Abstract
Objective
To study gender differences in management and outcome in patients with non‐ST‐elevation acute coronary syndrome.
Design, setting and patients
Cohort study of 53 781 consecutive patients (37% women) from the Register of Information and Knowledge about Swedish Heart Intensive care Admissions (RIKS‐HIA), with a diagnosis of either unstable angina pectoris or non‐ST‐elevation myocardial infarction. All patients were admitted to intensive coronary care units in Sweden, between 1998 and 2002, and followed for 1 year.
Main outcome measures
Treatment intensity and in‐hospital, 30‐day and 1‐year mortality.
Results
Women were older (73 vs 69 years, p<0.001) and more likely to have a history of hypertension and diabetes, but less likely to have a history of myocardial infarction or revascularisation. After adjustment, there were no major differences in acute pharmacological treatment or prophylactic medication at discharge.
Revascularisation was, however, even after adjustment, performed more often in men (OR 1.15; 95% CI, 1.09 to 1.21). After adjustment, there was no significant difference in in‐hospital (OR 1.03; 95% CI, 0.94 to 1.13) or 30‐days (OR 1.07; 95% CI, 0.99 to 1.15) mortality, but at 1 year being male was associated with higher mortality (OR 1.12; 95% CI, 1.06 to 1.19).
Conclusion
Although women are somewhat less intensively treated, especially regarding invasive procedures, after adjustment for differences in background characteristics, they have better long‐term outcomes than men.
Since the beginning of the 1990s there have been numerous studies on gender differences in management of acute coronary syndromes (ACS). Many earlier studies,1,2,3,4,5,6,7,8 but not all,9 found that women were treated less intensively in the acute phase. In some of the studies, after adjustment for age, comorbidity and severity of the disease, most of the differences disappeared.6,7 There is also conflicting evidence on gender differences in evidence‐based treatment at discharge.1,3,5,6,8,10,11
After acute myocardial infarction (AMI), a higher short‐term mortality in women is documented in several studies.2,5,6,7,12,13,14 After adjustment for age and comorbidity some difference has usually,2,5,12,13 but not always,11,14 remained. On the other hand, most studies assessing long‐term outcome have found no difference between the genders, or a better outcome in women, at least after adjustment.7,10,13,14 Earlier studies focusing on gender differences in outcome after an acute coronary syndrome have usually studied patients with AMI, including both ST‐elevation myocardial infarction and non‐ST‐elevation myocardial infarction (NSTEMI).2,5,6,7,12,13,14 However, the pathophysiology and initial management differs between these two conditions,15 as does outcome according to gender.11,16 In patients with NSTEMI or unstable angina pectoris (UAP), women seem to have an equal or better outcome, after adjustment for age and comorbidity.1,4,8,11,16,17 Studies on differences between genders, in treatment and outcome, in real life, contemporary, non‐ST‐elevation acute coronary syndrome (NSTE ACS) populations, large enough to make necessary adjustments for confounders, are lacking.
The aim of this study was to assess gender differences in background characteristics, management and outcome in a real‐life intensive coronary care unit (ICCU) population, with NSTE ACS.
Methods
Study population
The Register of Information and Knowledge about Swedish Heart Intensive Care Admissions (RIKS‐HIA) registers all patients admitted to the intensive coronary care units of participating hospitals. Information is reported on case record forms. On admission 30 variables are recorded including age, gender, risk factors, medical history, previous medications, symptoms and ECG findings. During the hospital stay another 37 variables are recorded regarding biochemical markers, treatments, investigations and major complications. At discharge, a further 33 variables are recorded, including outcomes during the hospital stay, and medications and diagnosis at discharge. The complete protocol is available online (http://www.riks‐hia.se).
Standardised criteria for the diagnosis of acute myocardial infarction and unstable angina according to WHO were used by all participating centres.18 Biochemical criteria were revised during the study period in accordance with the ESC/ACC consensus document.19 Finally, diagnoses were coded according to the International Classification of Diseases, version 10, at the treating physician's discretion.
The register started in 1995 with 19 participating hospitals and has increased gradually to 46 hospitals in 1997 and 70 of 78 hospitals in 2002. This means that in 2002 about 95% of all ICCU admissions in Sweden were covered.
Source data have continuously been validated by comparison of the register information with the hospitals' patient records by an external monitor. In 1972 computer forms from 38 hospitals comprising 161 280 data points, there was 94% overall agreement between registered information and the source data in patients' records.
Data on mortality were obtained by merging the RIKS‐HIA register with the Swedish National Cause of Death Register. Previous history of congestive heart failure, stroke, dementia, cancer, chronic obstructive pulmonary disease and renal failure were obtained by merging the RIKS‐HIA register with the National Patient Register, which comprises all diagnoses of patients hospitalised in Sweden from 1987 onwards.
