Abstract
Tolerogenic dendritic cells (DCs) may be valuable in transplantation for silencing immune reaction. Macrophage colony-stimulating factor (M-CSF)/IL-4 induces differentiation of cord blood (CB) monocytes into DCs (M-DCs) with tolerogenic phenotype/function. We assessed whether factors produced by tolerogenic DCs could modulate hematopoiesis. TGF-β1 added to CB M-DC cultures induced bona fide DC morphology (TGF-M-DCs), similar to that of DCs generated with TGF-β and granulocyte-macrophage colony-stimulating factor (GM-CSF)/IL-4 (TGF-GM-DCs). Of conditioned media (CM) produced from TGF-M-DCs, TGF-GM-DCs, M-DCs, and GM-DCs, TGF-M-DC CM was the only one that enhanced SCF, Flt3 ligand, and TPO expansion of myeloid progenitor cells ex vivo. This effect was blocked by neutralizing anti–M-CSF Ab, but protein analysis of CM suggested that M-CSF alone was not manifesting enhanced expansion of myeloid progenitors. LPS-stimulated TGF-M-DCs induced T-cell tolerance/anergy as effectively as M-DCs. TGF-M-DCs secreted significantly lower concentrations of progenitor cell inhibitory cytokines and were less potent in activating T cells than TGF-GM-DCs. Functional differences between TGF-M-DCs and TGF-GM-DCs included enhanced responses to LPS-induced ERK, JNK, and P38 activation in TGF-M-DCs and their immune suppressive–skewed cytokine release profiles. TGF-M-DCs appear unique among culture-generated DCs in their capability for silencing immunity while promoting expansion of myeloid progenitors, events that may be of therapeutic value.
Introduction
Dendritic cells (DCs) are the most potent antigen-presenting cells and play a pivotal role in modulating immune responses.1 DCs have the potential to induce immune rejection or tolerance and thus play a critical role in transplantation.2,3 Plasmacytoid precursor DCs facilitate hematopoietic stem cell (HSC) engraftment in an allogeneic setting without causing graft-versus-host diseases (GVHD).4 Generation of regulatory DCs by treatment of DCs with IL-10 induces tolerance across MHC barriers in both human xenogeneic GVHD and murine GVHD models.5 These results suggest the possibility for potential therapeutic uses of modified DCs to achieve transplantation tolerance
Little is known about potential roles for DCs in proliferation, survival, and differentiation of hematopoietic stem/progenitor cells. Murine bone marrow–derived DCs support colony formation of bone marrow colony-forming units–granulocyte macrophage (CFU-GMs) and colony-forming units–megakaryocytes (CFU-Ms) in vitro.6 Whether human DCs, especially tolerogenic DCs, support hematopoiesis has not been reported. A population of DCs that induces tolerance as well as enhancing hematopoietic recovery may be of therapeutic use. In transplantation settings, host conditioning and GVHD lead to systemic and local inflammation that could possibly induce maturation of DCs. Maturation signals such as bacterial lipopolysaccharide (LPS) induce DCs to up-regulate messenger RNA for cytokines and chemokines,7 which might modulate systematic immune reactions and hematopoietic recovery after transplantation.7
We reported that macrophage colony-stimulating factor (M-CSF) and IL-4 induce differentiation of cord blood (CB) monocytes into a population of IL-10highIL-12absent DCs (M-DCs) with tolerogenic potential.8 This is different from standard methods that use granulocyte-macrophage colony-stimulating factor (GM-CSF) and IL-4 to generate DCs (GM-DCs). TGF-β1 modulates DC differentiation and function,9–11 but whether TGF-β1 modulates M-DC immune function and plays a potential supporting role for these cells in hematopoiesis was not known. Maturation of DCs is associated with activation of at least 3 members of the mitogen-activated protein kinase (MAPK) family, including extracellular signal–regulated kinase (ERK), c-Jun N-terminal kinase (JNK), and p38 kinase.12–14 MAPK activation associated with maturation plays an important role in regulation of phenotype, cytokine production, and T-cell regulatory function of human DCs.12–14 In the present study, we evaluated effects of TGF-β1 in modulating M-DC immune function, enhancing cytokine-induced ex vivo expansion of myeloid progenitor cells, and a role for MAPK in these effects.
Materials and methods
Isolation of monocytes, CD34+ cells, and CD4+ T cells from CB
Heparinized umbilical CB was collected according to institutional guidelines. Approval was obtained from the committee of the Indiana University School of Medicine's institutional review board for these studies. Adult blood (AB) buffy coat was obtained from the Indiana Blood Center (Indianapolis, IN). CB and AB mononuclear cells were isolated by density gradient centrifugation on Ficoll Paque plus (1.077 g/mL; Amersham Pharmacia Biotech). Monocytes, CD34+ progenitor cells, and CD4+ T cells were purified from CB using magnetic-activated cell sorting (MACS) CD14+ magnetic beads, CD34 progenitor isolation kit, and CD4+ T cell isolation kit, respectively (Miltenyi Biotec, Auburn, CA). CD14+ monocytes were also purified from AB buffy coat. Enriched CD4+ T cells (> 95% pure as analyzed by flow cytometry) from different CB samples were frozen until use.
Cell culture
CB or AB CD14+ monocytes (5 × 105 cells/mL) were cultured in RPMI 1640 medium (BioWhittaker, Walkersville, MD) as described previously8 with different combinations of the following amounts of purified recombinant human cytokines: 10 ng/mL interleukin-4 (IL-4), 100 ng/mL macrophage colony-stimulating factor (M-CSF), 10 ng/mL transforming growth factor-beta 1 (TGF-β1) (Peprotech, Rocky Hill, NJ), and 10 ng/mL granulocyte-macrophage colony-stimulating factor (GM-CSF) (Immunex/Amgen, Seattle, WA). To induce maturation of M-DCs (produced with M-CSF, IL-4 ± TGF-β) and DCs (produced with GM-CSF, IL-4 ± TGF-β), 1 μg/mL bacterial lipopolysaccharide (LPS) from Salmonella minnesota (Sigma-Aldrich, St Louis, MO) was added to cultures on day 5, and cells were incubated for an additional 24 hours before cells were washed.
Surface and intracellular immunostaining
Harvested cells were washed twice with PBS supplemented with 1% BSA. Fc receptors on cells were preblocked with excess human IgG (Sigma-Aldrich) on ice for 15 minutes. Cells were stained for 30 minutes at 4°C with the following FITC-conjugated Abs: anti–HLR-DR, anti-CD80, anti-CD86, and anti-CD83 or isotype controls (eBioscience, San Diego, CA), and PE-conjugated Abs: CD1a (eBioscience) and CD207 (Langerin; BD Bioscience, San Jose, CA). For intracellular staining of Foxp3 expression on T cells, T cells were first stained with anti–CD4-FITC and anti–CD25-PE. Then, T cells were fixed and permeabilized before staining with anti–Foxp3-APC (BD Bioscience). Cells were analyzed by flow cytometry.
