems, as discontinuations that will probably not cause problems, or as discontinuations that should not have occurred, unless purposefully done on the advice of the attending physician. In the last, most serious category of discontinuations, 15 discontinuations in 12 patients (6%) were considered inadvertent as no information was found that could explain the discontinuation. The evidence for the conclusion of the authors that information of drug histories obtained at the time of hospital admission is not always accurate is indirect, as the completeness of the medical records was not studied, and as other reasons such as a omission to record the reason for stopping a drug in the medical history might account for the lack of information.
Strom et al. [4] and Guess et al. [5] also used computerized files of dispensed prescriptions to evaluate the completeness of the medication history in the inpatient medical record, but were restricted to one or a small number of drug classes. In the study of Strom et al. [4], the registration of drugs that are commonly linked with causing the Stevens–Johnson syndrome in the inhospital medical record was compared with outpatient Medicaid pharmacy claims files. Only 50% of the 234 prescriptions for these drugs known to be dispensed in the 30 days prior to hospitalization were retrieved. In the study of Guess et al. [5] of persons with fatal upper gastrointestinal haemorrhage or perforation, the use of NSAIDs was mentioned in the discharge or autopsy report for only 31% of cases identified as exposed according to the drug file.
In agreement with Beers et al. we found that omission errors were far more common than commission errors [3]. Their estimation of the number of commission errors could be too low though, as patients tend to deny their nonadherence to medical advice [9]. The expression of the registration errors as a fraction of the frequency of use showed that the errors were not confined to certain drug categories, and that high error percentages were seen in important drug categories, as NSAIDs (38% registration errors), oral antidiabetics (19%), and inhalation corticosteroids (20%).
Unawareness of health care providers of the drugs a patient takes at home can result in several problems. Price et al. showed that a major proportion of patients admitted to the general medical ward used drugs that were inappropriate or seemed unnecessary [10]. The method that we employed to obtain the medication history from the community pharmacy was quick and easy to implement. Recently, several initiatives between hospital and community pharmacists have been set up in the Netherlands to improve transfer of medication history and prescriptions between hospitals, general practices, and community pharmacies [11]. The Dutch Colleges of community and hospital pharmacists have collaborated to set up a draft, including criteria, on ‘seamless pharmaceutical care’ (transmurale zorg) as a guide for the pharmaceutical profession [12]. These developments in the pharmaceutical profession provide the possibility to offer patients who are transferred between primary and secondary care continuous pharmaceutical care.
We conclude that the medication history in the hospital medical record of general internal patients is often incomplete and that pharmacy records from the community pharmacy are easily available and can be used to obtain more complete information on the medication history of patients admitted to the hospital.
References
- 1.Schwarz A, Faber U, Borner K, Keller F, Offermann G, Molzahn M. Reliability of drug history in analgesic users. Lancet. 1984;2:1163–1164. doi: 10.1016/s0140-6736(84)91608-8. [DOI] [PubMed] [Google Scholar]
- 2.Gilchrist WJ, Lee YC, Tam HC, MacDonald JB, Williams BO. Prospective study of drug reporting of general practitioners for an elderly population referred to a geriatric service. Br Med J. 1987;294:289–290. doi: 10.1136/bmj.294.6567.289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Beers MH, Munekata M, Storrie M. The accuracy of medication histories in the hospital medical records of elderly persons. J Am Geriatr Soc. 1990;38:1183–1187. doi: 10.1111/j.1532-5415.1990.tb01496.x. [DOI] [PubMed] [Google Scholar]
- 4.Strom BL, Carson JL, Halpern AC. Using a claims database to investigate drug-induced Stevens–Johnson syndrome. Statistics Med. 1991;10:565–576. doi: 10.1002/sim.4780100408. [DOI] [PubMed] [Google Scholar]
- 5.Guess HA, West R, Strand LM, Helston D, Lydick EG, Bergman U, Wolski K. Fatal upper gastrointestinal hemorrhage or perforation among users and nonusers of nonsteroidal anti-inflammatory drugs in Saskatchewan, Canada 1983. J Clin Epidemiol. 1988;41:35–45. doi: 10.1016/0895-4356(88)90007-8. [DOI] [PubMed] [Google Scholar]
- 6.Van-Hessen PA, Petri H, Urquhart J. Do prescribed drugs always follow the patients to hospital? Pharm Weekbl [Sci] 1990;12:66–70. doi: 10.1007/BF01970148. [DOI] [PubMed] [Google Scholar]
- 7.Lau HS, de Boer A, Beuning KS, Porsius AJ. Validation of pharmacy records in drug exposure assessment. J Clin Epidemiol. 1997;50:619–625. doi: 10.1016/s0895-4356(97)00040-1. [DOI] [PubMed] [Google Scholar]
- 8.Anonymous. Guidelines for ATC Classification. Oslo: WHO Collaborating centre for drug statistics methodology – Nordic Council on medicines; 1990. [Google Scholar]
- 9.Cramer JA, Spilker B, editors. Patient Compliance in Medical Practice and Clinical Trials. New York: Raven Press; 1991. pp. 3–10. [Google Scholar]
- 10.Price D, Cooke J, Singleton S, Feely M. Doctors' unawareness of the drugs their patients are taking: a major cause of overprescribing? Br Med J. 1986;292:99. doi: 10.1136/bmj.292.6513.99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Balhuizen F. Transmurale farmacie in Nederland: een terrein in ontwikkeling [Seamless pharmaceutical care in the Netherlands: a field in development] Pharm Weekbl. 1996;129:85–86. [Google Scholar]
- 12.Dutch Colleges of community and hospital pharmacy. Transmurale farmacie, beter: transmurale farmaceutische zorg. Pharm Weekbl. 1997;132:977–979. [Google Scholar]