Data presented in this paper were obtained from 5 years between 1998 and 2002. All patients with a discharge diagnosis of AMI or UAP were included. Patients with ST‐segment elevation or left bundle branch block on admission rest‐ECG were excluded. Also patients treated with thrombolysis or primary percutaneous coronary intervention (PCI) were excluded. Finally, only the first time an individual appeared in the register with NSTEMI or UAP was included for analysis.
Ethics approval
The RIKS‐HIA register and the process of merging with other registries were approved by the Swedish Data Inspection Board. This study complies with the Declaration of Helsinki and was approved by the local ethics committee.
Statistical analysis
Group differences based on continuous variables were assessed using the t test and differences based on categorical variables were assessed using the χ2 test.
Gender differences in background characteristics were assessed with logistic regression analysis. In the first model gender was included as the sole independent variable. In the second model gender and age were included. Differences between the genders in performed procedures, pharmacological treatment, both acute and at discharge, and outcome were assessed in the same way. To further adjust for differences in background characteristics a third logistic regression model was created which included 23 covariates: age, gender, smoking status, previous myocardial infarction, PCI or coronary artery bypass grafting, history of hypertension, diabetes, congestive heart failure, renal failure, stroke, chronic obstructive pulmonary disease or malignant disease, information on medical treatment before admission (including ACE inhibitors, aspirin, oral anticoagulants, heparin, low molecular weight heparin, β‐blockers, long‐acting nitroglycerine, lipid‐lowering drugs, digitalis and diuretics), ST‐segment depression on admission, cardiopulmonary resuscitation immediately before admission and marked elevation of biochemical markers (defined as creatine kinase muscle/brain (CKMB)⩾10 μg/l or troponin T (TnT)⩾0.1 μg/l).
Age distribution differs markedly between the genders. To further study the importance of age on differences in management, treatments and procedures were assessed in four age strata.
To identify differences in outcome between the genders during 1‐year follow‐up, hazard ratios were calculated in four different age intervals, using Cox regression survival analysis, with the same covariates included as in the logistic regression analysis.
All statistical analyses were performed using SPSS version 13.0 software.
Results
Between 1998 and 2002, 53 781 patients with a discharge diagnosis of either NSTEMI or UAP were included in this study. Women constituted 37% (n = 19 761) of the population. Women were older than men (73 vs 69 years, p<0.001). There were only minor differences between the genders in the proportion of patients diagnosed as NSTEMI (72% vs 73%), and in the proportion of patients with elevated biochemical markers (79% vs 79%) (table 1).
Table 1 Baseline characteristics.
| Men (n = 34 020) | Women (n = 19 761) | Unadjusted OR (95% CI) | Age‐adjusted OR* (95% CI) | |
|---|---|---|---|---|
| Age, mean (SD),years | 69 (12) | 73 (11) | – | – |
| Risk factors | ||||
| Hypertension | 35 | 43 | 0.71 (0.69–0.74) | 0.74 (0.71–0.77) |
| Diabetes | 21 | 24 | 0.84 (0.80–0.87) | 0.86 (0.82–0.89) |
| Current smoker | 21 | 17 | 1.28 (1.22–1.34) | 0.96 (0.91–1.01) |
| History of MI | 36 | 30 | 1.27 (1.23–1.32) | 1.44 (1.38–1.49) |
| History of PCI | 9 | 6 | 1.56 (1.45–1.68) | 1.35 (1.26–1.45) |
| History of CABG | 9 | 5 | 1.97 (1.83–2.13) | 1.94 (1.79–2.09) |
| Medical treatment before admission | ||||
| ACE inhibitor | 21 | 21 | 0.99 (0.94–1.03) | 1.03 (0.99–1.08) |
| Aspirin/other thrombocyte inhibitor | 53 | 52 | 1.04 (1.01–1.08) | 1.15 (1.11–1.20) |
| Oral anticoagulant | 6 | 5 | 1.21 (1.12–1.31) | 1.36 (1.25–1.47) |