Production of conditioned medium (CM)
Cultured M-DCs and GM-DCs were harvested on day 5 and washed 3 times to remove residual cytokines. Cells (5 × 105/mL) were stimulated with 1 μg/mL LPS for 24 hours in RPMI 1640 culture medium. Supernatant was collected and frozen at − 80°C. Control CM prepared with 1 μg/mL LPS without cells was used as a control for the effects of LPS itself. Control medium is RPMI 1640 culture medium.
Ex vivo expansion
For colony assessment of precultured freshly isolated CB, CD34+ cells were plated in triplicate as described15,16 in 0.9% methylcellulose culture medium with 30% FBS and a combination of recombinant human GM-CSF (10 ng/mL), interleukin-3 (IL-3, 10 ng/mL), stem cell factor (SCF, 50 ng/mL), and erythropoietin (Epo, 1 U/mL). Different CD34+ cell concentrations were plated in order to find the concentration of cells that resulted in enough colonies to score accurately and without colony overlap. For ex vivo expansion, CB CD34+ cells (1 × 104/mL) were cultured in IMDM medium (supplemented with 5% heat-inactivated FBS, 2 mM l-glutamine, 25 μM Hepes, 50 μM β-mercaptoethanol, 100 U/mL penicillin, and 100 μg/mL streptomycin) and 25% to 50% vol/vol CM in the presence or absence of a combination of previously determined optimal progenitor cell expanding growth factors (50 ng/mL SCF, 100 ng/mL Flt-3 ligand [FL], and 100 ng/mL thrombopoietin [TPO]: SFT). In some experiments, neutralizing goat anti–M-CSF or goat control Ab (20 μg/mL) (R&D Systems, Minneapolis, MN) was added into cultures containing CM and SFT. Cells were cultured for 1 week, harvested, and counted to determine absolute cell numbers after expansion, stained with CD34-PE to determine percentage of CD34+ cells, and plated at various concentrations in 0.9% methylcellulose culture medium as described earlier in this paragraph to determine generation of myeloid progenitor cells. Cells were plated in this paragraph in low (5%) oxygen for ex vivo expansion and for colony assessment. Colonies were scored after 12 to 14 days in methylcellulose culture. Absolute numbers of myeloid progenitor cells were calculated after 1-week culture.
Assay for cytokine protein levels
Cells were washed extensively and 2.5 × 105 cells/mL were stimulated with LPS (1 μg/mL) in culture medium in 24-well plates for 24 hours. Washed cells were also incubated with ERK inhibitor U0126 for 30 minutes before addition of LPS. Conditioned media were sent to Whatman (Sanford, ME) for analysis of multiple cytokines using microspot enzyme-linked immunosorbent assay (ELISA) technology. Each sample was analyzed in triplicate.
Primary and secondary mixed leukocyte reaction (MLR)
The assay was done as described previously8 with modifications. In brief, primary MLR was established with 5 × 104 CB CD4+ T cells and allogeneic stimulators at effecter to target (E/T) cell ratios ranging from 1:10 to 1:2500 (in triplicate). Cells were pulsed with [methyl-3H]thymidine (1 μCi [0.037 MBq]/well; Amersham Pharmacia Biotech) for 16 hours before the end of the culture on day 6 and harvested onto glass fiber filter. Incorporated thymidine was measured using a scintillation counter (Microbeta; Wallac, Turku, Finland).
Also, 3 × 106 CB CD4+ T cells (donor A) were cultured with 3 × 105 different subsets of allogeneic DCs (donor B) in 6-well plates for 7 days. T cells (donor A) were harvested, washed, and restimulated at 2.5 × 104 cells/well with GM-CSF/IL-4–induced mature DCs (donor B) at an E/T ratio of 1:5. T-cell proliferation was measured by pulsing cells with [methyl-3H]thymidine (1 μCi [0.037 MBq]/well) for 16 hours before the end of culture on day 6. In another experiment, harvested T cells (2.5 × 104/well from donor A) were added into an independently set-up MLR containing naive CD4+ T cells (5 × 104/well; donor A) and GM-CSF/IL-4–induced mature DCs (5 × 103/well; donor B) to examine whether harvested T cells could suppress the independently set-up MLR. T-cell proliferation was measured by pulsing cells with [methyl-3H]thymidine (1 μCi [0.037 MBq]/well) for 16 hours before the end of culture on day 6.
Preparation of cell lysates and Western blotting
M-DCs and GM-DCs (1 × 106/mL) were stimulated with 1 μg/mL LPS in signaling buffer (RPMI medium with 0.5% endotoxin-free BSA and 25 μM Hepes) for 15 and 30 minutes. Cell pellets were solubilized in lysis buffer (10 mM Tris/HCl, 1 mM EDTA, 200 mM NaCl, 10% glycerol, 0.5% NP40, 5 mM NaF, 0.5 mM NaVO4, 1 mM DTT, 1 mM PMSF, and protease inhibitors) on ice for 30 minutes. Equal amounts of protein, as determined by Bio-Rad protein assay (Hercules, CA), were electrophoresed on 12% sodium dodecyl sulfate–polyacrylamide gel electrophoresis (SDS-PAGE) gels and transferred to PVDF membranes for Western blot analysis. Briefly, PVDF membranes were incubated with TBS super-blocking buffer (Pierce, Rockford, IL) for 1 hour, and then incubated overnight at 4°C with Abs against p-ERK, p-JNK, and p-P38 (Cell Signaling, Beverly, MA). Immunoreactive bands were detected by HRP-labeled goat antirabbit Ab (Cell Signaling), visualized by Supersignal West Pico Chemiluminescent Substrate (Pierce), and quantified by densitometry. Membranes were stripped and reprobed with Abs against total ERK as loading controls.
Statistical analysis
A 2-tailed paired Student t test (unless otherwise indicated) was used to determine statistical significance. Values of P less than .05 were considered significant.
