Abstract
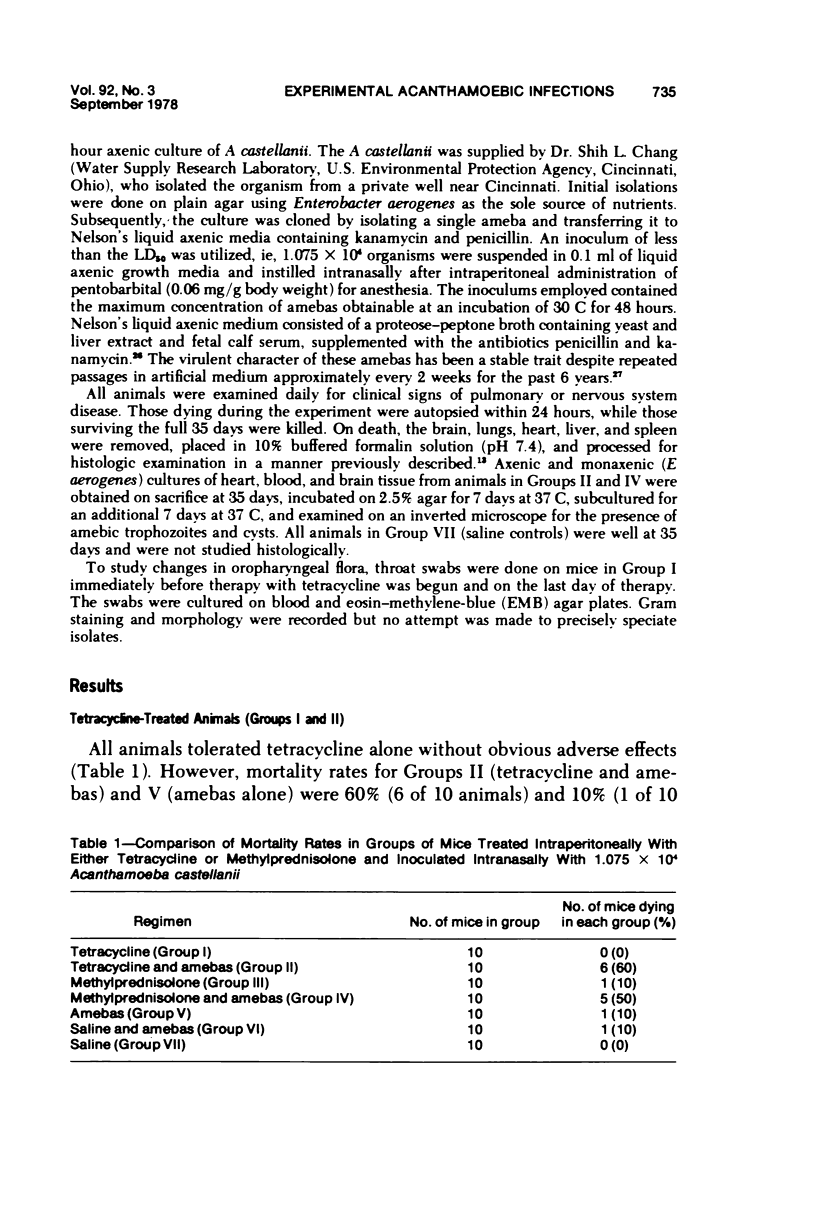
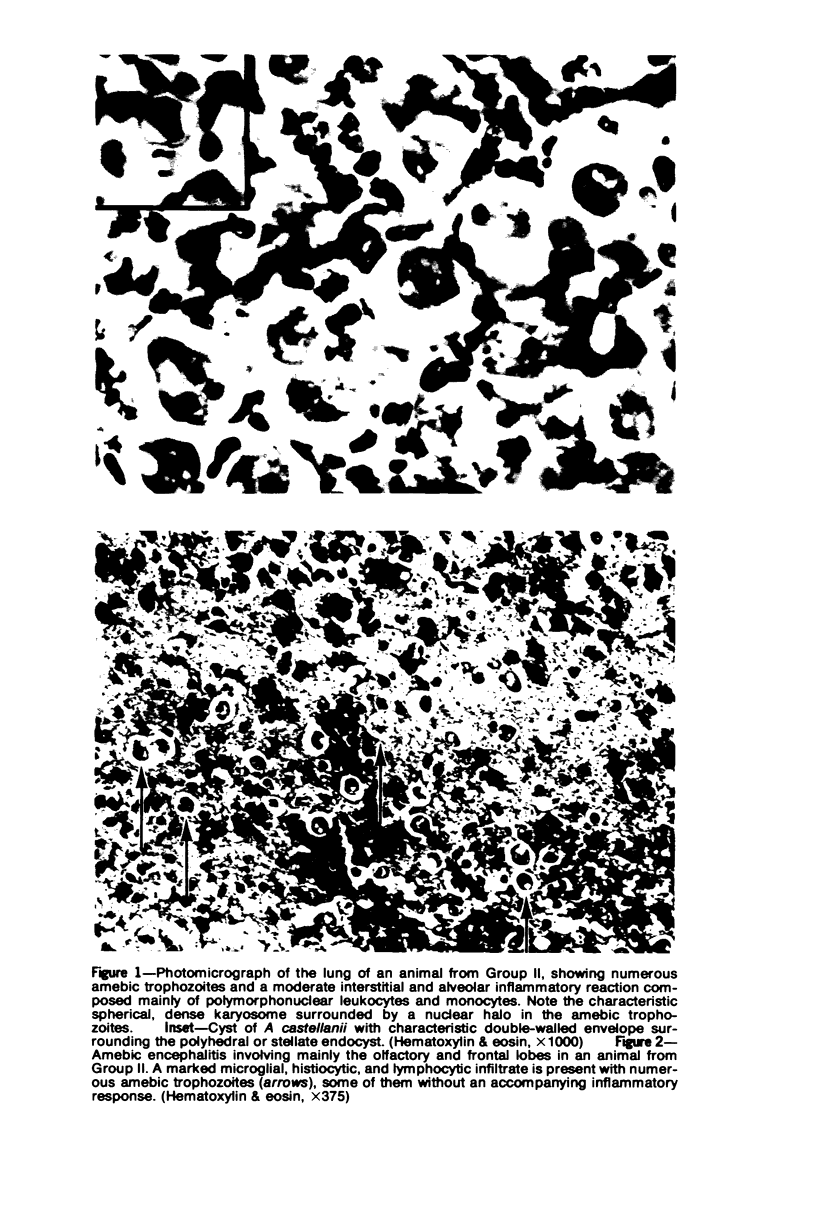
Human infections due to free-living amebas of the genus Acathamoeba have been reported sporadically, occasionally in individuals with underlying diseases. To determine if such infections may be considered opportunistic, groups of laboratory mice were pretreated with either methylprednisolone or tetracycline and inoculated intranasally with 1.075 times 10(4) Acanthamoeba castellanii isolated from a natural fresh water well. Results were compared with controls receiving either drug or amebas alone and with controls receiving saline injections with and without amebas. The mortality rate for those animals receiving methylprednisolone and amebas (50%) was found to be greater than the mortality in ameba controls (10%) (P equal 0.074). Similarly, the mortality rate for animals receiving tetracycline and amebas (60%) was higher than the mortality in the ameba controls (10%) (P equal 0.0286). Precise mechanisms for the increased mortality were unknown but were suspected to be due to the capacity of either corticosteroids or tetracycline to suppress host defenses, particularly those depending on neutrophils. The findings suggest a potentially pathogenic role for naturally occurring Acanthamoeba sp in humans with depressed host immunity.