| β‐blocker | 46 | 47 | 0.95 (0.92–0.98) | 0.97 (0.93–1.00) |
| Digitalis | 7 | 10 | 0.69 (0.64–0.73) | 0.89 (0.83–0.95) |
| Diuretic | 26 | 41 | 0.50 (0.49–0.52) | 0.63 (0.60–0.65) |
| Long‐acting nitroglycerine | 29 | 31 | 0.88 (0.85–0.92) | 1.04 (0.99–1.08) |
| Lipid‐lowering therapy | 22 | 19 | 1.23 (1.18–1.29) | 1.06 (1.01–1.11) |
| Medical history | ||||
| Stroke | 12 | 12 | 1.02 (0.97–1.08) | 1.27 (1.20–1.35) |
| Renal failure | 1.9 | 1.3 | 1.44 (1.25–1.66) | 1.56 (1.35–1.80) |
| COPD | 6 | 7 | 0.78 (0.72–0.83) | 0.86 (0.80–0.93) |
| Dementia | 0.2 | 0.4 | 0.52 (0.38–0.71) | 0.68 (0.50–0.93) |
| Heart failure | 13 | 17 | 0.72 (0.68–0.75) | 0.93 (0.88–0.98) |
| Cancer diagnosed last 3 years | 4.8 | 3.8 | 1.26 (1.15–1.37) | 1.50 (1.37–1.64) |
| Ischaemic signs | ||||
| ST depression† | 34 | 38 | 0.83 (0.80–0.86) | 0.95 (0.92–0.99) |
| Marker elevation (n = 47 348)§ | ||||
| CKMB⩾5 μg/l / TnT⩾0.06 μg/l | 79 | 79 | 1.02 (0.99–1.06) | 1.16 (1.11–1.21) |
| CKMB⩾10 μg/l / TnT⩾0.1 μg/l | 72 | 71 | 1.05 (1.01–1.09) | 1.20 (1.15–1.25) |
| Diagnosis at discharge | ||||
| NSTEMI | 72 | 73 | 0.91 (0.88–0.95) | 1.09 (1.05–1.14) |
| UAP | 29 | 27 | 1.10 (1.05–1.14) | 0.92 (0.88–0.96) |
Data are presented as percentages unless otherwise indicated.
CABG, coronary artery bypass grafting; CKMB, creatine kinase muscle/brain; COPD, chronic obstructive pulmonary disease; MI, myocardial infarction; PCI, percutaneous coronary intervention; NSTEMI, non‐ST‐elevation myocardial infarction; TnT, troponin T; UAP, unstable angina pectoris.
*Odds ratios were obtained by logistic regression analysis and presented for men vs women.
†ST‐segment depression was defined as ⩾1 mm depression of the ST‐segment in ⩾2 leads, on admission ECG.
§Valid values for CKMB or TnT were available in 88% of the cases. Different troponin I methods or CKB were used otherwise.
Management
Before adjustment men were more often treated with heparin/low molecular weight heparin (LMWH) and GPIIb/IIIa inhibitor during hospital stay, and with aspirin, β‐blockers and lipid‐lowering drugs at discharge. Men were also more likely to have a stress test, echocardiography, coronary angiography, PCI and coronary artery bypass grafting (CABG) performed (table 2).
Table 2 Procedures, treatments and outcome.
| Men (%) (n = 34 020) | Women (%) (n = 19 761) | OR* before adjustment (95% CI) | OR* after age‐adjustment (95% CI) | OR* after multiple adjustment† (95% CI) | |
|---|---|---|---|---|---|
| Treatment | |||||
| Heparin/LMWH | 59 | 56 | 1.11 (1.07–1.15) | 1.02 (0.98–1.06) | 1.02 (0.98–1.07) |
| Nitroglycerin iv | 32 | 32 | 1.00 (0.96–1.03) | 0.99 (0.96–1.03) | 0.98 (0.94–1.03) |
| GPIIb/IIIa inhibitor | 6 | 4 | 1.43 (1.31–1.56) | 1.22 (1.11–1.34) | 1.18 (1.07–1.30) |
| Procedures‡ | |||||
| Stress test | 28 | 20 | 1.56 (1.50–1.63) | 1.31 (1.25–1.37) | 1.34 (1.27–1.40) |
| Echocardiography | 44 | 40 | 1.17 (1.13–1.21) | 1.10 (1.06–1.14) | 1.11 (1.06–1.15) |
| Coronary angiography | 37 | 29 | 1.44 (1.38–1.49) | 1.12 (1.07–1.16) | 1.10 (1.05–1.15) |
| PCI | 18 | 14 | 1.35 (1.28–1.42) | 1.07 (1.02–1.13) | 1.03 (0.97–1.09) |
| CABG | 7 | 5 | 1.55 (1.43–1.68) | 1.40 (1.29–1.52) | 1.43 (1.31–1.57) |
| PCI/CABG | 24 | 18 | 1.45 (1.38–1.51) | 1.17 (1.11–1.22) | 1.15 (1.09–1.21) |
| Medication at discharge | |||||
| ACE inhibitor | 37 | 36 | 1.04 (1.00–1.07) | 1.10 (1.06–1.14) | 1.13 (1.07–1.19) |
| Aspirin/other thrombocyte inhibitor | 88 | 85 | 1.22 (1.15–1.28) | 1.04 (0.98–1.09) | 1.02 (0.96–1.09) |
| β‐blocker | 82 | 78 | 1.23 (1.17–1.28) | 1.04 (1.00–1.09) | 1.06 (1.00–1.12) |
| Lipid‐lowering drugs | 51 | 45 | 1.30 (1.25–1.35) | 0.99 (0.95–1.03) | 0.98 (0.94–1.03) |
| Mortality (all‐cause) | |||||
| In‐hospital | 5 | 7 | 0.74 (0.69–0.80) | 1.03 (0.96–1.11) | 1.03 (0.94–1.13) |
| 30 days | 7 | 9 | 0.76 (0.71–0.81) | 1.05 (0.98–1.12) | 1.07 (0.99–1.15) |
| 1 year | 16 | 19 | 0.77 (0.74–0.81) | 1.11 (1.05–1.16) | 1.12 (1.06–1.19) |
Data are given as percentages unless otherwise indicated.
