Abstract
As of April 2007 the early open artery hypothesis is alive and well, but the late open artery hypothesis is adrift. For the foreseeable future, stable patients with persistent occlusion of the infarct artery late after myocardial infarction, and without severe ischaemia or uncontrollable angina, should be managed initially with optimal medical treatment alone, and not with percutaneous coronary intervention. Efforts should focus on establishing reperfusion earlier, including reducing the time to patient presentation.
Keywords: open artery hypothesis, Occluded Artery Trial
Basic and clinical research elucidated the concept that an epicardial coronary artery occlusion leads to an advancing wavefront of necrosis, which progresses from endocardium to epicardium.1,2 This wavefront also advances radially and leads to a border zone of mixed infarcted, viable and dysfunctional, and viable but ischaemic myocytes. Coronary reperfusion before the wavefront of necrosis is complete diminishes infarct size, improves regional and global left ventricular (LV) function, and reduces mortality.
It was not until the development of pharmacotherapy to open infarct arteries, however, that studies like the Western Washington intracoronary streptokinase trial could demonstrate that interruption of the wavefront of myocardial necrosis could also take place in humans.3 At present, stenting of patients with ST elevation myocardial infarction leads to a patent artery in over 90% of patients.4,5 From the outset of these efforts at reperfusion it had been clear that the earlier after occlusion reperfusion occurred, the more complete the salvage of myocardium. Other lines of evidence, however, hinted that late reperfusion, too late for myocardial salvage, might also be advantageous.6,7,8
Late reperfusion
Experiments in late reperfusion of the experimental infarct suggested that preservation of LV geometry6,7 was possible, even in the absence of myocardial salvage. The improved survival of patients in thrombolytic trials appeared out of proportion to the improvement in ejection fraction (EF), suggesting that late infarct artery patency carried its own incremental benefit, above and beyond that of myocardial salvage. The total benefit of reperfusion was thought to be the sum of the benefit of myocardial salvage plus the benefit of having an open artery after myocardial infarction (MI). Retrospective analyses of clinical trials like SAVE suggested that even when a severe infarct occurred and differences in EF were controlled for, leaving the hospital with an open artery predicted a good prognosis.8 The concept that late opening of an occluded artery might be beneficial remains appealing, because recent data suggest that many patients with acute MI fail to receive timely reperfusion treatment either because of late or atypical presentation.
A number of mechanisms were proposed for this finding, and the most plausible of these centred on stabilisation or prevention of LV remodelling. Other lines of discussion focused on electrical stabilisation of an arrhythmogenic substrate, recruitment of hypofunctional border‐zone myocardium, and provision of collaterals to other coronary beds that might themselves become ischaemic.9,10,11 Thus, more than a decade ago, multiple investigators called for a clinical trial to test the veracity of the late open artery hypothesis.
Four small trials of percutaneous coronary intervention (PCI) in late post‐MI in patients with occluded infarct arteries were designed, executed, and published.12,13,14,15 These trials had variable results, ranging from an optimistic reduction in LV remodelling and events, to, paradoxically, an increase in LV volumes and clinical events with PCI. Thus, as so often happens in the scientific evaluation of complex medical subjects, small‐scale studies that focus on surrogate physiological end points may give incomplete answers, but do prepare the field for a definitive trial.
Occluded Artery Trial (OAT)
The recently published OAT is the only robust trial in the field.16,17 OAT was sponsored by the National Heart, Lung and Blood Institute, and brought together 217 sites from 24 countries. A total of 2166 patients enrolled between February 2000 and December 2005. Enrolled patients had sustained an MI within 28 days, with certain high‐risk features, notably a proximal occlusion of a major epicardial artery, or LV dysfunction with an EF <50. The time window permitted patient enrolment just over 24 hours after MI. Patients underwent coronary angiography and, if an eligible occluded artery was found and they were clinically stable without three‐vessel disease, they were randomly assigned to a PCI‐stent, or to leaving the artery occluded without further intervention. We required that patients be receiving optimal medical treatment regardless of the treatment group to which they were assigned. Patients were followed up for an average of 1059 days.