Results
Effects of TGF-β1 on CB and AB M-CSF/IL-4–induced M-DC differentiation
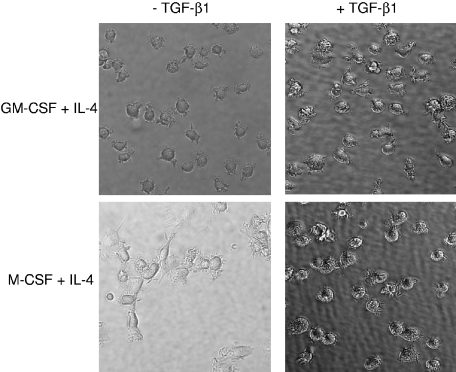
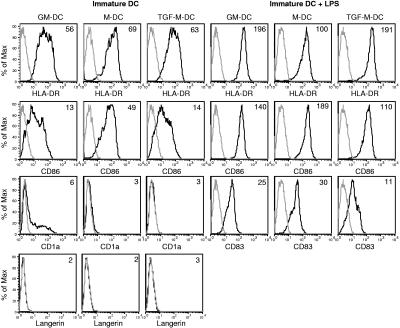
We previously reported that CB monocytes cultured with M-CSF and IL-4 (M-DCs) differentiated into a tolerogenic population of cells, but with a heterogeneous morphology.8 In this report, we analyzed effects of TGF-β1 on M-DC differentiation. Addition of TGF-β1 to highly purified CB monocytes cultured with M-CSF and IL-4 (TGF-M-DCs) induced homogeneous cell morphology similar to that of cells cultured with GM-CSF and IL-4 (GM-DCs), as well as cells cultured with GM-CSF, IL-4, and TGF-β1 (TGF-GM-DCs) (Figure 1). TGF-M-DCs expressed reduced surface levels of CD86 compared with M-DCs. After LPS activation, TGF-M-DCs acquired significantly increased expression of CD86, HLA-DR, and CD83, although CD86 and CD83 were expressed at a lower level than on M-DCs (Figure 2). TNF-α in addition to LPS did not make any noticeable phenotypic changes in the TGF-M-DCs (data not shown), suggesting that LPS alone is able to induce activation of TGF-M-DCs. TGF-β1 is known to induce Langerhans cells from CD14+ cells.17,18 However, CB TGF-M-DCs did not show any phenotypic criteria of Langerhans cells in that they did not express either CD1a or langerin on their surface (Figure 2). AB monocytes cultured with M-CSF, IL-4, and TGF-β also gave rise to a homogeneous population of cells with DC morphology. Analysis of phenotype showed the expression of HLA-DR, CD86, and minimal level of CD1a on their surface. LPS acted by significantly up-regulating surface level of HLA-DR, CD86, and CD83 on adult TGF-M-DCs (data not shown).
Figure 1.
TGF-β1 induces a homogeneous DC morphology for M-DCs. CB monocytes were cultured with GM-CSF and IL-4 or M-CSF and IL-4 to generate GM-DCs and M-DC, respectively (left panels). TGF-β1 was added into GM-DC and M-DC cultures at the beginning of cell culture (right panels). Pictures were taken on day 5 of culture. Results are representative of more than 10 independent experiments. Cell morphology and photographs were observed and taken under a Zeiss Axiovert 25 inverted fluorescence light microscope (Carl Zeiss Microimaging, Thornwood, NY) with a CCD digital camera and computer for image analysis. Cell photographs were taken at a magnification of 400×.
Figure 2.
Effects of TGF-β1 on phenotypic markers of M-DCs. CB monocytes were cultured with M-CSF and IL-4 ± TGF-β1 for 5 to 6 days. LPS was added on the last day of cell culture. Cells were stained with CD1a, CD80, CD86, CD207 (langerin), HLA-DR, and CD83. Gray line designates isotype control. The black area represents indicated molecules. The mean fluorescence intensities of indicated molecules are shown on the upper right corner of the histograms. Results are representative of 3 to 5 independent experiments.
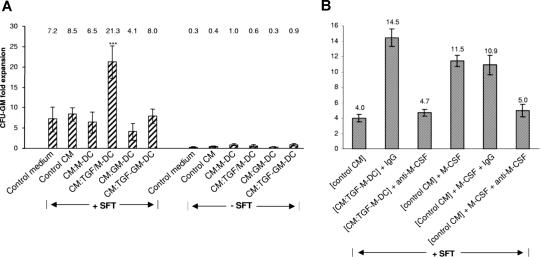
Conditioned medium (CM) collected from LPS-stimulated CB TGF-M-DCs enhances ex vivo expansion of myeloid progenitors in combination with SCF, FL, and TPO (SFT)
To determine if DCs could modulate ex vivo expansion of hematopoietic progenitors by themselves or in the presence of the potent cytokine combination of SFT, CM was generated from the 4 different types of DCs described in Figure 1 after maturation of these cells with LPS. CM from these DCs were compared for their capacity to expand CB myeloid progenitors in the absence and presence of SFT (Figure 3). Fold expansion of CFU-GMs in the presence of SFT using medium conditioned by LPS in the absence of cells (control CM) was similar to that of control culture medium (8.5- vs 7.2-fold expansion; P > .05) (Figure 3A). Of the CM produced by the 4 types of DCs, only CM from mature TGF-M-DCs significantly enhanced expansion of CFU-GM above that of the control medium. None of the CM significantly expanded CFU-GM numbers in the absence of SFT.
Figure 3.
Enhancing effects of conditioned medium produced by mature (LPS-stimulated) TGF-M-DCs on expansion of CFU-GM progenitors from CB. (A) CM from TGF-M-DCs selectively expands CFU-GM ex vivo in synergy with SFT. Freshly isolated CD34+ cells (1 × 104/mL) were incubated with CM from M-DCs, TGF-M-DCs, GM-DCs, TGF-GM-DCs, control CM, or control medium plus or minus SFT for 1 week. Cells were harvested and plated in triplicate. Fold expansion of CFU-GMs after 1-week culture was determined. Data represent a summary of CM from 8 different CB donors. Average fold expansion of CFU-GMs is shown on the top of each bar. (B) Neutralizing anti–M-CSF Ab, but not control Ab, blocks the ex vivo myeloid-enhancing activity of TGF-M-DC CM. Isolated CD34+ cells (1 × 104/mL) were cultured with those factors as indicated on the x-axis in the presence of SFT for 1 week. Fold expansion of CFU-GMs after 1-week culture is shown on the y-axis. The average fold-expansion level of CFU-GMs is shown on the top of each bar. The data represent an average plus or minus SEM from 4 experiments for the neutralizing anti–M-CSF and 2 experiments for the recombinant M-CSF.