CABG, coronary artery bypass grafting; GPIIb/IIIa, glycoprotein IIb/IIIa; LMWH, low molecular weight heparin; PCI, percutaneous coronary intervention;
*Odds ratios were obtained by logistic regression analysis and presented as OR for men vs women.
†Multivariate logistic regression model with adjustment for age, gender, smoking status, previous myocardial infarction, PCI or CABG, history of hypertension, diabetes, congestive heart failure, renal failure, stroke, chronic obstructive pulmonary disease or malignant disease during last 3 years, information on medical treatment before admission (including ACE inhibitors, aspirin, oral anticoagulants, heparin, LMWH, β‐blockers, long‐acting nitroglycerine, lipid‐lowering drugs, digitalis and diuretics), ST‐segment depression on admission, cardiopulmonary resuscitation immediately before admission and elevation of biochemical markers (defined as CKMB⩾10 μg/l or TnT⩾0.1 μg/l).
‡Performed during hospital stay.
After adjustment for differences in age, there remained no significant differences in pharmacological treatments, except for treatment with GPIIb/IIIa inhibitors and ACE inhibitors at discharge, which were more often used in men. However, age‐adjusted odds ratios for procedure use, such as stress tests, echocardiography, coronary angiography, PCI and CABG, were all higher in men. Further adjustment with another 21 covariates did not change these associations except that there remained no significant difference in PCI rates (table 2).
We also assessed gender differences at different ages by stratifying the population in four age groups. There were marked differences in treatments and procedure use according to age, while differences between men and women within each age group were comparably small. Cardiac procedures were, however, generally used less often in women (table 3).
Table 3 Treatments and procedures according to gender, stratified in age intervals.
| ⩽59 years | 60–69 years | 70–79 years | ⩾80 years | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M (n = 7893) | W (n = 2621) | p Value | M (n = 8326) | W (n = 3654) | p Value | M (n = 11 216) | W (n = 6939) | p Value | M (n = 6585) | W (n = 6547) | p Value | |
| Acute treatment | ||||||||||||
| Heparin/LMWH | 64 | 64 | 0.70 | 63 | 63 | 0.67 | 58 | 58 | 0.94 | 49 | 48 | 0.27 |
| Nitroglycerin iv | 31 | 32 | 0.28 | 33 | 33 | 0.60 | 32 | 33 | 0.21 | 32 | 30 | 0.10 |
| GPIIb/IIIa inhibitor | 9 | 8 | 0.07 | 7 | 6 | 0.006 | 5 | 4 | 0.18 | 3 | 2 | 0.02 |
| Procedures* | ||||||||||||
| Stress test | 36 | 35 | 0.18 | 35 | 31 | <0.001 | 27 | 22 | <0.001 | 9 | 4 | <0.001 |
| Echocardiography | 47 | 43 | <0.001 | 46 | 45 | 0.28 | 45 | 45 | 0.53 | 35 | 31 | <0.001 |
| Coronary angiography | 54 | 53 | 0.37 | 46 | 45 | 0.17 | 32 | 30 | 0.003 | 10 | 8 | <0.001 |
| PCI | 30 | 26 | <0.001 | 22 | 22 | 0.96 | 13 | 14 | 0.25 | 4 | 4 | 0.26 |
| CABG | 7 | 6 | <0.001 | 9 | 7 | <0.001 | 7 | 6 | <0.001 | 2 | 1 | <0.001 |
| Medication at discharge | ||||||||||||
| ACE inhibitor | 30 | 25 | <0.001 | 37 | 34 | 0.002 | 41 | 40 | 0.10 | 37 | 37 | 0.65 |
| Aspirin/other thrombocyte inhibitor | 93 | 93 | 0.13 | 90 | 91 | 0.19 | 86 | 85 | 0.31 | 81 | 80 | 0.05 |
| β‐blocker | 89 | 86 | <0.001 | 86 | 85 | 0.06 | 80 | 80 | 0.66 | 70 | 70 | 0.82 |
| Lipid‐lowering drugs | 71 | 63 | <0.001 | 64 | 66 | 0.03 | 46 | 49 | <0.001 | 19 | 19 | 0.27 |
Data are given as percentages unless otherwise indicated.
