Abstract
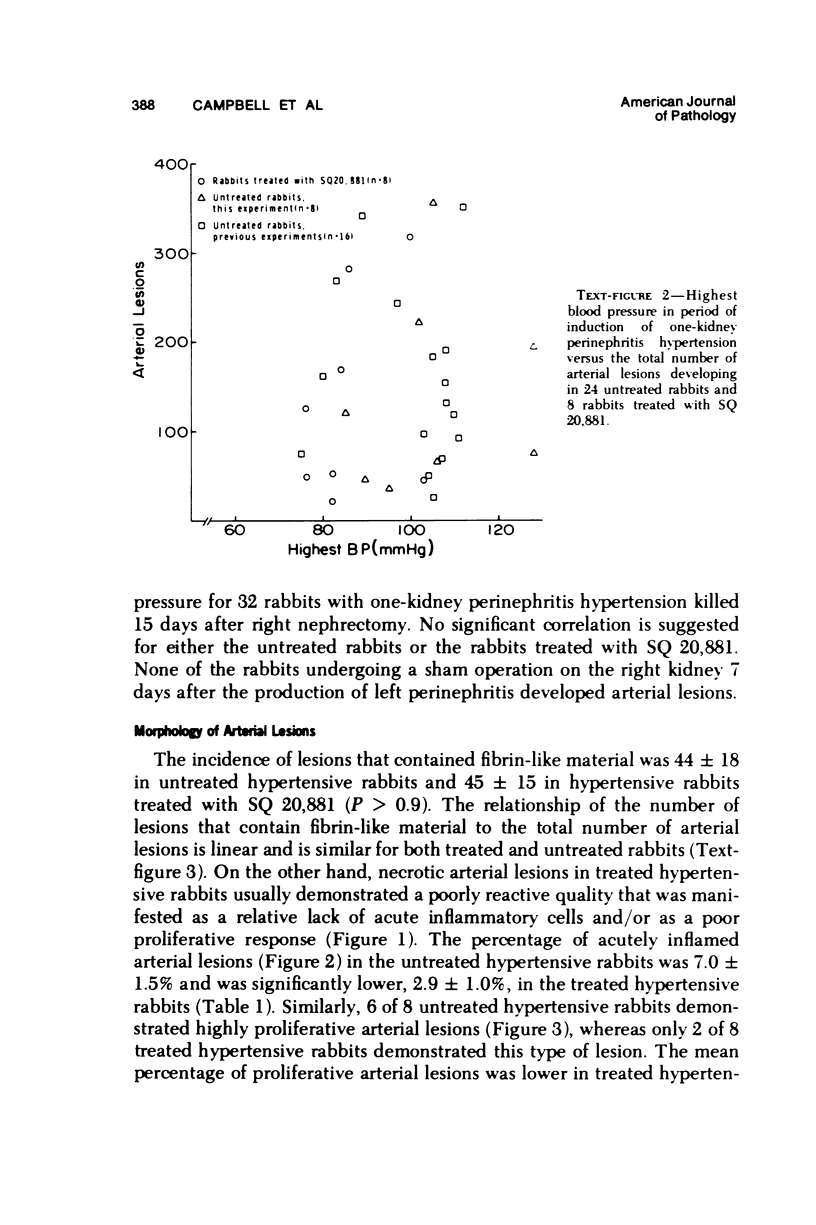
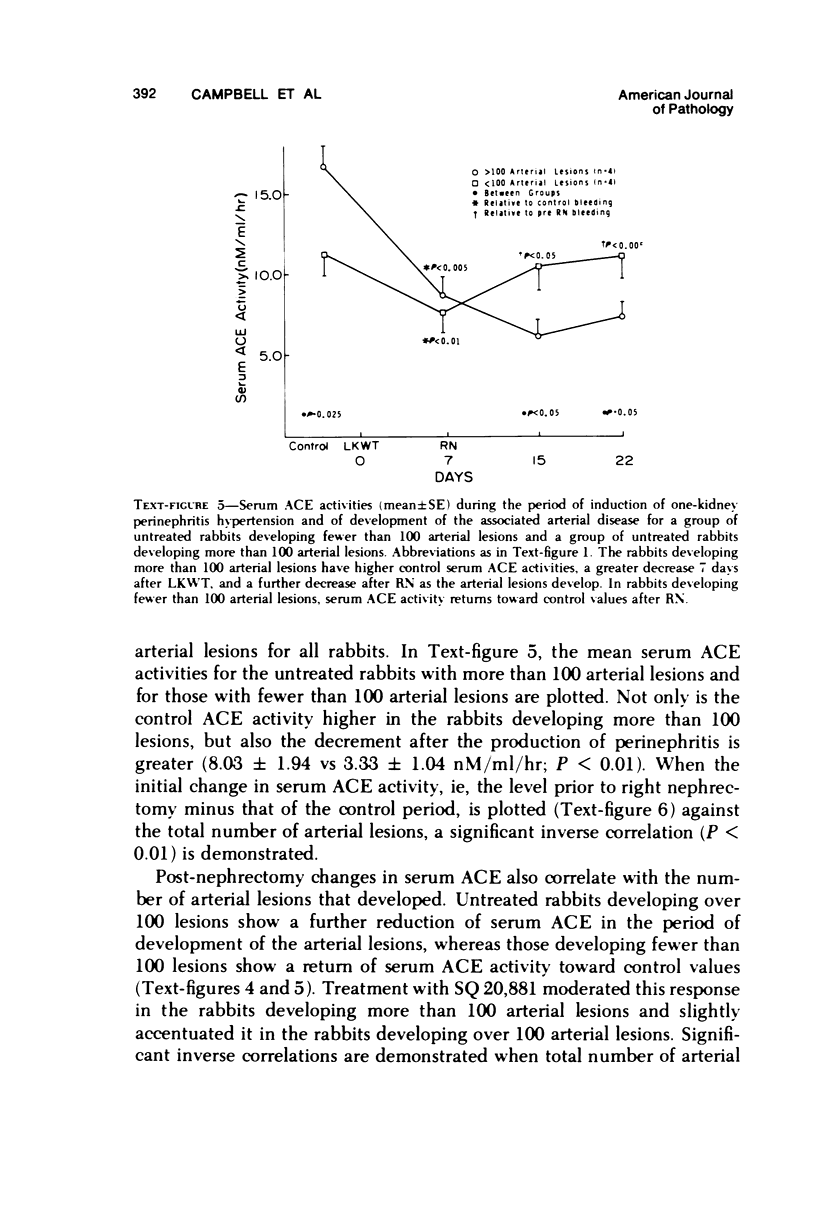
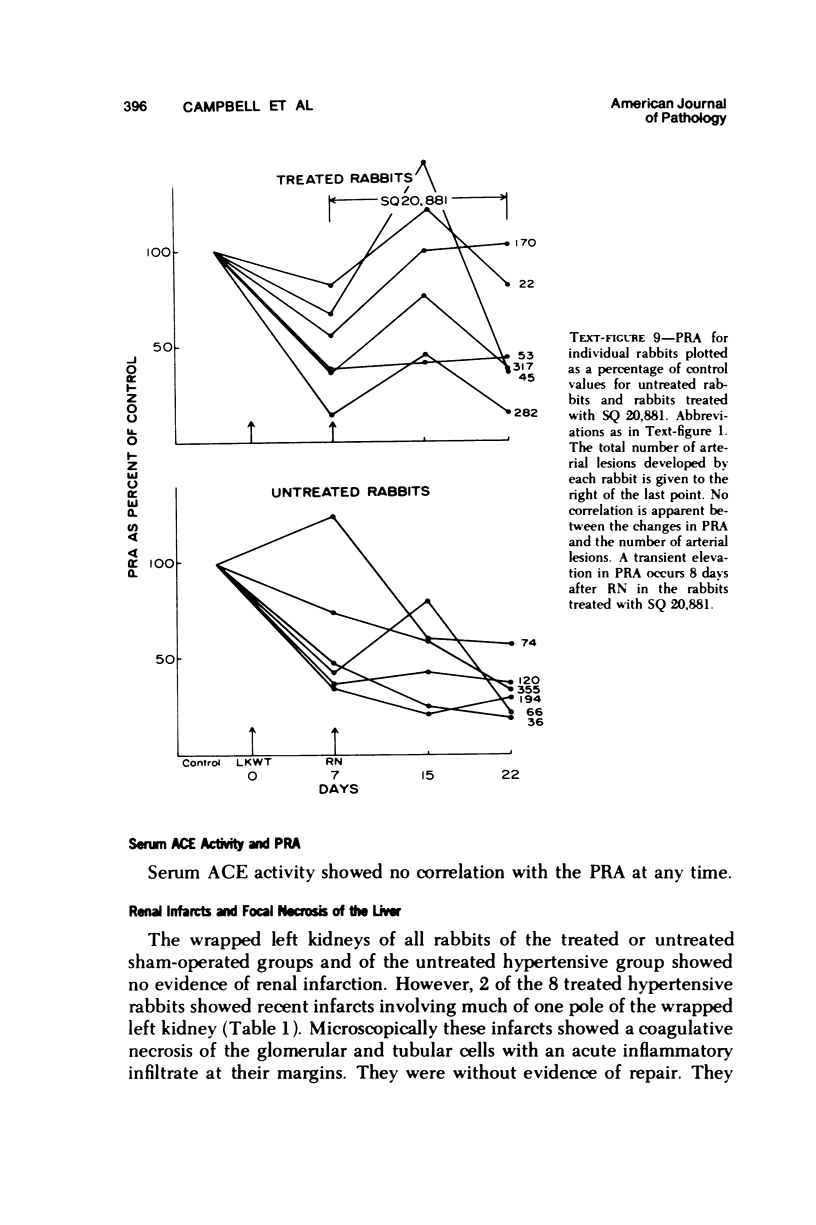
Serum angiotensin converting enzyme (ACE) activity and plasma renin activity (PRA) were studied during the development of the widespread necrotic arterial disease that occurs in the induction phase of one-kidney perinephritis hypertension. Control serum ACE activity was significantly higher in rabbits developing many arterial lesions than it was in rabbits developing relatively few arterial lesions. Serum ACE decreased 7 days after the production of unilateral perinephritis in all rabbits. Following contralateral nephrectomy, serum ACE decreased further in rabbits devloping many arterial lesions but returned toward control values in rabbits developing relatively few arterial lesions. Significant inverse correlations were demonstrated for the total number of arterial lesions that developed relative to a) the decrease in serum ACE activity 7 days after the production of unilateral perinephritis, b) the lowest or the average serum ACE activity during the period of development of the arterial lesions after contralateral nephrectomy, and c) the change in serum ACE activity during the period of development of the arterial lesions. Chronic treatment with SQ 20,881, a synthetic nonapeptide inhibitor of ACE activity, during the period of development of the hypertension and the arterial lesions significantly reduced the serum ACE activity and the hypertension but did not change interrelationships between serum ACE activity and the number of arterial lesions that developed. PRA