In further experiments, CM from LPS-stimulated CB and AB TGF-M-DCs and TG-GM-DCs were compared for effects on ex vivo expansion of CB CFU-GMs. In the absence of CM from DCs, the combination of cytokines (SFT) caused a 4.5 plus or minus 0.3-fold expansion of CFU-GMs (N = 4; compared with control medium with or without LPS, P < .001). Only CM from CB TGF-M-DCs in combination with SFT significantly enhanced ex vivo expansion of CFU-GMs above that of SFT (2.0 ± 0.1-fold; N = 2). CM from CB TGF-GM-DCs (1.07- to 1.2-fold; N = 2) or AB TGF-M-DCs or TGF-GM-DCs (0.93- to 0.98-fold; N = 3 each) had no significant enhancing effects above that of SFT. Thus, ex vivo enhancing effects seem to be confined to CB TGF-M-DCs.
Assessment of the types of cells making up the CFU-GM colonies after expansion culture with SFT in the absence and presence of CM from the different types of DCs demonstrated neutrophil, macrophage, and mixed neutrophil-macrophage colonies. As M-CSF is a cytokine acting on macrophage and mixed neutrophil macrophage progenitors, we added a neutralizing Ab against M-CSF or control Ab at the initiation of the 1-week expansion cultures consisting of SFT and TGF-M-DC CM. Neutralizing anti–M-CSF Ab, but not control IgG, completely blocked TGF-M-DC CM-induced enhancement in expansion of myeloid progenitors (Figure 3B). Also, adding rhM-CSF (100 ng/mL) at the initiation of the 1-week expansion culture consisting of SFT in the absence of CM significantly enhanced ex vivo expansion of CFU-GM progenitors. This did not reach the level achieved by TGF-M-DC CM. M-CSF–enhanced ex vivo expansion of CFU-GMs was blocked by anti–M-CSF, but not control Ab (Figure 3B). After treatment with anti–M-CSF or control Ab, the cultures expanded with mature TGF-M-DC– produced CFU-GM colonies containing mainly macrophages or mixed neutrophils and macrophages. These results suggested that M-CSF present in mature TGF-M-DC CM contributed to expansion of these myeloid progenitors. However these results suggest that M-CSF was not the only cytokine in mature TGF-M-DC CM responsible for the enhanced ex vivo expansion of CFU-GMs.
Cytokine levels in mature TGF-M-DC CM were quantified using microSpot ELISA technology and mature M-DC CM was analyzed as a control. Results of the cytokine analysis are summarized in Table 1. Interestingly, a number of the cytokines analyzed (IL-Iβ, IL-6, IL-10, GM-CSF, and VEGF) were significantly lower in mature TGF-M-DC CM compared with mature M-DC CM, or were not significantly different between the 2 groups. Of interest, the amount of M-CSF found in the CM from both sets of mature DCs was very low and not significantly different. Thus, while it is clear from the antibody studies shown in Figure 3B that M-CSF was involved in the enhanced expansion of CFU-GMs by the mature TGF-M-DC CM, it was not M-CSF alone that was responsible for the enhancement. M-CSF had to be manifesting its effect in combination with one or more cytokines present in the mature TGF-M-DC CM (including possibly factors we did not evaluate in the CM) and/or with SCF, FL, and/or TPO to synergistically enhance ex vivo expansion. Among the cytokines assessed in the DC CM, a number of them (including IL-1, IL-10, TNF-α, and VEGF) are known to suppress proliferation of CFU-GMs either directly or through induction of release of other cytokines with suppressive activity.19 Since the levels of myeloid-suppressive cytokines in the mature TGF-M-DCs were below that present in the mature M-DC CM, which did not enhance ex vivo expansion, it is possible that decreased levels of some suppressive cytokine might also be responsible at least in part for the enhanced activity of the mature TGF-M-DC CM.
Table 1.
A comparative analysis of cytokines released by LPS-activated M-DCs and TGF-M-DCs
| Cytokines, pg/mL |
||
|---|---|---|
| CM: mature (LPS-stimulated) M-DCs | CM: mature (LPS-stimulated) TGF-M-DCs | |
| Significant decrease from M-DCs to TGF-M-DCs | ||
| IL-1β | 17 ± 2 | ND* |
| IL-6 | 12804 ± 3186 | 4092 ± 987* |
| IL-10 | 3798 ± 736 | 1218 ± 415* |
| GM-CSF | 179 ± 10 | 58 ± 9* |
| VEGF | 588 ± 232 | 82 ± 25† |
| No change from M-DCs to TGF-M-DCs | ||
| SDF-1α | 750 ± 543 | 325 ± 192 |
| TGFβ | 13 ± 8 | 5 ± 3 |
| TPO | ND | 7687 ± 6556 |
| PDGF-BB | 200 ± 78 | 374 ± 87 |
| IL-2 | 7 ± 1 | 7 ± 1 |
| M-CSF | ND | 2 ± 2 |
| IL-3 | ND | ND |
| IL-12 | ND | ND |
| IL-17 | ND | ND |
ND indicates nondetectable in all 4 donor samples.
P < .05 when using 2-tailed t test.
P < .05 when using 1-tailed t test.
A comparison of CM prepared from mature TGF-M-DCs to that prepared from mature TGF-GM-DCs also showed no significant difference in release of M-CSF. Here the TGF-M-DCs showed significantly less release of IL-1, IL-6, GM-CSF, and VEGF, but increased IL-10 compared with that released by TGF-GM-DCs (Table 2). The results suggest again that M-CSF is not the only player in the enhanced expansion capability of the mature TGF-M-DC CM.
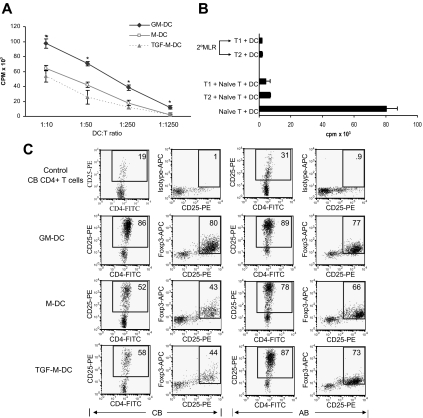
LPS-activated TGF-M-DCs induce T-cell tolerance/regulatory T cells
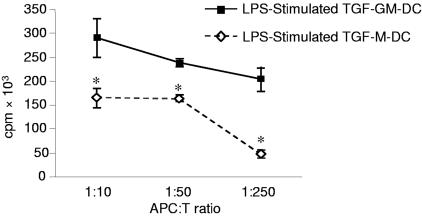
Since a possible advantage of M-DCs is that they might have tolerogenic potential even in their mature form, we examined effects of TGF-M-DCs in regulation of T-cell proliferation and tolerance in their mature form compared with that of mature M-DCs. LPS-activated TGF-M-DCs displayed similar effect in inducing allogeneic MLR to LPS-stimulated M-DCs, both at reduced potency compared with LPS-activated GM-DCs (Figure 4A).