CABG, coronary artery bypass grafting; GPIIb/IIIa, glycoprotein IIb/IIIa; LMWH, low molecular weight heparin; M, men; PCI, percutaneous coronary intervention; W, women.
*Performed during hospital stay.
Outcome
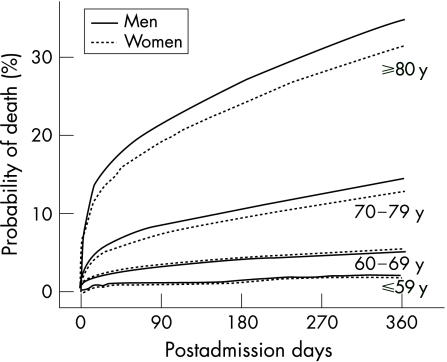
Crude short‐term and long‐term mortality were higher in women. However, after adjustment for age, there was no difference in mortality during hospital stay or at 30 days. At 1 year female gender was even associated with a lower mortality. This association persisted after including a further 21 covariates in a multivariate logistic regression analysis (table 2). Adding year of enrolment to the covariates did not change the results. We assessed all‐cause mortality as the main outcome measure, but there was no important difference between men and women in the proportion of cardiovascular cause of death during hospital stay (89% vs 90%), at 30 days (89% vs 89%) or at 1 year (82% vs 84%). When 1‐year mortality was calculated in a Cox regression analysis, with extensive adjustment for covariates, and presented in four age strata, we found no significant differences between men and women in patients younger than 70 years. In patients older than 70 years the relative risk of death at 1 year was significantly higher in men (fig 1).
Figure 1 Adjusted 1‐year mortality. Abbreviation: y, years. Hazard ratios (HR) were calculated using Cox regression analysis. For information on covariates, see Methods. HR at 1 year: ⩽59 years, HR = 1.12 (95% CI 0.85 to 1.47); 60–69 years, HR = 0.99 (95% CI 0.85 to 1.16); 70–79 years, HR = 1.14 (95% CI 1.05 to 1.23); ⩾80 years HR = 1.13 (95% CI 1.05 to 1.20).
Discussion
This prospective cohort study of consecutively hospitalised patients with NSTE ACS, in a contemporary ICCU setting, revealed significant differences in both background characteristics and management between men and women. This large cohort covers almost all patients with NSTE ACS treated at ICCUs in Sweden between 1998 and 2002. Most of the differences in management were due to the observed differences in background characteristics, especially age. However, even after adjustment, cardiac procedures were used less often in women than in men. While crude outcomes were worse in women, adjustment revealed that female gender was associated with lower long‐term mortality.
The women in this study were older than the men, were more likely to have hypertension, diabetes and a history of congestive heart failure, and were less likely to have a history of myocardial infarction or revascularisation, which is in agreement with earlier studies on patients with ACS.1,3,5,6,7,8,10,16,17,20,21,22 After adjustment for age there were no differences between men and women in treatment before admission, with ACE inhibitors, β‐blockers, calcium channel blockers or long‐acting nitroglycerin, which is in agreement with earlier findings.1,20 However, more men were treated with aspirin and lipid‐lowering drugs and women were more likely to be treated with digitalis and diuretics, which probably reflects the higher occurrence of a history of an AMI in men and of hypertension and congestive heart failure in women.
In this study, after adjustment, we found no differences in medical treatment, except for higher use of GPII/bIIIa inhibitors and ACE inhibitors in men. Data on medical treatment in a population with NSTE ACS are scarce, but Stone et al.1 reported from the TIMI (Thrombolysis In Myocardial Ischemia) III registry of patients with UAP or non‐Q‐wave AMI, that women were less likely to receive heparin and intravenous nitroglycerin in the acute phase, as well as aspirin at discharge, even after adjustment for age. Recently, Blomkalns et al.8 reported from the CRUSADE (Can Rapid Risk Stratification of Unstable Angina Patients Suppress Adverse Outcomes With Early Implementation of the American College of Cardiology/American Heart Association Guidelines) National Quality Improvement Initiative, that, even after adjustment, women were less often treated with heparin/LMWH and GPIIb/IIIa inhibitors in the acute phase, and less often received aspirin, ACE inhibitor and statins. In our data from Swedish ICCUs the differences between the genders in pharmacological treatment are small, and less than in earlier reports.