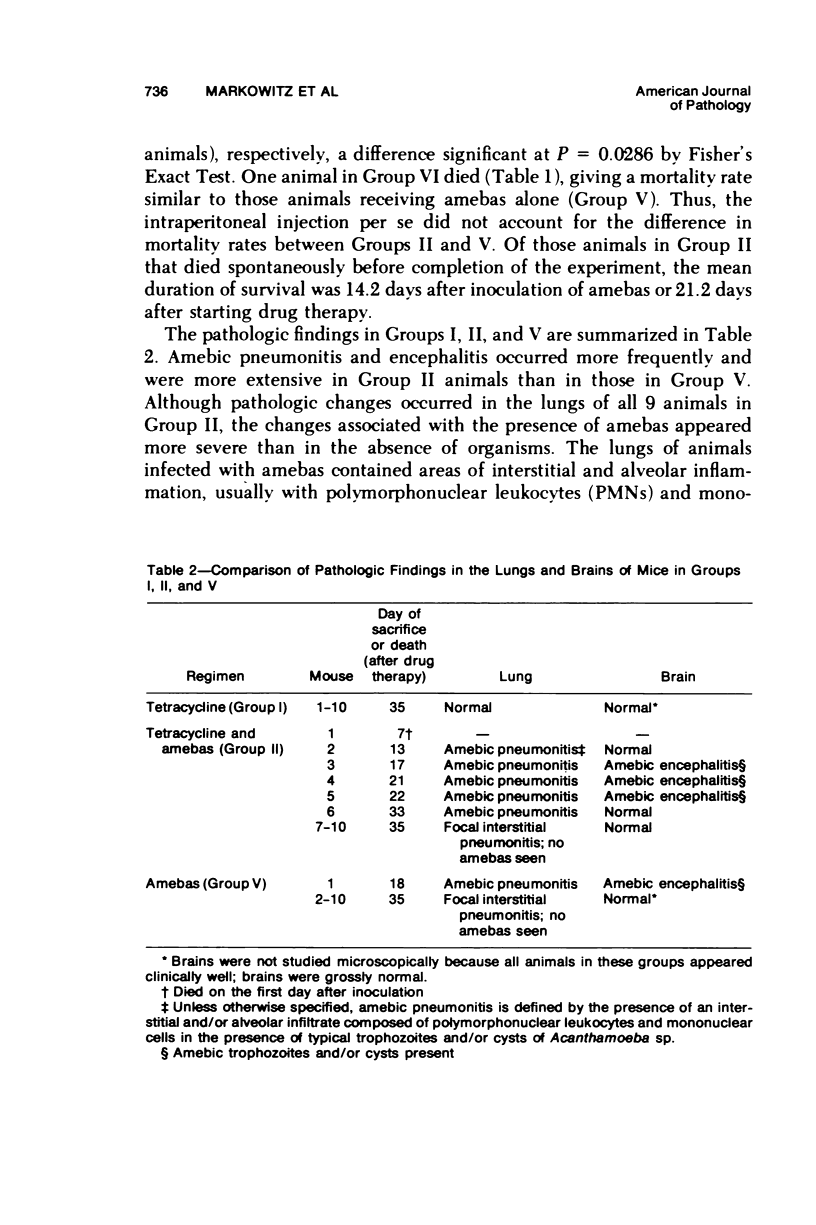
Full text
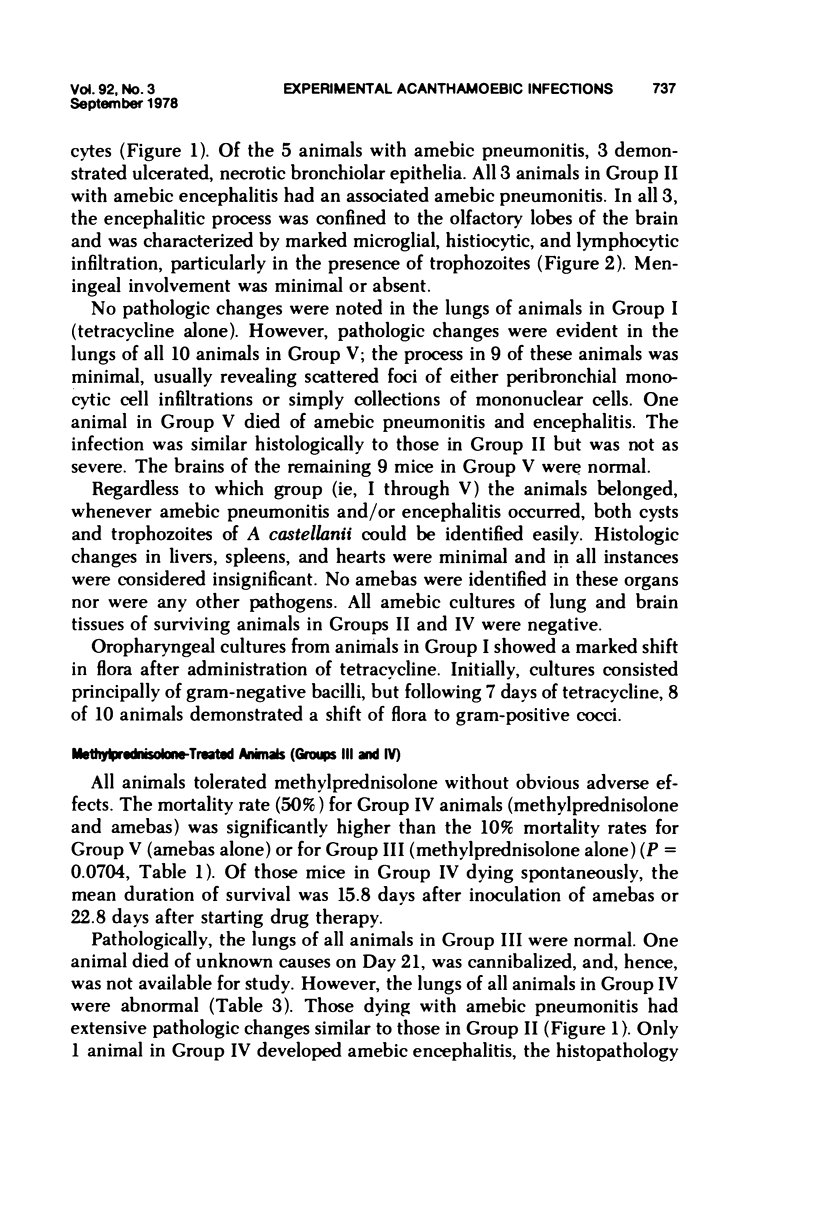
PDF


Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Ayers K. M., Billups L. H., Garner F. M. Acanthamoebiasis in a dog. Vet Pathol. 1972;9(3):221–226. doi: 10.1177/030098587200900305. [DOI] [PubMed] [Google Scholar]
- Butt C. G. Primary amebic meningoencephalitis. N Engl J Med. 1966 Jun 30;274(26):1473–1476. doi: 10.1056/NEJM196606302742605. [DOI] [PubMed] [Google Scholar]
- CULBERTSON C. G., SMITH J. W., COHEN H. K., MINNER J. R. Experimental infection of mice and monkeys by Acanthamoeba. Am J Pathol. 1959 Jan-Feb;35(1):185–197. [PMC free article] [PubMed] [Google Scholar]
- Callicott J. H., Jr, Nelson E. C., Jones M. M., dos Santos J. G., Utz J. P., Duma R. J., Morrison J. V., Jr Meningoencephalitis due to pathogenic free-living amoebae. Report of two cases. JAMA. 1968 Oct 14;206(3):579–582. [PubMed] [Google Scholar]
- Chretien J. H., Garagusi V. F. Corticosteroid effect on phagocytosis and NBT reduction by human polymorphonuclear neutrophils. J Reticuloendothel Soc. 1972 Apr;11(4):358–367. [PubMed] [Google Scholar]
- Cruz T., Reboucas G., Rocha H. Fatal strongyloidiasis in patients receiving corticosteroids. N Engl J Med. 1966 Nov 17;275(20):1093–1096. doi: 10.1056/NEJM196611172752003. [DOI] [PubMed] [Google Scholar]
- Culbertson C. G., Ensminger P. W., Overton W. M. Hartmannella (acanthamoeba). Experimental chronic, granulomatous brain infections produced by new isolates of low virulence. Am J Clin Pathol. 1966 Sep;46(3):305–314. doi: 10.1093/ajcp/46.3.305. [DOI] [PubMed] [Google Scholar]
- Dale D. C., Petersdorf R. G. Corticosteroids and infectious diseases. Med Clin North Am. 1973 Sep;57(5):1277–1287. doi: 10.1016/s0025-7125(16)32228-3. [DOI] [PubMed] [Google Scholar]
- Duma R. J., Helwig W. B., Martinez A. J. Meningoencephalitis and brain abscess due to a free-living amoeba. Ann Intern Med. 1978 Apr;88(4):468–473. doi: 10.7326/0003-4819-88-4-468. [DOI] [PubMed] [Google Scholar]
- Duma R. J. Primary amoebic meningoencephalitis. CRC Crit Rev Clin Lab Sci. 1972 Jun;3(2):163–192. doi: 10.3109/10408367209151325. [DOI] [PubMed] [Google Scholar]