Figure 4.
Effect of mature (LPS-induced) TGF-M-DCs, in comparison with mature M-DCs, in regulation of T-cell proliferation and tolerance. (A) Mature TGF-M-DCs are similar to mature M-DCs in induction of allogeneic MLR, both at lower efficiency than mature GM-DCs in MLR. LPS-activated TGF-M-DCs, M-DCs, and GM-DCs were stimulated with allogeneic naive CD4+ T cells for 6 days. T-cell proliferation was determined by [methyl-3H]thymidine incorporation for the last 16 hours of cell culture. (B) TGF-M-DCs induce T-cell tolerance/regulatory T cells with similar efficiency to that of M-DCs. T1 and T2 are naive CD4+ T cells (donor A) prestimulated with mature TGF-M-DCs or M-DCs (donor B) for 7 days. T1 and T2 (2.5 × 104) were restimulated with allogeneic GM-CSF/IL-4–induced DCs in secondary MLR, and both of T1 and T2 were hyporesponsive T cells (top panel). Also, T1 and T2 (2.5 × 104) were added to another MLR containing naive CD4+ T cells (5 × 104; donor A) and GM-CSF/IL-4–induced DCs (5 × 103; donor B) (bottom panel). Proliferation of T cells was determined by [3H]thymidine incorporation after 6 days of culture. Results are representative of 3 independent experiments. (C) CB CD4+ T cells were cocultured with LPS-activated GM-DCs, M-DCs, and TGF-M-DCs derived from both CB and AB in MLR for 7 days. Cells were harvested and stained with anti–CD4-FITC, anti–CD25-PE, and intracellular anti–Foxp3-APC. The top row is CD4+ T cells isolated from CB stained with anti-CD4, anti-CD25, and isotype control IgG for APC. The percentages of gated cell population are shown on the upper-right corner of dot plots. Results are one representative of 3 CB and 6 AB.
To analyze whether mature TGF-M-DCs could induce inhibitory T cells, naive CD4+ T cells were cultured for 7 days with LPS-activated M-DCs or TGF-M-DCs. T cells harvested at the end of culture were respectively denoted T1 (cultured with LPS-activated TGF-M-DCs) and T2 (cultured with activated M-DCs). First, T1 and T2 cells were restimulated with GM-CSF/IL-4–induced DCs in a secondary MLR. Results shown in Figure 4B (top panel) demonstrated that both T1 and T2 cells were hyporesponsive T cells in secondary MLR. Second, T1 and T2 cells were added into an independently set-up MLR containing naive CD4+ T cells and allogeneic GM-CSF/IL-4–induced DCs to assay whether T1 and/or T2 cells could suppress the MLR. Results shown in Figure 4B (bottom panel) revealed that both T1 and T2 cells significantly suppressed the independently set-up MLR. These results demonstrated that both LPS-activated TGF-M-DCs and M-DCs induced a population of regulatory T cells from the 3 donors tested. There-fore, LPS-activated TGF-M-DCs had similar potency in induction of T-cell tolerance/or regulatory T cells as that of M-DCs.
Foxp3, a transcription factor, is known to play a critical role for regulatory T-cell function.20 Thus, we determined Foxp3 expression in the T cells recovered from MLR by 3-color staining with antibodies against CD4, CD25, and Foxp3. Results (Figure 4C left 2 panels) showed that activated GM-DCs derived from CB induced allogeneic CB CD4+ T cells to express the highest level of CD25 and Foxp3 among the 3 types of DCs tested (GM-DCs, M-DCs, and TGF-M-DCs). Costaining of CD25 and Foxp3 indicated that Foxp3 was exclusively expressed in activated CD25+ T-cell subsets. Therefore, the expression level of Foxp3 is highly correlated with the activation status of CD4+ T cells. CB T cells cultured with TGF-M-DCs and M-DCs were less well activated with reduced expression of both CD25 and Foxp3. These results further indicated that CB TGF-M-DCs and M-DCs were less stimulatory. However, regulatory capacity of TGF-M-DCs could not be further confirmed by phenotypic analysis due to the lack of a reliable phenotypic marker for in vitro–activated human regulatory T cells. This information is supported by the previous reports that human CD4+ T cells induce Foxp3 expression simply by activation, and thus human Foxp3+CD4+ T cells are not necessarily regulatory T cells.21,22 In contrast, TGF-M-DCs and M-DCs generated from AB were not consistently less stimulatory than adult GM-DCs in terms of expression level of CD25 and Foxp3 (Figure 4C right 2 panels). TGF-M-DCs derived from 3 of 6 AB donors we tested were capable of inducing marked levels of CD25 and Foxp3 expression on CB CD4+ T cells at a comparable level with GM-DCs (data not shown).
LPS-activated TGF-M-DCs are less immune active than mature TGF-GM-DCs: effects associated with enhanced LPS activation of the MAPK pathway in TGF-M-DCs
We previously reported that M-DCs produced in the presence of M-CSF and IL-4 were more anti-inflammatory than GM-DCs. We now tested whether in the presence of TGF-β, such differences between M-CSF– and GM-CSF–induced DCs still exist. Results in Figure 5 show that TGF-M-DCs displayed reduced capability in induction of allogeneic MLR compared with TGF-GM-DCs. The LPS-induced TGF-M-DCs secreted greater amounts of immune-suppressive cytokine IL-10, but lower amounts of inflammatory cytokines (IL-1, IL-6, GM-CSF, and VEGF) than mature TGF-GM-DCs (Table 2). This suggests that M-CSF–induced DCs might generally be more favorable than GM-CSF–induced DCs for silencing the immune system, regardless of whether these DC populations are produced in the presence of TGF-β.
Figure 5.
Mature TGF-M-DCs are less efficient in induction of allogeneic MLR than mature TGF-GM-DCs. LPS-activated mature TGF-M-DCs and TGF-GM-DCs were stimulated with allogeneic naive CD4+ T cells for 6 days. T-cell proliferation was determined by [methyl-3H]thymidine incorporation assay. Data are representative of 3 independent experiments.
Table 2.