Age distribution differs markedly between the genders, and since it has been shown that, among patients with AMI especially, young women seem to fare worse than their male counterparts,22,23,24 we also assessed treatments and use of procedures, stratifying the data in four age groups. We then found marked differences in treatments according to age, while there were only small differences between men and women within each age group, and the observed differences were not consistent according to gender. However, in the youngest age group, fewer women received prophylactic medication at discharge, which might be explained by actual differences between the genders in left ventricular function and cholesterol values.
In our study stress test, echocardiography, coronary angiography, PCI or CABG were performed less often in women, even after adjustment for age. After adjustment for age and other comorbidities, there remained no significant difference in PCI rate, but there was still a lower rate of CABG in women. These findings parallel findings in earlier reports on patients with UAP.1,4,17
In FRISC II (FRagmin and Fast Revascularisation during InStability in Coronary artery disease), a randomised controlled clinical trial comparing early invasive and non‐invasive strategy in NSTE ACS patients, a significant benefit with an early invasive strategy could be shown for men, but not for women.25,26 There is still conflicting evidence regarding the benefit of an early invasive strategy in women with NSTE ACS, and caution is needed in the interpretation of differences found in subgroup analyses. While post‐hoc analysis of RITA 3, (Randomized Intervention Trial of unstable Angina) according to gender, supported the results from FRISC II, with no benefit of an invasive strategy in women, TACTICS TIMI‐18 (Treat Angina with Aggrastat and determine Cost of Therapy with an Invasive or Conservative Strategy) and ICTUS (Invasive versus Conservative Treatment in Unstable coronary Syndromes) indicated similar results in men and women.25,26,27,28 In the present study, more men than women were investigated with coronary angiography and treated with CABG, while PCI rates were equal between the genders, after adjustment for age and comorbidities. These findings go along with earlier findings of less severe coronary artery disease in women in a population with NSTE ACS.25,26,28 Although crude mortality was higher in women, adjustment for age revealed that there was no difference between the genders in in‐hospital or 30‐day mortality, and at 1 year, male gender was associated with 11% higher odds for death. The finding that women, in spite of less intensive treatment, have a better outcome may appear contradictory. However, in both FRISC II and RITA 3 there was no evidence for a beneficial effect of an early invasive strategy in women, in contrast to in men.25,26,28 Earlier studies on patients with NSTE ACS, have shown that a larger proportion of men than women have significant coronary artery stenoses on an angiogram.25,26,28 Hence the differences between the genders in underlying degree of coronary artery disease could also contribute to the findings and even implicate undertreatment in men, where there is evidence of a beneficial effect with an invasive strategy in moderate to high‐risk patients. Another reason for a less beneficial effect of an invasive strategy in women could be a higher risk for death or MI, for women compared to men, associated with CABG.25,26
The impression of different interactions between treatments and outcomes in relation to gender raises questions over whether there are true differences in the effects of different treatment strategies according to gender, the importance of underlying differences in pathophysiology and comorbidity on treatment strategy and the possibility of identifying the most appropriate treatment strategy according to gender. These results also emphasise the need for further studies, with sufficient numbers of both women and men, to identify optimal, evidence‐based treatment strategies for both genders.
Study limitations
A major limitation of this observational study is that, although data have been adjusted for many confounding variables, it is not possible to adjust for variables not included in the register. Information on indications for treatments, such as information on cholesterol, low‐density lipoprotein levels and left ventricular function, were optional in the register and available for only 20–30% of the patients. Accordingly, these variables were not included as covariates. Contraindications for specific treatments were not registered. Regarding differences between the genders in revasculariation rates, the proportion of patients with significant stenoses on the angiogram were not registered and hence could not be taken into account. It is well known that patients with NSTE ACS, and especially older patients, are treated not only in ICCUs, but also in general wards. We have therefore designed and carried out a study including all patients admitted to general wards with a suspected ACS. These data are currently being analysed.
A strength of this registry study is that it is based on a large cohort, which made necessary adjustments possible and it reflects real‐world management strategies.
Conclusion
Although men are managed somewhat more intensively, especially concerning invasive procedures, after adjustment they have higher long‐term mortality.