- EISERT J., HANNIBAL J. E., Jr, SANDERS S. L. Fatal amebiasis complicating corticosteroid management of pemphigus vulgaris. N Engl J Med. 1959 Oct 22;261:843–845. doi: 10.1056/NEJM195910222611704. [DOI] [PubMed] [Google Scholar]
- Forsgren A., Grarpe H. Tetracyclines and host-defense mechanisms. Antimicrob Agents Chemother. 1973 Jun;3(6):711–715. doi: 10.1128/aac.3.6.711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forsgren A., Schmeling D., Quie P. G. Effect of tetracycline on the phagocytic function of human leukocytes. J Infect Dis. 1974 Oct;130(4):412–415. doi: 10.1093/infdis/130.4.412. [DOI] [PubMed] [Google Scholar]
- Fowler M., Carter R. F. Acute pyogenic meningitis probably due to Acanthamoeba sp.: a preliminary report. Br Med J. 1965 Sep 25;2(5464):740–742. doi: 10.1136/bmj.2.5464.734-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frenkel J. K., Good J. T., Shultz J. A. Latent Pneumocystis infection of rats, relapse, and chemotherapy. Lab Invest. 1966 Oct;15(10):1559–1577. [PubMed] [Google Scholar]
- Jager B. V., Stamm W. P. Brain abscesses caused by free-living amoeba probably of the genus Hartmannella in a patient with Hodgkin's disease. Lancet. 1972 Dec 23;2(7791):1343–1345. doi: 10.1016/s0140-6736(72)92781-x. [DOI] [PubMed] [Google Scholar]
- Jones D. B., Visvesvara G. S., Robinson N. M. Acanthamoeba polyphaga keratitis and Acenthamoeba uveitis associated with fatal meningoencephalitis. Trans Ophthalmol Soc U K. 1975 Jul;95(2):221–232. [PubMed] [Google Scholar]
- KASS E. H., GEIMAN Q. M., FINLAND M. Effects of ACTH on induced malaria in man. N Engl J Med. 1951 Dec 27;245(26):1000–1002. doi: 10.1056/NEJM195112272452602. [DOI] [PubMed] [Google Scholar]
- KETCHEL M. M., FAVOUR C. B., STURGIS S. H. The in vitro action of hydrocortisone on leucocyte migration. J Exp Med. 1958 Feb 1;107(2):211–218. doi: 10.1084/jem.107.2.211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kenney M. The Micro-Kolmer complement fixation test in routine screening for soil ameba infection. Health Lab Sci. 1971 Jan;8(1):5–10. [PubMed] [Google Scholar]