Comparative analysis of cytokines released by LPS-activated TGF-GM-DCs and TGF-M-DCs
| Cytokines, pg/mL |
||
|---|---|---|
| CM: mature (LPS-stimulated) TGF-GM-DCs | CM: mature (LPS-stimulated) TGF-M-DCs | |
| Significant decrease of TGF-M-DCs to TGF-GM-DCs | ||
| IL-1β | 86 ± 4 | 3 ± 3* |
| IL-6 | 50305 ± 1282 | 20661 ± 2251† |
| GM-CSF | 559 ± 67 | 40 ± 14* |
| VEGF | 103 ± 4 | 15 ± 15† |
| Significant increase when comparing TGF-M-DCs to TGF-GM-DCs: IL-10 | 195 ± 115 | 829 ± 251* |
| No significant change from TGF-GM-DCs to TGF-M-DCs | ||
| TGF-β | 41 ± 13 | 27 ± 3 |
| M-CSF | 13 ± 13 | 34 ± 34 |
| PDGF-BB | 242 ± 101 | 151 ± 151 |
| IL-2 | 12 ± 1 | 22 ± 13 |
| IL-3 | ND | ND |
| IL-12 | 40 ± 40 | ND |
| IL-17 | ND | ND |
Conditioned medium prepared from 5 × 105 cells/mL. Data represent average cytokine levels of triplicate ± SEM from 4 different donors.
ND indicates nondetectable in all 4 donor samples.
P < .05 when using 2-tailed t test.
P < .05 when using 1-tailed t test.
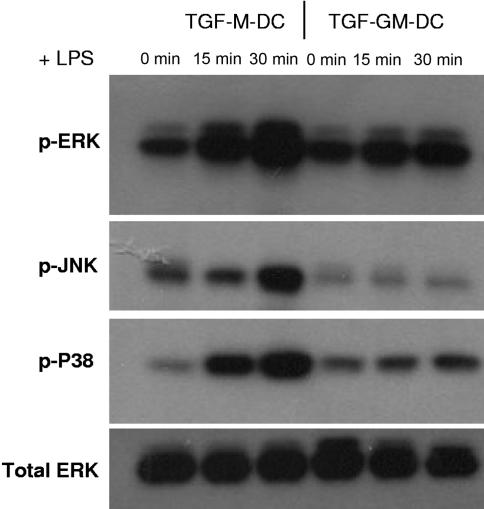
To begin to understand the potential intracellular molecules that might underlie functional differences between M-CSF– and GM-CSF–induced DCs in response to maturation signals, we examined activation of the 3 members of MAPK pathway (ERK, JNK, P38) by LPS. Since TGF-M-DCs, compared with M-DCs, have similar tolerance potential but are homogeneous in morphology, less adherent for easy handling and myeloid promoting, we chose to study the MAPK pathways in M-CSF– and GM-CSF–induced DCs cultured in the presence of TGF-β. LPS induced dramatically increased phosphorylation of ERK, JNK, and p38 in TGF-M-DCs compared with TGF-GM-DCs (Figure 6), suggesting that enhanced MAPK activity in TGF-M-DCs might play a role in their unique functions. We found that the ERK-specific inhibitor U0126 suppressed LPS-induced secretion of TGF-β in TGF-M-DC–derived cells (Table 3). In contrast, this ERK inhibitor suppressed TGF-β, IL-6, and IL-1-β, and increased GM-CSF by TGF-GM-DCs from the same donors. These results suggest that the ERK inhibitor differently regulates cytokine production by TGF-M-DCs and TGF-GM-DCs. Thus, within the MAPK pathway, at least enhanced ERK signaling in TGF-M-DCs might be involved in quantitative cytokine differences we observed between mature populations of TGF-M-DCs and TGF-GM-DCs.
Figure 6.
TGF-M-DCs respond to LPS with markedly enhanced phosphorylation of members of MAPK pathway (ERK, JNK, and p38) compared with TGF-GM-DCs. TGF-M-DCs and TGF-GM-DCs were either not treated (as a control) or treated side by side for 15 and 30 minutes with LPS. Cell lysate was subjected to Western blotting using rabbit polyclonal antibodies specific for p-ERK, -JNK, or -P38. PVDF membranes were stripped and reprobed with a rabbit polyclonal antibody specific for total ERK as a loading control.
Table 3.
Effects of ERK inhibitor on cytokine production by TGF-M-DCs and TGF-GM-DCs
| ERK inhibitor |
||
|---|---|---|
| − | + | |
| Cytokines decreased by ERK inhibitor | ||
| CM: TGF-M-DCs, pg/mL | ||
| TGFβ | 41 ± 13 | 9 ± 9† |
| IL-6 | 20661 ± 2251 | 9757 ± 3613 |
| CM: TGF-GM-DCs, pg/Ml | ||
| TGFβ | 27 ± 3 | 0 ± 0* |
| IL-6 | 50305 ± 1282 | 23300 ± 5558† |
| IL-1β | 86 ± 4 | 12 ± 6* |
| SDF-1 α | 725 ± 265 | 176 ± 135 |
| Cytokines increased by ERK inhibitor | ||
| CM: TGF-M-DCs, pg/mL | ||
| GM-CSF | 40 ± 14 | 155 ± 67 |
| CM: TGF-GM-DCs, pg/mL | ||
| GM-CSF | 559 ± 67 | 720 ± 72* |
| Cytokines unchanged by ERK inhibitor | ||
| CM: TGF-M-DCs, pg/mL | ||
| VEGF | 15 ± 15 | 33 ± 2 |
| PDGF-BB | 151 ± 151 | 350 ± 60 |
| IL-1β | 3 ± 3 | 4 ± 4 |
| SDF-1α | 1141 ± 139 | 1358 ± 159 |
| CM: TGF-GM-DCs, pg/mL | ||
| VEGF | 103 ± 4 | 117 ± 23 |
| PDGF-BB | 242 ± 101 | 363 ± 64 |
Cytokine levels were detected on protein array slides in triplicate for each sample treated ± ERK inhibitor U0126. Data represent average cytokine levels from triplicate samples ± SEM from 2 donors.
P < .05 when using 2-tailed paired t test.
P < .05 when using 1-tailed paired t test.
Discussion
In the present study, we demonstrated that TGF-β1, in combination with M-CSF and IL-4, induced CB monocytes to differentiate into a novel type of DCs (TGF-M-DCs) with the capability of enhancing expansion of myeloid progenitors ex vivo and inducing immune cell tolerance in vitro. These observations, combined with our previous reports on M-DCs,8 indicate that CB M-CSF–induced DCs might be more appropriate for silencing unwanted immune responses, such as in transplantation or autoimmune diseases. Major differences between M-CSF– and GM-CSF–induced DCs lie in their activities upon LPS-induced maturation. M-CSF–induced DCs produced enhanced amounts of anti-inflammatory/inflammatory cytokines and more potently induced T-cell tolerance upon LPS stimulation. AB M-CSF–induced DCs might not be as efficient and consistent as CB M-CSF–induced DCs in the context of silencing immune responses in that they could be potent enough to induce T-cell activation. It remains unsolved whether the Foxp3+CD4+ T cells generated by coculture with CB TGF-M-DCs and M-DCs represent prototype Foxp3+ regulatory T cells. This is due to the fact that Foxp3 could be induced merely by T-cell activation, an observation consistent with recent reports.21,22 However, the fact that Foxp3 is up-regulated by T-cell activation does not necessarily rule out the possibility that Foxp3 expressed in the CD4+ T cells cocultured with CB TGF-M-DCs might act tolerogenically. More reliable phenotypic markers for regulatory T cells would allow us to define the nature of the inhibitory CD4+ T cells we developed using TGF-M-DCs from CB.