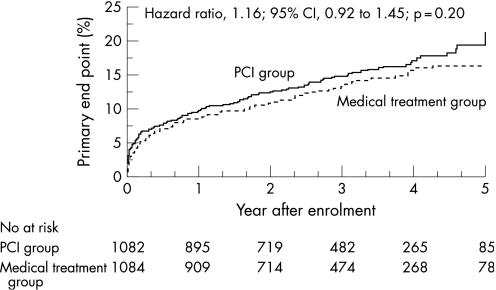
There was no benefit from performing PCI (17.2% 4‐year rate of death, MI or class IV heart failure for PCI vs 15.6% for optimal medical treatment only), and a trend towards excess early and late reinfarctions in the PCI‐treated group was noted (fig 1). Within this large trial, several smaller mechanistic ancillary studies confirmed that sustained epicardial coronary patency was present18 and there was often retained infarct‐zone viability in enrolled patients. A subset of 332 OAT patients underwent repeat angiography at 1 year after study entry. In the PCI group 87% had sustained patency, whereas in the medical group 25% had recanalised. Moreover, resting sestamibi scanning in another small subgroup confirmed retained infarct‐zone viability (>40% of peak tracer uptake) in 69% of 124 patients.
Figure 1 Kaplan–Meier curves for the Occluded Artery Trial primary end point: death from any cause, non‐fatal reinfarction, or NYHA class IV heart failure requiring admission to hospital or time in a short‐stay unit. Reproduced with permission from Hochman JS, Lamas GA, Buller CE, et al. Coronary intervention for persistent occlusion after myocardial infarction. N Engl J Med 2006;355:2395–407.16 Copyright © 2007 Massachusetts Medical Society. All rights reserved.
Is the open artery hypothesis still viable?
Therefore, although the benefit of opening the infarct artery early after infarct onset is not in doubt,19 it has now become necessary to ask the question posed: where does OAT leave the late open artery hypothesis? Let us review the critiques of OAT, and critically determine whether the open artery hypothesis has been laid to rest.
1. The OAT enrolled a low‐risk population; patients at high risk, particularly those with low EFs and proximal left anterior descending coronary artery occlusions, were not included.
The annualised event rates for OAT reflect the benefits of modern post‐MI care as well as the selection of patients who survived the first few days of the MI and were clinically stable. In fact, an annualised event rate of 4% is not low and the rate was below the expected range only for the heart failure end point. We did, however, prospectively identify high‐risk subgroups such as those with a low EF and left anterior descending infarct artery, where the risk of events was high, and there was still no suggestion of benefit.
2. The most likely benefits of late opening of the infarct artery are in attenuation of LV remodelling. It would take a long time for the clinical benefit to become apparent.
The angiographic ancillary study assessed LV remodelling 1 year after the index infarction.18 The EF increased to a similar degree in both groups. A multivariable analysis in a subgroup of patients with paired volumetric ventriculograms found that PCI patients tended to have less LV dilatation in diastole (p = 0.02) and systole (p = 0.04). Thus we are left with a hint that there may be opposing processes at work. Perhaps attenuation of LV remodelling is counterbalanced by adverse consequences of myocardial injury from procedure‐related embolisation and both early and late reinfarction.
3. The PCI techniques were not the most modern treatments, because few drug‐eluting stents were used.
Recent meta‐analyses comparing bare metal with drug‐eluting stents have been published.20,21,22,23 There is no evidence that drug‐eluting stents reduce the combined end point of death or MI. Furthermore, the LV remodelling benefit in the observational studies was demonstrated in patients with residual post‐MI stenoses, so restenosis should not adversely affect the potential protective effect of patency. Therefore, the stent type is not relevant to the interpretation of the primary end point.
4. In OAT, arteries were opened too late after the infarct; there might have been a benefit if the arteries had been opened earlier.