significantly decreased after the production of perinephritis and decreased somewhat further during the induction period of the hypertension after contralateral nephrectomy. No relationships were demonstrated between PRA, or changes in PRA, and the development of arterial lesions. The increase in blood pressure during the incubation period of the hypertension did not correlate with the number of arterial lesions that developed. These finding indicate that serum ACE activity reflects importantly on the capacity to develop necrotic arterial lesions during the induction phase of one-kidney perinephritis hypertention and on functional events relating to their pathogenesis.
Full text
PDF
















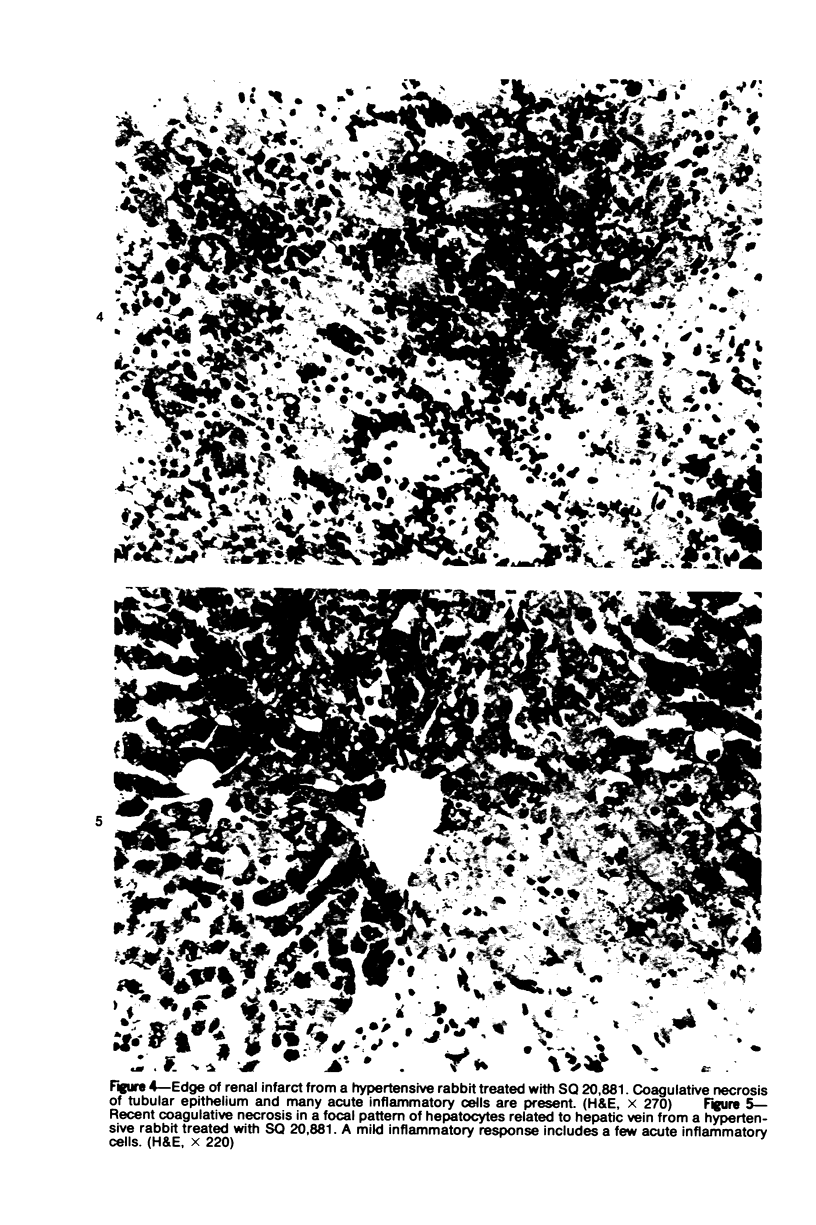
Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- CAMPBELL W. G., Jr, SANTOS BUCH C. A. WIDELY DISTRIBUTED NECROTIZING ARTERITIS INDUCED IN RABBITS BY EXPERIMENTAL RENAL ALTERATIONS. IV. DEMONSTRATION OF DECREASED AMOUNT OF THROMBIN CLOTTABLE PLASMA PROTEIN DURING DEVELOPMENT OF THE ARTERIAL LESIONS. Am J Pathol. 1965 Jan;46:71–83. [PMC free article] [PubMed] [Google Scholar]
- CAMPBELL W. G., Jr, SANTOS-BUCH C. A. WIDELY DISTRIBUTED NECROTIZING ARTERITIS INDUCED IN RABBITS BY EXPERIMENTAL RENAL ALTERATIONS. III. STUDIES ON ACTIVITY AND DECAY OF NECROTIZING FACTORS. Am J Pathol. 1963 Aug;43:131–141. [PMC free article] [PubMed] [Google Scholar]
- CAMPBELL W. G., Jr, SANTOS-BUCH C. A. Widely distributed necrotizing arteritis induced in rabbits by experimental renal alterations. I. Comparison with the vascular lesions induced by injections of foreign serum. Am J Pathol. 1959 May-Jun;35(3):439–465. [PMC free article] [PubMed] [Google Scholar]