M-CSF might be an important growth factor for inhibitory DC development in vivo. In line with this speculation, it was recently reported that M-CSF–deficient mice had reduced numbers of DCs.23 M-CSF levels are elevated in immune-suppressive conditions such as pregnancy, neonatal CB, and tumors.24–27 It is known that immature DCs induce tolerance, while mature DCs induce T-cell activation. Biochemical analysis showed that M-CSF–induced TGF-M-DCs respond to LPS with enhanced activation of the 3 MAPK family members, ERK, JNK, and p38. This suggests that the enhanced tolerance function of TGF-M-DCs is not due to inability to respond to maturation signals or to differentiation into a mature form. MAPK signaling is likely to contribute, at least in part, to the functional differences between M-CSF– and GM-CSF–induced DCs. ERK inhibitor inhibited TGF-β but increased GM-CSF expression by both TGF-M-DCs and TGF-GM-DCs. As TGF-M-DCs produced increased levels of TGF-β, but decreased level of GM-CSF, increased ERK signaling in TGF-M-DCs might play a role in preferential production of TGF-β, but diminished production of GM-CSF.
Cytokines/growth factors regulate hematopoiesis.19,28,29 Due to the potential therapeutic value of tolerogenic DCs in transplantation, we considered it an important goal to investigate the capability of tolerogenic DCs to modulate hematopoiesis. Of particular interest, CB TGF-M-DCs were the only DC type that released factors that enhanced SFT-induced ex vivo expansion of myeloid progenitors. The blocking effects of neutralizing Ab against M-CSF suggest that M-CSF is involved in this expansion, but is not the only factor involved. In other words, the very low levels of M-CSF present in the CM may be acting in synergy with other cytokines present in the CM or cultures, or alternatively, higher levels of M-CSF may be produced endogenously by CD34+ or other cells cocultured with TGF-M-DC CM during the first week of expansion. Quantitative protein array analysis identified previously known cytokines produced by DCs in response to LPS (IL-1, IL-6, IL-10, TGF-β, GM-CSF, M-CSF) as well as cytokines/growth factors not previously reported to be produced by DCs (IL-2, SDF-1α, and PDGF). Among the cytokines detected, IL-6 and SDF-1 promote the expansion or survival of hematopoietic progenitors, while IL-1 and VEGF could be hematopoietic suppressive. The quantitative cytokine profile of factors released by TGF-M-DCs in response to LPS could account for the myeloid-supporting activity of CB TGF-M-DCs, although all the actual players involved in the expansion are not yet clear. Based on the cytokine profile we analyzed, we reasoned that M-CSF, in synergy with a moderate level of hematopoietic-supportive factors (IL-6 and SDF-1) and minimal level of hematopoietic-suppressive factors (IL-1 and VEGF), detected in TGF-M-DC CM could contribute to the overall myeloid expansion effect of TGF-M-DC CM we observed ex vivo in synergy with SFT. Overall, CB TGF-M-DCs might be therapeutically desirable accessory cells in CB transplantation by enhancing myeloid expansion of hematopoietic progenitors, thus facilitating myeloid recovery and, at the same time, inducing immune tolerance.
Acknowledgments
This work was supported by US Public Health Service–National Institutes of Health (NIH) grants R01 HL56416 and R01 HL67384 (H.E.B.), and Project no. 1 (PO1) HL053586 (H.E.B.).
Footnotes
An Inside Blood analysis of this article appears at the front of this issue.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Authorship
Contribution: G.L. and H.E.B. designed and performed the study, analyzed the data, and drafted the paper; T.B.C., S.I., B.G.-E., and S.C. performed the study; S.A. and Y.-J.K. performed the study and analyzed the data. G.L. and Y.-J. K. contributed equally to this work.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Hal E. Broxmeyer, Walther Oncology Center, Indiana University School of Medicine, 950 West Walnut St, R2–302, Indianapolis, IN 46202-5181; e-mail: hbroxmey@iupui.edu.
