Abstract
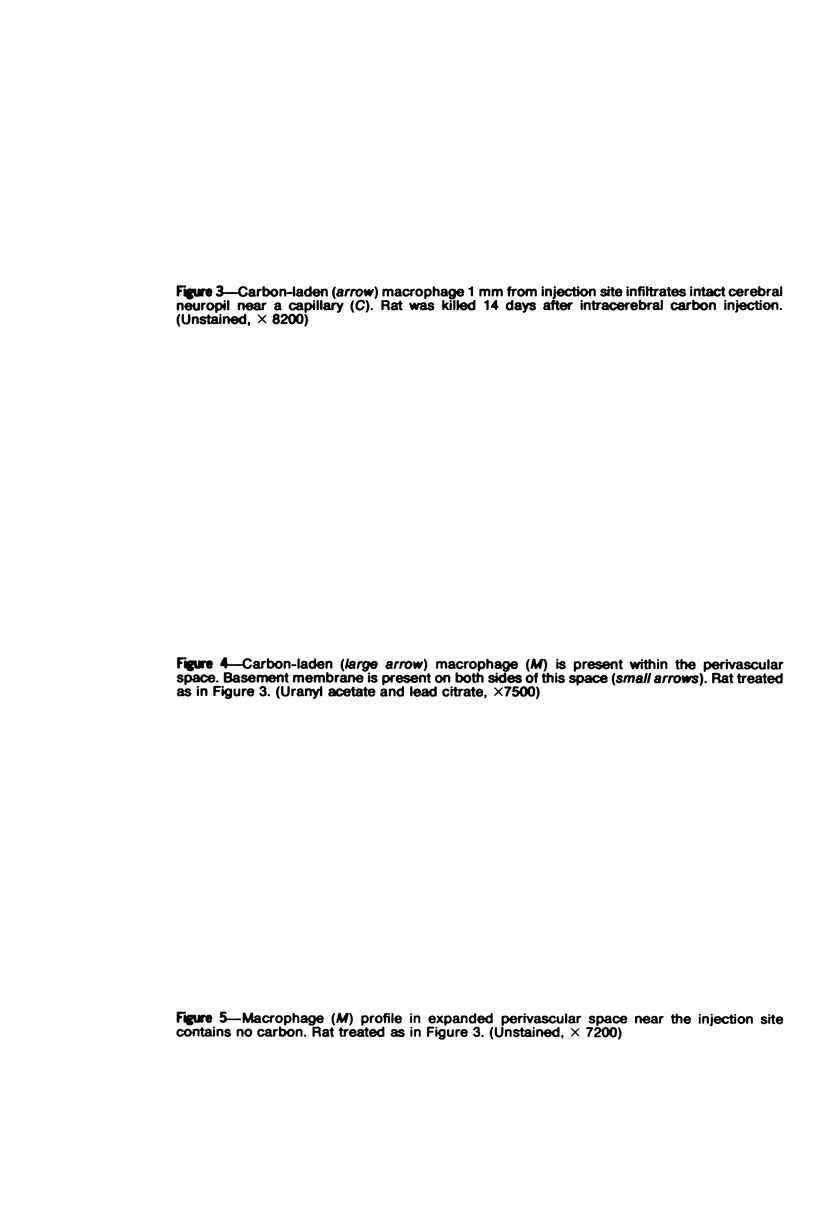
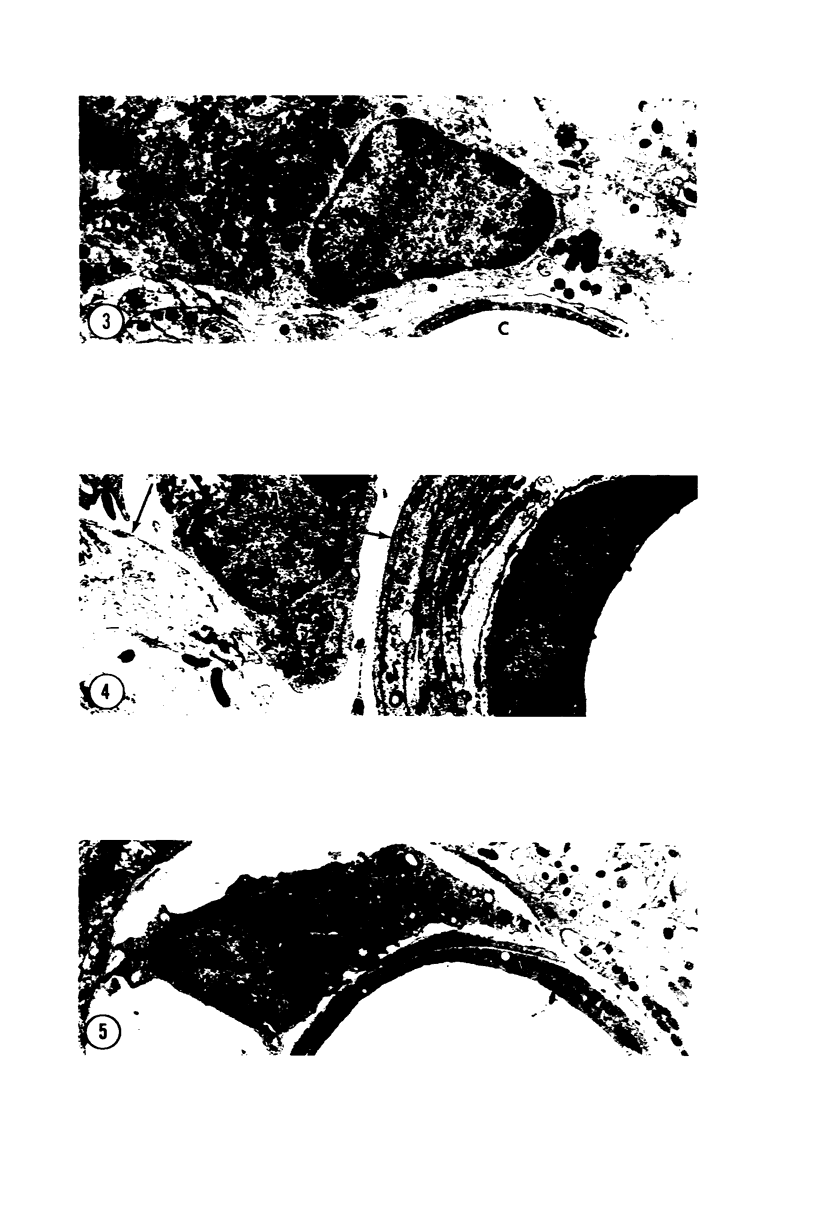
Forty-eight rats received intracerebral injections of sterile colloidal carbon. At intervals between 10 minutes and 31 days after carbon injection, the rats were perfused with glutaraldehyde, and autopsies were performed. Between 10 minutes and 3 hours after injection, carbon particles were extracellular and located strictly within the needle track. During the first few days the carbon was ingested by macrophages. Initially absent, carbon-laden macrophages spread to the neuropil immediately surrounding the injection site at 7 to 31 days following injection. These carbon-laden macrophages frequently were elongated within the neuropil and resembled microglia. Carbon-laden macrophages eventually accumulated around local vessels and in perivascular spaces. Many macrophages containing carbon remained in the injection site at the longest sampling interval of 31 days. Results indicate two macrophage responses to colloidal carbon in the central nervous system: a) an indolent population remains in the injection site for at least 1 month and b) a second population of macrophages emigrates through the neuropil. They eventually surround local vessels and enter the perivascular space. The migrating macrophages offer an explanation for the peculiar perivascular cells in Krabbe's disease and may provide a link between the CNS parenchyma and immunocompetent cells.