- CAMPBELL W. G., Jr, SANTOS-BUCH C. A. Widely distributed necrotizing arteritis induced in rabbits by experimental renal alterations. II. Relationship of the arterial lesions to perirenal inflammation. Am J Pathol. 1959 Jul-Aug;35(4):769–789. [PMC free article] [PubMed] [Google Scholar]
- Campbell D. J., Skinner S. L., Day A. J. Cellophane perinephritis hypertension and its reversal in rabbits. Effect on plasma renin, renin substrate, and renal mass. Circ Res. 1973 Jul;33(1):105–112. doi: 10.1161/01.res.33.1.105. [DOI] [PubMed] [Google Scholar]
- Campbell W. G., Jr, Santos-Buch C. A. Widely distributed necrotic arterial lesions induced in rabbits by experimental renal alterations. V. Light microscopic studies of early lesions of arterial, cardiac, and skeletal muscle. Lab Invest. 1966 Dec;15(12):1856–1869. [PubMed] [Google Scholar]
- Cushman D. W., Cheung H. S. Spectrophotometric assay and properties of the angiotensin-converting enzyme of rabbit lung. Biochem Pharmacol. 1971 Jul;20(7):1637–1648. doi: 10.1016/0006-2952(71)90292-9. [DOI] [PubMed] [Google Scholar]
- Eide I., Aars H. Renal hypertension in rabbits immunized with angiotensin. II. Scand J Clin Lab Invest. 1970 Mar;25(2):119–127. doi: 10.3109/00365517009049193. [DOI] [PubMed] [Google Scholar]
- Eide I., Aars H. Renal hypertension in rabbits immunized with angiotensin. Nature. 1969 May 10;222(5193):571–571. doi: 10.1038/222571a0. [DOI] [PubMed] [Google Scholar]