In OAT, the median time from MI to randomisation was 8 days, and patients assigned to PCI had their intervention within 24 hours after. By protocol, however, patients could be randomised just over 24 hours after MI. Subgroup analyses did not suggest any benefit from PCI at any time within the OAT time window.5
5. Does this mean that an occluded infarct artery should never be opened late?
The results of the OAT should not be extrapolated to clinical situations and patient subsets that were not included. For example, patients with cardiogenic shock revascularised up to 36 hours after onset of MI and 12 hours after shock onset derived a survival advantage over initial medical stabilisation.24 Additionally, rescue PCI after failed fibrinolytic treatment, or primary PCI up to 12–24 hours after the event, is recommended for unstable or high‐risk patients with ST elevation myocardial infarction.19 Those with severe ischaemia were excluded; there was no suggestion of benefit for the subset with mild to moderate ischaemia on a stress test. In stable patients the efficacy of an initial intensive medical approach, even in the presence of recorded ischaemia, is supported by the findings of the COURAGE study.25
Conclusions
The critiques above point out important considerations in the interpretation of OAT, but none temper its results. We respectfully submit that today, in April 2007, the early open artery hypothesis is alive and well, but the late open artery hypothesis is adrift.
Therefore, today and for the foreseeable future, stable patients, such as those enrolled in the OAT, with persistent occlusion of the infarct artery late after MI, and without severe ischaemia or uncontrollable angina, should be managed with an initial strategy of optimal medical treatment alone, and not with PCI. Efforts should focus on establishing reperfusion earlier, including reducing the time to patient presentation.
G Lamas
J Hochman
Abbreviations
EF - ejection fraction
LV - left ventricular
MI - myocardial infarction
OAT - Occluded Artery Trial
PCI - percutaneous coronary intervention
Footnotes
Competing interests: Dr Lamas has received speaking fees from CV Therapeutics, Medtronic, Guidant and Bristol‐Myers Squibb, and consulting fees from CV Therapeutics and Medtronic. Dr Hochman has received consulting fees from Eli Lilly, Bristol‐Myers Squibb, Sanofi Aventis, and CV Therapeutics, speaking fees from the Network for Continuing Medical Education (supported by Bristol‐Myers Squibb and Sanofi Aventis) and grant support to her institution for this study from Eli Lilly, Millennium Pharmaceuticals, Schering‐Plough, Guidant, and Merck.
References
- 1.Reimer K A, Lowe J E, Rasmussen M M.et al The wavefront phenomenon of ischemic cell death. 1. Myocardial infarct size vs duration of coronary occlusion in dogs. Circulation 197756786–794. [DOI] [PubMed] [Google Scholar]
- 2.Kloner R A, Ellis S G, Lange R.et al Studies of experimental coronary artery reperfusion. Effects on infarct size, myocardial function, biochemistry, ultrastructure and microvascular damage. Circulation 198368(Pt 2)I8–15. [PubMed] [Google Scholar]
- 3.Kennedy J W, Ritchie J L, Davis K B.et al The Western Washington randomized trial of intracoronary streptokinase in acute myocardial infarction. A 12‐month follow‐up report. N Engl J Med 19853121073–1078. [DOI] [PubMed] [Google Scholar]
- 4.Keeley E C, Boura J A, Grines C L. Comparison of primary and facilitated percutaneous coronary interventions for ST‐elevation myocardial infarction: quantitative review of randomised trials. Lancet 2006367579–588. [DOI] [PubMed] [Google Scholar]
- 5.Holmes D R, Jr, Gersh B J, Ellis S G. Rescue percutaneous coronary intervention after failed fibrinolytic therapy: have expectations been met? Am Heart J 2006151779–785. [DOI] [PubMed] [Google Scholar]
- 6.Force T, Kemper A, Leavitt M.et al Acute reduction in functional infarct expansion with late coronary reperfusion: assessment with quantitative two‐dimensional echocardiography. J Am Coll Cardiol 198811192–200. [DOI] [PubMed] [Google Scholar]
- 7.Hochman J S, Choo H. Limitation of myocardial infarct expansion by reperfusion independent of myocardial salvage. Circulation 198775299–306. [DOI] [PubMed] [Google Scholar]