Full text
PDF



Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- ADRIAN E. K., Jr, WALKER B. E. Incorporation of thymidine-H3 by cells in normal and injured mouse spinal cord. J Neuropathol Exp Neurol. 1962 Oct;21:597–609. doi: 10.1097/00005072-196210000-00007. [DOI] [PubMed] [Google Scholar]
- AUSTIN J. H., LEHFELDT D. STUDIES IN GLOBOID (KRABBE) LEUKODYSTROPHY. 3. SIGNIFICANCE OF EXPERIMENTALLY-PRODUCED GLOBOID-LIKE ELEMENTS IN RAT WHITE MATTER AND SPLEEN. J Neuropathol Exp Neurol. 1965 Apr;24:265–289. [PubMed] [Google Scholar]
- Brierley J. B., Field E. J. The connexions of the spinal sub-arachnoid space with the lymphatic system. J Anat. 1948 Jul;82(Pt 3):153–166. [PMC free article] [PubMed] [Google Scholar]
- COHN Z. A., WIENER E. THE PARTICULATE HYDROLASES OF MACROPHAGES. I. COMPARATIVE ENZYMOLOGY, ISOLATION, AND PROPERTIES. J Exp Med. 1963 Dec 1;118:991–1008. doi: 10.1084/jem.118.6.991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CROME L., ZAPELLA M. SCHILDER'S DISEASE (SUDANOPHILIC LEUCODYSTROPHY) IN FIVE MALE MEMBERS OF ONE FAMILY. J Neurol Neurosurg Psychiatry. 1963 Oct;26:431–438. doi: 10.1136/jnnp.26.5.431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cardella C. J., Davies P., Allison A. C. Immune complexes induce selective release of lysosomal hydrolases from macrophages. Nature. 1974 Jan 4;247(5435):46–48. doi: 10.1038/247046a0. [DOI] [PubMed] [Google Scholar]
- Casley-Smith J. R., Földi-Börsök E., Földi M. The prelymphatic pathways of the brain as revealed by cervical lymphatic obstruction and the passage of particles. Br J Exp Pathol. 1976 Apr;57(2):179–188. [PMC free article] [PubMed] [Google Scholar]
- Cohen S., Vassalli P., Benacerraf B., McCluskey R. T. The distribution of antigenic and nonantigenic compounds within draining lymph nodes. Lab Invest. 1966 Jul;15(7):1143–1155. [PubMed] [Google Scholar]
- Davies P., Page R. C., Allison A. C. Changes in cellular enzyme levels and extracellular release of lysosomal acid hydrolases in macrophages exposed to group A streptococcal cell wall substance. J Exp Med. 1974 May 1;139(5):1262–1282. doi: 10.1084/jem.139.5.1262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fujita S., Kitamura T. Origin of brain macrophages and the nature of the so-called microglia. Acta Neuropathol Suppl. 1975;Suppl 6:291–296. doi: 10.1007/978-3-662-08456-4_51. [DOI] [PubMed] [Google Scholar]
- HEPPLESTON A. G. The disposal of inhaled particulate matter; a unifying hypothesis. Am J Pathol. 1963 Feb;42:119–135. [PMC free article] [PubMed] [Google Scholar]
- Hirth R. S., Nielsen S. W. A familial canine globoid cell leukodystrophy ("Krabbe Type"). J Small Anim Pract. 1967 Oct;8(10):569–575. doi: 10.1111/j.1748-5827.1967.tb04499.x. [DOI] [PubMed] [Google Scholar]
- Huntington H. W., Terry R. D. The origin of the reactive cells in cerebral stab wounds. J Neuropathol Exp Neurol. 1966 Oct;25(4):646–653. doi: 10.1097/00005072-196610000-00010. [DOI] [PubMed] [Google Scholar]
- Imamoto K., Leblond C. P. Presence of labeled monocytes, macrophages and microglia in a stab wound of the brain following an injection of bone marrow cells labeled with 3H-uridine into rats. J Comp Neurol. 1977 Jul 15;174(2):255–279. doi: 10.1002/cne.901740205. [DOI] [PubMed] [Google Scholar]
- KONIGSMARK B. W., SIDMAN R. L. ORIGIN OF BRAIN MACROPHAGES IN THE MOUSE. J Neuropathol Exp Neurol. 1963 Oct;22:643–676. doi: 10.1097/00005072-196310000-00006. [DOI] [PubMed] [Google Scholar]
- Kerns J. M., Hinsman E. J. Neuroglial response to sciatic neurectomy. I. Light microscopy and autoradiography. J Comp Neurol. 1973 Oct 1;151(3):237–254. doi: 10.1002/cne.901510303. [DOI] [PubMed] [Google Scholar]
- Kitamura T., Hattori H., Fujita S. Autoradiographic studies on histogenesis of brain macrophages in the mouse. J Neuropathol Exp Neurol. 1972 Jul;31(3):502–518. doi: 10.1097/00005072-197207000-00008. [DOI] [PubMed] [Google Scholar]
- LABELLE C. W., BRIEGER H. The fate of inhaled particles in the early postexposure period. II. The role of pulmonary phagocytosis. Arch Environ Health. 1960 Nov;1:423–427. doi: 10.1080/00039896.1960.10662717. [DOI] [PubMed] [Google Scholar]