The optimal treatment recommendations for men and women respectively can only be resolved by inclusion of sufficient numbers of both women and men in future clinical trials.
Acknowledgements
We acknowledge all participating hospitals for their help and cooperation to contribute with data to RIKS‐HIA. We also acknowledge Max Köster at the National Board of Health and Welfare in Stockholm, for help with merging the databases. The RIKS‐HIA register is supported by grants from the Swedish Heart‐Lung Foundation, the Federation of Swedish County Councils, and the National Board of Health and Welfare. This study was supported by grants from the Medical Research Council of Southeast Sweden.
The Swedish Heart‐Lung Foundation, the Federation of Swedish County Councils, the National Board of Health and Welfare and the Medical Research Council of Southeast Sweden had no role in the collection, management, analysis or interpretation of the data, or the preparation, review or approval of the manuscript.
Abbreviations
CRUSADE - Can Rapid Risk Stratification of Unstable Angina Patients Suppress Adverse Outcomes With Early Implementation of the American College of Cardiology/American Heart Association Guidelines
FRISC II - FRagmin and fast revascularisation during InStability in Coronary artery disease
ICTUS - Invasive versus Conservative Treatment in Unstable coronary Syndromes
RIKS‐HIA - Register of Information and Knowledge about Swedish Heart Intensive care Admissions
RITA 3 - Randomized Intervention Trial of unstable Angina
TACTICS TIMI‐18 - Treat Angina with Aggrastat and determine Cost of Therapy with an Invasive or Conservative Strategy
Footnotes
Competing interests: None declared.
References
- 1.Stone P H, Thompson B, Anderson H V.et al Influence of race, sex, and age on management of unstable angina and non‐Q‐wave myocardial infarction: the TIMI III registry. JAMA 19962751104–1112. [PubMed] [Google Scholar]
- 2.Chandra N C, Ziegelstein R C, Rogers W J.et al Observations of the treatment of women in the United States with myocardial infarction: a report from the National Registry of Myocardial Infarction‐I. Arch Intern Med 1998158981–988. [DOI] [PubMed] [Google Scholar]
- 3.Scirica B M, Moliterno D J, Every N R.et al Differences between men and women in the management of unstable angina pectoris (The GUARANTEE Registry). The GUARANTEE Investigators. Am J Cardiol 1999841145–1150. [DOI] [PubMed] [Google Scholar]
- 4.Roger V L, Farkouh M E, Weston S A.et al Sex differences in evaluation and outcome of unstable angina. JAMA 2000283646–652. [DOI] [PubMed] [Google Scholar]
- 5.Gan S C, Beaver S K, Houck P M.et al Treatment of acute myocardial infarction and 30‐day mortality among women and men. N Engl J Med 20003438–15. [DOI] [PubMed] [Google Scholar]
- 6.Mahon N G, McKenna C J, Codd M B.et al Gender differences in the management and outcome of acute myocardial infarction in unselected patients in the thrombolytic era. Am J Cardiol 200085921–926. [DOI] [PubMed] [Google Scholar]
- 7.Gottlieb S, Harpaz D, Shotan A.et al Sex differences in management and outcome after acute myocardial infarction in the 1990s: a prospective observational community‐based study. Israeli Thrombolytic Survey Group. Circulation 20001022484–2490. [DOI] [PubMed] [Google Scholar]
- 8.Blomkalns A L, Chen A Y, Hochman J S.et al Gender disparities in the diagnosis and treatment of non‐ST‐segment elevation acute coronary syndromes: large‐scale observations from the CRUSADE (Can Rapid Risk Stratification of Unstable Angina Patients Suppress Adverse Outcomes With Early Implementation of the American College of Cardiology/American Heart Association Guidelines) National Quality Improvement Initiative. J Am Coll Cardiol 200545832–837. [DOI] [PubMed] [Google Scholar]
- 9.Raine R A, Black N A, Bowker T J.et al Gender differences in the management and outcome of patients with acute coronary artery disease. J Epidemiol Community Health 200256791–797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mehilli J, Kastrati A, Dirschinger J.et al Sex‐based analysis of outcome in patients with acute myocardial infarction treated predominantly with percutaneous coronary intervention. JAMA 2002287210–215. [DOI] [PubMed] [Google Scholar]
- 11.Hasdai D, Porter A, Rosengren A.et al Effect of gender on outcomes of acute coronary syndromes. Am J Cardiol 2003911466–9, A6. [DOI] [PubMed] [Google Scholar]