References
- 1.Steinman RM. The dendritic cell system and its role in immunogenicity. Annu Rev Immunol. 1991;9:271–296. doi: 10.1146/annurev.iy.09.040191.001415. [DOI] [PubMed] [Google Scholar]
- 2.Steinman RM, Hawiger D, Nussenzweig MC. Tolerogenic dendritic cells. Annu Rev Immunol. 2003;21:685–711. doi: 10.1146/annurev.immunol.21.120601.141040. [DOI] [PubMed] [Google Scholar]
- 3.Sato K, Yamashita N, Baba M, Matsuyama T. Regulatory dendritic cells protect mice from murine acute graft-versus-host disease and leukemia relapse. Immunity. 2003;18:367–379. doi: 10.1016/s1074-7613(03)00055-4. [DOI] [PubMed] [Google Scholar]
- 4.Fugier-Vivier IJ, Rezzoug F, Huang Y, et al. Plasmacytoid precursor dendritic cells facilitate allogeneic hematopoietic stem cell engraftment. J Exp Med. 2005;201:373–383. doi: 10.1084/jem.20041399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sato K, Yamashita N, Baba M, Matsuyama T. Modified myeloid dendritic cells act as regulatory dendritic cells to induce anergic and regulatory T cells. Blood. 2003;101:3581–3589. doi: 10.1182/blood-2002-09-2712. [DOI] [PubMed] [Google Scholar]
- 6.Huang Q, Liu D, Majewski P, et al. The plasticity of dendritic cell responses to pathogens and their components. Science. 2001;294:870–875. doi: 10.1126/science.294.5543.870. [DOI] [PubMed] [Google Scholar]
- 7.Wang Q, Zhang W, Ding G, et al. Dendritic cells support hematopoiesis of bone marrow cells. Transplantation. 2001;72:891–899. doi: 10.1097/00007890-200109150-00026. [DOI] [PubMed] [Google Scholar]
- 8.Li G, Kim YJ, Broxmeyer HE. Macrophage colony-stimulating factor drives cord blood monocyte differentiation into IL-10(high)IL-12absent dendritic cells with tolerogenic potential. J Immunol. 2005;174:4706–4717. doi: 10.4049/jimmunol.174.8.4706. [DOI] [PubMed] [Google Scholar]
- 9.Geissmann F, Revy P, Regnault A, et al. TGF-beta 1 prevents the noncognate maturation of human dendritic Langerhans cells. J Immunol. 1999;162:4567–4575. [PubMed] [Google Scholar]
- 10.Borkowski TA, Letterio JJ, Farr AG, Udey MC. A role for endogenous transforming growth factor beta 1 in Langerhans cell biology: the skin of transforming growth factor beta 1 null mice is devoid of epidermal Langerhans cells. J Exp Med. 1996;184:2417–2422. doi: 10.1084/jem.184.6.2417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Strobl H, Riedl E, Scheinecker C, et al. TGF-beta 1 promotes in vitro development of dendritic cells from CD34+ hemopoietic progenitors. J Immunol. 1996;157:1499–1507. [PubMed] [Google Scholar]
- 12.Puig-Kroger A, Relloso M, Fernandez-Capetillo O, et al. Extracellular signal-regulated protein kinase signaling pathway negatively regulates the phenotypic and functional maturation of monocyte-derived human dendritic cells. Blood. 2001;98:2175–2182. doi: 10.1182/blood.v98.7.2175. [DOI] [PubMed] [Google Scholar]
- 13.Hacker H, Mischak H, Hacker G, et al. Cell type-specific activation of mitogen-activated protein kinases by CpG-DNA controls interleukin-12 release from antigen-presenting cells. EMBO J. 1999;18:6973–6982. doi: 10.1093/emboj/18.24.6973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Arrighi JF, Rebsamen M, Rousset F, Kindler V, Hauser C. A critical role for p38 mitogen-activated protein kinase in the maturation of human blood-derived dendritic cells induced by lipopolysaccharide, TNF-alpha, and contact sensitizers. J Immunol. 2001;166:3837–3845. doi: 10.4049/jimmunol.166.6.3837. [DOI] [PubMed] [Google Scholar]
- 15.Broxmeyer HE, Orschell CM, Clapp DW, et al. Rapid mobilization of murine and human hematopoietic stem and progenitor cells with AMD3100, a CXCR4 antagonist. J Exp Med. 2005;201:1307–1318. doi: 10.1084/jem.20041385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Broxmeyer HE, Srour E, Orschell C, et al. Cord blood-derived stem cell progenitor cells. In: Lanza R, Klimanskaya I, editors. Methods in Enzymology. Vol. 419. San Diego, CA: Academic Press, Elsevier Science; 2006. pp. 439–473. [DOI] [PubMed] [Google Scholar]
- 17.Jaksits S, Kriehuber E, Charbonnier AS, et al. CD34+ cell-derived CD14+ precursor cells develop into Langerhans cells in a TGF-β1-dependent manner. J Immunol. 1999;163:4869–4877. [PubMed] [Google Scholar]
- 18.Heinz LX, Platzer B, Reisner PM, et al. Differential involvement of PU. 1 and Id2 downstream of TGF-beta1 during Langerhans-cell commitment. Blood. 2006;107:1445–1453. doi: 10.1182/blood-2005-04-1721. [DOI] [PubMed] [Google Scholar]
- 19.Shaheen M, Broxmeyer HE. The humoral regulation of hematopoiesis. In: Hoffman R, Benz E, Shattil S, Furie B, Cohen H, Silberstein L, McGlave P, editors. Hematology: Basic Principles and Practice. 4th ed. Philadelphia, PA: Elsevier Churchill Livingston; 2005. pp. 233–265. [Google Scholar]
- 20.Zheng Y, Rudensky AY. Foxp3 in control of the regulatory T cell lineage. Nat Immunol. 2007;8:457–462. doi: 10.1038/ni1455. [DOI] [PubMed] [Google Scholar]
- 21.Ziegler SE. Foxp3: not just for regulatory T cells anymore. Eur J Immunol. 2007;37:21–23. doi: 10.1002/eji.200636929. [DOI] [PubMed] [Google Scholar]
- 22.Wang J, Ioan-Facsinary A, van der Voort EI, et al. Transient expression of Foxp3 in human activated nonregulatory CD4+ T cells. Eur J Immunol. 2007;37:129–138. doi: 10.1002/eji.200636435. [DOI] [PubMed] [Google Scholar]
- 23.MacDonald KP, Rowe V, Bofinger HM, et al. The colony-stimulating factor 1 receptor is expressed on dendritic cells during differentiation and regulates their expansion. J Immunol. 2005;175:1399–1405. doi: 10.4049/jimmunol.175.3.1399. [DOI] [PubMed] [Google Scholar]
- 24.Bartocci A, Pollard JW, Stanley ER. Regulation of colony-stimulating factor 1 during pregnancy. J Exp Med. 1986;164:956–961. doi: 10.1084/jem.164.3.956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ikeno K, Koike K, Fukuromoto T, Shimizu T, Nagatomo M, Komiyama A. Increased macrophage-colony stimulating factor levels in neonates with perinatal complications. Early Hum Dev. 1996;46:229–237. doi: 10.1016/0378-3782(96)01766-5. [DOI] [PubMed] [Google Scholar]
- 26.Saito S, Motoyoshi K, Ichijo M, Saito M, Takaku F. High serum human macrophage colony-stimulating factor level during pregnancy. Int J Hematol. 1992;55:219–225. [PubMed] [Google Scholar]
- 27.Scholl SM, Pallud C, Beuvon F, et al. Anti-colony-stimulating factor-1 antibody staining in primary breast adenocarcinomas correlates with marked inflammatory cell infiltrates and prognosis. J Natl Cancer Inst. 1994;86:120–126. doi: 10.1093/jnci/86.2.120. [DOI] [PubMed] [Google Scholar]
- 28.Trey JE, Kushner I. The acute phase response and the hematopoietic system: the role of cytokines. Crit Rev Oncol Hematol. 1995;21:1–18. doi: 10.1016/1040-8428(94)00141-3. [DOI] [PubMed] [Google Scholar]
- 29.Nishikawa SI, Hashi H, Honda K, Fraser S, Yoshida H. Inflammation, a prototype for organogenesis of the lymphopoietic/hematopoietic system. Curr Opin Immunol. 2000;12:342–345. doi: 10.1016/s0952-7915(00)00097-2. [DOI] [PubMed] [Google Scholar]