- Liepman M. Disseminated Strongyloides stercoralis. A complication of immunosuppression. JAMA. 1975 Jan 27;231(4):387–388. [PubMed] [Google Scholar]
- MUNOZ J., GEISTER R. Inhibition of phagocytosis by aureomycin. Proc Soc Exp Biol Med. 1950 Nov;75(2):367–370. doi: 10.3181/00379727-75-18201. [DOI] [PubMed] [Google Scholar]
- Martin R. R., Warr G. A., Couch R. B., Yeager H., Knight V. Effects of tetracycline on leukotaxis. J Infect Dis. 1974 Feb;129(2):110–116. doi: 10.1093/infdis/129.2.110. [DOI] [PubMed] [Google Scholar]
- Martinez A. J., Markowitz S. M., Duma R. J. Experimental pneumonitis and encephalitis caused by acanthamoeba in mice: pathogenesis and ultrastructural features. J Infect Dis. 1975 Jun;131(6):692–699. doi: 10.1093/infdis/131.6.692. [DOI] [PubMed] [Google Scholar]
- McConnell E. E., Garner F. M., Kirk J. H. Hartmannellosis in a bull. Pathol Vet. 1968;5(1):1–6. doi: 10.1177/030098586800500101. [DOI] [PubMed] [Google Scholar]
- Naginton J., Watson P. G., Playfair T. J., McGill J., Jones B. R., Steele A. D. Amoebic infection of the eye. Lancet. 1974 Dec 28;2(7896):1537–1540. doi: 10.1016/s0140-6736(74)90285-2. [DOI] [PubMed] [Google Scholar]
- Patras D., Andujar J. J. Meningoencephalitis due to Hartmannella (Acanthamoeba). Am J Clin Pathol. 1966 Aug;46(2):226–233. [PubMed] [Google Scholar]
- Peters W. P., Holland J. F., Senn H., Rhomberg W., Banerjee T. Corticosteroid administration and localized leukocyte mobilization in man. N Engl J Med. 1972 Feb 17;286(7):342–345. doi: 10.1056/NEJM197202172860703. [DOI] [PubMed] [Google Scholar]
- Robert V. B., Rorke L. B. Primary amebic encephalitis, probably from Acanthamoeba. Ann Intern Med. 1973 Aug;79(2):174–179. doi: 10.7326/0003-4819-79-2-174. [DOI] [PubMed] [Google Scholar]
- Wang S. S., Feldman H. A. Isolation of hartmannella species from human throats. N Engl J Med. 1967 Nov 30;277(22):1174–1179. doi: 10.1056/NEJM196711302772204. [DOI] [PubMed] [Google Scholar]
- Webel M. L., Ritts R. E., Jr, Taswell H. F., Danadio J. V., Jr, Woods J. E. Cellular immunity after intravenous administration of methylprednisolone. J Lab Clin Med. 1974 Mar;83(3):383–392. [PubMed] [Google Scholar]