- 12.Marrugat J, Sala J, Masia R.et al Mortality differences between men and women following first myocardial infarction. RESCATE Investigators. Recursos Empleados en el Sindrome Coronario Agudo y Tiempo de Espera. JAMA 19982801405–1409. [DOI] [PubMed] [Google Scholar]
- 13.Maynard C, Every N R, Martin J S.et al Association of gender and survival in patients with acute myocardial infarction. Arch Intern Med 19971571379–1384. [PubMed] [Google Scholar]
- 14.Moen E K, Asher C R, Miller D P.et al Long‐term follow‐up of gender‐specific outcomes after thrombolytic therapy for acute myocardial infarction from the GUSTO‐I trial. Global Utilization of Streptokinase and Tissue Plasminogen Activator for Occluded Coronary Arteries. J Womens Health 19976285–293. [DOI] [PubMed] [Google Scholar]
- 15.Braunwald E, Antman E M, Beasley J W.et al ACC/AHA 2002 guideline update for the management of patients with unstable angina and non‐ST‐segment elevation myocardial infarction summary article: a report of the American College of Cardiology/American Heart Association task force on practice guidelines (Committee on the Management of Patients With Unstable Angina). J Am Coll Cardiol 2002401366–1374. [DOI] [PubMed] [Google Scholar]
- 16.Hochman J S, Tamis J E, Thompson T D.et al Sex, clinical presentation, and outcome in patients with acute coronary syndromes. Global Use of Strategies to Open Occluded Coronary Arteries in Acute Coronary Syndromes IIb Investigators. N Engl J Med 1999341226–232. [DOI] [PubMed] [Google Scholar]
- 17.Kim C, Schaaf C H, Maynard C.et al Unstable angina in the myocardial infarction triage and intervention registry (MITI): short‐ and long‐term outcomes in men and women. Am Heart J 200114173–77. [DOI] [PubMed] [Google Scholar]
- 18.Tunstall‐Pedoe H, Kuulasmaa K, Amouyel P.et al Myocardial infarction and coronary deaths in the World Health Organization MONICA Project. Registration procedures, event rates, and case‐fatality rates in 38 populations from 21 countries in four continents. Circulation 199490583–612. [DOI] [PubMed] [Google Scholar]
- 19.Anonymous Myocardial infarction redefined: a consensus document of The Joint European Society of Cardiology/American College of Cardiology Committee for the redefinition of myocardial infarction. Eur Heart J 2000211502–1513. [DOI] [PubMed] [Google Scholar]
- 20.Hochman J S, McCabe C H, Stone P H.et al Outcome and profile of women and men presenting with acute coronary syndromes: a report from TIMI IIIB. TIMI Investigators. Thrombolysis in Myocardial Infarction. J Am Coll Cardiol 199730141–148. [DOI] [PubMed] [Google Scholar]
- 21.Heer T, Schiele R, Schneider S.et al Gender differences in acute myocardial infarction in the era of reperfusion (the MITRA registry). Am J Cardiol 200289511–517. [DOI] [PubMed] [Google Scholar]
- 22.Vaccarino V, Parsons L, Every N R.et al Sex‐based differences in early mortality after myocardial infarction. National Registry of Myocardial Infarction 2 Participants. N Engl J Med 1999341217–225. [DOI] [PubMed] [Google Scholar]
- 23.Vaccarino V, Krumholz H M, Yarzebski J.et al Sex differences in 2‐year mortality after hospital discharge for myocardial infarction. Ann Intern Med 2001134173–181. [DOI] [PubMed] [Google Scholar]
- 24.Rosengren A, Spetz C L, Koster M.et al Sex differences in survival after myocardial infarction in Sweden; data from the Swedish National Acute Myocardial Infarction Register. Eur Heart J 200122314–322. [DOI] [PubMed] [Google Scholar]
- 25.Lagerqvist B, Safstrom K, Stahle E.et al Is early invasive treatment of unstable coronary artery disease equally effective for both women and men? FRISC II Study Group Investigators. J Am Coll Cardiol 20013841–48. [DOI] [PubMed] [Google Scholar]
- 26.Clayton T C, Pocock S J, Henderson R A.et al Do men benefit more than women from an interventional strategy in patients with unstable angina or non‐ST‐elevation myocardial infarction? The impact of gender in the RITA 3 trial. Eur Heart J 2004251641–1650. [DOI] [PubMed] [Google Scholar]
- 27.de Winter R J, Windhausen F, Cornel J H.et al Early invasive versus selectively invasive management for acute coronary syndromes. N Engl J Med 20053531095–1104. [DOI] [PubMed] [Google Scholar]
- 28.Glaser R, Herrmann H C, Murphy S A.et al Benefit of an early invasive management strategy in women with acute coronary syndromes. JAMA 20022883124–3129. [DOI] [PubMed] [Google Scholar]