- Liu H. M. Ultrastructure of globoid leukodystrophy (Krabbe's disease) with reference to the origin of globoid cells. J Neuropathol Exp Neurol. 1970 Jul;29(3):441–462. doi: 10.1097/00005072-197007000-00008. [DOI] [PubMed] [Google Scholar]
- MILLER J. J., 3rd, NOSSAL G. J. ANTIGENS IN IMMUNITY. VI. THE PHAGOCYTIC RETICULUM OF LYMPH NODE FOLLICLES. J Exp Med. 1964 Dec 1;120:1075–1086. doi: 10.1084/jem.120.6.1075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKeever P., Balentine J. D. An ultrastructural study of acid phosphatase activity of rat ventral motor horn cells with observations on the effects of hyperbaric oxygen. Lab Invest. 1973 Dec;29(6):633–641. [PubMed] [Google Scholar]
- NELSON E., AUREBECK G., OSTERBERG K., BERRY J., JABBOUR J. T., BORNHOFEN J. ULTRASTRUCTURAL AND CHEMICAL STUDIES ON KRABBE'S DISEASE. J Neuropathol Exp Neurol. 1963 Jul;22:414–434. doi: 10.1097/00005072-196307000-00004. [DOI] [PubMed] [Google Scholar]
- NELSON E., OSTERBERG K., BLAW M., STORY J., KOZAK P. Electron microscopic and histochemical studies in diffuse sclerosis (sudanophilic type). Neurology. 1962 Dec;12:896–909. doi: 10.1212/wnl.12.12.896. [DOI] [PubMed] [Google Scholar]
- NORMAN R. M., URICH H., FRANCE N. E. Perivascular cavitation of the basal ganglia in gargoylism. J Ment Sci. 1959 Oct;105:1070–1077. doi: 10.1192/bjp.105.441.1070. [DOI] [PubMed] [Google Scholar]
- Nossal G. J., Abbot A., Mitchell J. Antigens in immunity. XIV. Electron microscopic radioautographic studies of antigen capture in the lymph node medulla. J Exp Med. 1968 Feb 1;127(2):263–276. doi: 10.1084/jem.127.2.263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nossal G. J., Abbot A., Mitchell J., Lummus Z. Antigens in immunity. XV. Ultrastructural features of antigen capture in primary and secondary lymphoid follicles. J Exp Med. 1968 Feb 1;127(2):277–290. doi: 10.1084/jem.127.2.277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roessmann U., Friede R. L. Entry of labeled monocytic cells into the central nervous system. Acta Neuropathol. 1968 Jun 7;10(4):359–362. doi: 10.1007/BF00690711. [DOI] [PubMed] [Google Scholar]
- Rosenthal A. S., Shevach E. M. The function of macrophages in T-lymphocyte antigen recognition. Contemp Top Immunobiol. 1976;5:47–90. [PubMed] [Google Scholar]
- Roser B. The origins, kinetics, and fate of macrophage populations. J Reticuloendothel Soc. 1970 Aug;8(2):139–161. [PubMed] [Google Scholar]
- Schochet S. S., Jr, Hardman J. M., Lampert P. W., Earle K. M. Krabbe's disease (globoid leukodystrophy). Electron microscopic observations. Arch Pathol. 1969 Sep;88(3):305–313. [PubMed] [Google Scholar]
- Stenwig A. E. The origin of brain macrophages in traumatic lesions, Wallerian degeneration, and retrograde degeneration. J Neuropathol Exp Neurol. 1972 Oct;31(4):696–704. doi: 10.1097/00005072-197210000-00011. [DOI] [PubMed] [Google Scholar]
- Tanaka R., Iwasaki Y., Koprowski H. Ultrastructural studies of perivascular cuffing cells in multiple sclerosis brain. Am J Pathol. 1975 Dec;81(3):467–478. [PMC free article] [PubMed] [Google Scholar]
- Thomas D. W., Yamashita U., Shevach E. M. Nature of the antigenic complex recognized by T lymphocytes. IV. Inhibition of antigen-specific T cell proliferation by antibodies to stimulator macrophage Ia antigens. J Immunol. 1977 Jul;119(1):223–226. [PubMed] [Google Scholar]
- Torvik A. The relationship between microglia and brain macrophages. Experimental investigations. Acta Neuropathol Suppl. 1975;Suppl 6:297–300. doi: 10.1007/978-3-662-08456-4_52. [DOI] [PubMed] [Google Scholar]
- VOGEL F. S. Demyelinization induced in living rabbits by means of a lipolytic enzyme preparation. J Exp Med. 1951 Apr 1;93(4):297–304. doi: 10.1084/jem.93.4.297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Furth R., Cohn Z. A. The origin and kinetics of mononuclear phagocytes. J Exp Med. 1968 Sep 1;128(3):415–435. doi: 10.1084/jem.128.3.415. [DOI] [PMC free article] [PubMed] [Google Scholar]