- Engel S. L., Schaeffer T. R., Gold B. I., Rubin B. Inhibition of pressor effects of angiotensin I and augmentation of depressor effects of bradykinin by synthetic peptides. Proc Soc Exp Biol Med. 1972 May;140(1):240–244. doi: 10.3181/00379727-140-36433. [DOI] [PubMed] [Google Scholar]
- Erdös E. G. The angiotensin I converting enzyme. Fed Proc. 1977 Apr;36(5):1760–1765. [PubMed] [Google Scholar]
- Gavras H., Brunner H. R., Laragh J. H., Vaughan E. D., Jr, Koss M., Cote L. J., Gavras I. Malignant hypertension resulting from deoxycorticosterone acetate and salt excess: role of renin and sodium in vascular changes. Circ Res. 1975 Feb;36(2):300–309. doi: 10.1161/01.res.36.2.300. [DOI] [PubMed] [Google Scholar]
- Giese J. Renin, angiotensin and hypertensive vascular damage: a review. Am J Med. 1973 Sep;55(3):315–332. doi: 10.1016/0002-9343(73)90133-2. [DOI] [PubMed] [Google Scholar]
- Haber E., Koerner T., Page L. B., Kliman B., Purnode A. Application of a radioimmunoassay for angiotensin I to the physiologic measurements of plasma renin activity in normal human subjects. J Clin Endocrinol Metab. 1969 Oct;29(10):1349–1355. doi: 10.1210/jcem-29-10-1349. [DOI] [PubMed] [Google Scholar]
- Ichikawa S., Johnson J. A., Stanton M. W., Payne C. G., Keitzer W. F. Hemodynamic effects of an angiotensin II antagonist in rabbits with perinephritis hypertension. Proc Soc Exp Biol Med. 1977 Jun;155(2):259–263. doi: 10.3181/00379727-155-39785. [DOI] [PubMed] [Google Scholar]
- Lendrum A. C. Deposition of plasmatic substances in vessel walls. Pathol Microbiol (Basel) 1967;30(5):681–684. doi: 10.1159/000161709. [DOI] [PubMed] [Google Scholar]