- 8.Lamas G A, Flaker G C, Mitchell G.et al Effect of infarct artery patency on prognosis after acute myocardial infarction. The Survival and Ventricular Enlargement Investigators. Circulation 1995921101–1109. [DOI] [PubMed] [Google Scholar]
- 9.Braunwald E. Myocardial reperfusion, limitation of infarct size, reduction of left ventricular dysfunction, and improved survival. Should the paradigm be expanded? Circulation 198979441–444. [DOI] [PubMed] [Google Scholar]
- 10.Califf R M, Topol E J, Gersh B J. From myocardial salvage to patient salvage in acute myocardial infarction: the role of reperfusion therapy. J Am Coll Cardiol 1989141382–1388. [DOI] [PubMed] [Google Scholar]
- 11.Van de Werf F. Discrepancies between the effects of coronary reperfusion on survival and left ventricular function. Lancet 198911367–1369. [DOI] [PubMed] [Google Scholar]
- 12.Dzavik V, Beanlands D S, Davies R F.et al Effects of late percutaneous transluminal coronary angioplasty of an occluded infarct‐related coronary artery on left ventricular function in patients with a recent (<6 weeks) Q‐wave acute myocardial infarction (Total Occlusion Post‐Myocardial Infarction Intervention Study [TOMIIS]—a pilot study). Am J Cardiol 199473856–861. [DOI] [PubMed] [Google Scholar]
- 13.Horie H, Takahashi M, Minai K.et al Long‐term beneficial effect of late reperfusion for acute anterior myocardial infarction with percutaneous transluminal coronary angioplasty. Circulation 1998982377–2382. [DOI] [PubMed] [Google Scholar]
- 14.Steg P G, Thuaire C, Himbert D.et al DECOPI (DEsobstruction COronaire en Post‐Infarctus): a randomized multi‐centre trial of occluded artery angioplasty after acute myocardial infarction. Eur Heart J 2004252187–2194. [DOI] [PubMed] [Google Scholar]
- 15.Yousef Z R, Redwood S R, Bucknall C A.et al Late intervention after anterior myocardial infarction: effects on left ventricular size, function, quality of life, and exercise tolerance: results of the Open Artery Trial (TOAT Study). J Am Coll Cardiol 200240869–876. [DOI] [PubMed] [Google Scholar]
- 16.Hochman J S, Lamas G A, Buller C E.et al Coronary intervention for persistent occlusion after myocardial infarction. N Engl J Med 20063552395–2407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hochman J S, Lamas G A, Knatterud G L.et al Design and methodology of the Occluded Artery Trial (OAT). Am Heart J 2005150627–642. [DOI] [PubMed] [Google Scholar]
- 18.Dzavik V, Buller C E, Lamas G A.et al Randomized trial of percutaneous coronary intervention for subacute infarct‐related coronary artery occlusion to achieve long‐term patency and improve ventricular function: the Total Occlusion Study of Canada (TOSCA)‐2 trial. Circulation 20061142449–2457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Antman E M, Anbe D T, Armstrong P W.et al ACC/AHA guidelines for the management of patients with ST‐elevation myocardial infarction; a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Revise the 1999 Guidelines for the Management of patients with acute myocardial infarction). J Am Coll Cardiol 200444E1–211. [DOI] [PubMed] [Google Scholar]
- 20.Kastrati A, Mehilli J, Pache J.et al Analysis of 14 trials comparing sirolimus‐eluting stents with bare‐metal stents. N Engl J Med 20073561030–1039. [DOI] [PubMed] [Google Scholar]
- 21.Lagerqvist B, James S K, Stenestrand U.et al Long‐term outcomes with drug‐eluting stents versus bare‐metal stents in Sweden. N Engl J Med 20073561009–1019. [DOI] [PubMed] [Google Scholar]
- 22.Spaulding C, Daemen J, Boersma E.et al A pooled analysis of data comparing sirolimus‐eluting stents with bare‐metal stents. N Engl J Med 2007356989–997. [DOI] [PubMed] [Google Scholar]
- 23.Stone G W, Moses J W, Ellis S G.et al Safety and efficacy of sirolimus‐ and paclitaxel‐eluting coronary stents. N Engl J Med 2007356998–1008. [DOI] [PubMed] [Google Scholar]
- 24.Hochman J S, Sleeper L A, Webb J G.et al Early revascularization in acute myocardial infarction complicated by cardiogenic shock. SHOCK investigators. Should we emergently revascularize occluded coronaries for cardiogenic shock. N Engl J Med 1999341625–634. [DOI] [PubMed] [Google Scholar]
- 25.Boden W E, O'Rourke R A, Teo K K.et al Optimal medical therapy with or without PCI for stable coronary disease. N Engl J Med 20073561503–1516. [DOI] [PubMed] [Google Scholar]