- Oparil S., Haber E. The renin-angiotensin system (second of two parts). N Engl J Med. 1974 Aug 29;291(9):446–457. doi: 10.1056/NEJM197408292910905. [DOI] [PubMed] [Google Scholar]
- Romero J. C., Hoobler S. W., Kozak T. J., Warzynski R. J. Effect of antirenin on blood pressure of rabbits with experimental renal hypertension. Am J Physiol. 1973 Oct;225(4):810–817. doi: 10.1152/ajplegacy.1973.225.4.810. [DOI] [PubMed] [Google Scholar]
- Romero J. C., Ott C. E., Aguilo J. J., Torres V. E., Strong C. G. Role of prostaglandins in the reversal of one-kidney hypertension in the rabbit. Circ Res. 1975 Nov;37(5):683–689. doi: 10.1161/01.res.37.5.683. [DOI] [PubMed] [Google Scholar]
- Romero J. C., Strong C. G. The effect of indomethacin blockade of prostaglandin synthesis on blood pressure of normal rabbits and rabbits with renovascular hypertension. Circ Res. 1977 Jan;40(1):35–41. doi: 10.1161/01.res.40.1.35. [DOI] [PubMed] [Google Scholar]
- Santos-Buch C. A., Goodhue W. W., Ewald B. H. Concurrence of iris aneurysms and cerebral hemorrhage in hypertensive rabbits. Arch Neurol. 1976 Feb;33(2):96–103. doi: 10.1001/archneur.1976.00500020024005. [DOI] [PubMed] [Google Scholar]
- Santos-Buch C. A., Murphy G. E., Becker C. G., Miscall B. G., Campbell W. G., Jr Evidence of a causative role of adrenocortical activity in the genesis of disseminated arterial lesions induced in rabbits by renal alterations. Lab Invest. 1966 Aug;15(8):1327–1341. [PubMed] [Google Scholar]
- Soffer R. L. Angiotensin-converting enzyme and the regulation of vasoactive peptides. Annu Rev Biochem. 1976;45:73–94. doi: 10.1146/annurev.bi.45.070176.000445. [DOI] [PubMed] [Google Scholar]