Abstract
Background: Rehospitalization occurs in approximately 20% of medical inpatients within 90 days of discharge. Rehospitalization accounts for considerable morbidity, mortality, and costs. Identification of risk factors could lead to interventions to reduce rehospitalization. The objective of the study was to determine if physical and mental health, substance abuse, and social support are risk factors for rehospitalization.
Method: This was a prospective cohort study in an innercity population conducted from September 2002 to September 2004. Participants included 144 adult inpatients with at least 1 hospital admission in the past 6 months. Measurements included age, length of stay, number of admissions in the past year, and medical comorbidity as well as measures of depression, alcohol and drug abuse, social support, and health-related quality of life. The outcome studied was the rehospitalization status of participants within 90 days of the index hospitalization.
Results: The mean age of the subjects was 54.8 years; 48% were black and 78% spoke English as a primary language. Subjects were admitted a mean of 2.5 times in the year before the index admission. Sixty-four patients (44%) were subsequently rehospitalized within 90 days after the index admission. In bivariate analysis, rehospitalized patients had more prior admissions (median of 3.0 vs. 2.0 admissions, p = .002), greater medical comorbidity (mean Charlson Comorbidity Index score of 2.6 vs. 2.0, p = .04), and poorer physical functional status (mean SF-12 physical component score of 31.5 vs. 36.2, p = .03). A logistic regression model, including prior admissions in the last year, comorbidity, physical functional status, and depression, showed that depression tripled the odds of rehospitalization (odds ratio = 3.3, 95% CI = 1.2 to 9.3). This model had fair accuracy in identifying patients at greatest risk for rehospitalization (c statistic = 0.72).
Conclusions: Hospitalized patients with a history of prior hospitalization within 6 months who screen positive for depression are 3 times more likely to be rehospitalized within 90 days in this relatively high-risk population. Screening during hospitalization for depressive symptoms may identify those at risk for rehospitalization.
Rehospitalization accounts for considerable morbidity, mortality, and costs and may also be a marker of poor quality health care. Studies of patients discharged from adult inpatient services find 90-day rehospitalization rates between 19% and 23%.1 Rehospitalization can place patients at risk of nosocomial infection, iatrogenic illness, and medical errors.2 By one estimate, rehospitalizations account for as much as half of all hospitalizations.3 In 2003, national health care expenditures in the United States on all hospitalizations were $516 billion,4 so rehospitalization might account for over $250 billion of U.S. national health care expenditures annually. The Agency for Healthcare Research and Quality found that in 1999, 4 states spent $1.9 billion in 6 months on rehospitalization.5 Therefore, even a small reduction in rehospitalization could have an important impact on health care services provision and quality.
Some successes in preventing rehospitalization in specific disorders such as congestive heart failure have been demonstrated, but strategies to prevent rehospitalization have had limited success in adult inpatients with other diagnoses.6 For an intervention aimed at reducing rehospitalization to be practical and cost-effective, there needs to be a reliable means of targeting those patients who are at high risk. Known risk factors for rehospitalization include advanced age, specific diagnoses (such as congestive heart failure), history of prior admission, length of stay, and some measure of the severity of the illness.7,8 However, these factors that are readily available from administrative databases explain only a small amount of the variance in rehospitalization. Predictors of rehospitalization in urban, underserved populations are even less well defined. Efforts to reduce rehospitalization in these populations deserve particular attention because there is evidence that people of lower socioeconomic status experience higher rehospitalization rates.9
We designed a study to assess if measurable behavioral and functional factors help to explain some of the variability in predicting rehospitalization. We hypothesized that depressive symptoms, alcohol and drug abuse, lack of social support, and poor health-related quality of life contribute to an increased risk of rehospitalization in a recurrently admitted, innercity population.
METHOD
Study Setting
This study was conducted on an adult inpatient service that admits from a consortium of 15 community health centers (CHCs) comprising the Boston HealthNet to Boston Medical Center (BMC), an innercity, academic medical center located in Boston, Mass. The Boston HealthNet inpatient service is staffed by family physicians and general internists from the CHCs and family physicians from the Department of Family Medicine at BMC. The study was conducted from September 2002 to September 2004. The institutional review board of Boston University Medical Center approved the study.
Study Design
This was a prospective cohort study. The index admission was the hospitalization during which the patient was enrolled in the study. Trained staff members screened inpatients for eligibility. Patients were eligible if they (1) were admitted to the Boston HealthNet medical inpatient service, (2) were over 18 years of age, (3) had a history of at least 1 hospitalization in the 6-month period before the index admission, (4) had an assigned primary care physician (PCP) at 1 of the CHCs, (5) were willing to be rehospitalized if indicated, and (6) were admitted from a non-institutionalized setting. Patients were excluded if (1) they expressed that they were unwilling or unable to keep appointments with their PCP, (2) rehospitalization was planned (e.g., for diagnostic test or procedure) at the time of enrollment, or (3) they were previously enrolled. Subjects were approached for study enrollment at each admission even if they declined participation at a previous admission.
Data Collection
After obtaining informed consent, research staff members collected demographic data and information about known risk factors for rehospitalization, including age, length of stay of the index admission, and number of admissions in the year before the index admission, and calculated the Charlson Comorbidity Index score10 from review of the hospital record. Research staff then conducted a face-to-face structured interview with the subject that included administering the following validated instruments.
Nine-item Patient Health Questionnaire (PHQ-9). The PHQ-911 uses a 4-point Likert scale and a standard scoring algorithm to diagnose major depression; the screen has been used in numerous studies. The PHQ-9 was developed as a 1-stage, self-report version of the depression section of the previously validated Primary Care Evaluation of Mental Disorders instrument.12 The PHQ-9 demonstrates a sensitivity of 88% and a specificity of 88% for major depression (as compared with mental health professional's diagnoses as the gold standard).11
Alcohol Use Disorders Identification Test (AUDIT). The AUDIT,13 which may be self-administered or administered by an interviewer, consists of 10 questions and takes approximately 3 minutes to complete. The first 8 questions refer to alcohol-related issues over the prior year, and the final 2 include information about previous years. The AUDIT has been extensively researched and validated, demonstrating high correlation with other frequently used instruments such as the Michigan Alcoholism Screening Test.13 Using the traditional cutoff of 8, the test has sensitivity for alcohol abuse or dependence (as defined by DSM-III-R criteria), ranging from 78% to 100%. Specificity values have been lower, ranging from 25% to 96%. Of note, the AUDIT has been validated among adults at an innercity medical clinic serving a population similar to that of BMC. In that population, the instrument was shown to be 96% sensitive for current alcohol abuse or dependence and to accurately distinguish between current and former alcohol-related problems.14 The AUDIT has been used in numerous research projects, including a recent study of a substance abuse treatment system14 accessed through the emergency department at BMC. Given extensive use in populations such as ours and ease of administration, we chose the AUDIT over other screening instruments.13–15
10-item Drug Abuse Screening Test (DAST-10). The DAST-1016 identifies drug use problems using a 10-item screen, with scores greater than 3 suggesting a moderate level of drug-related problems worthy of further investigation. The original DAST 28-item instrument demonstrated excellent content and construct validity and internal consistency ranging from .86 to .95, with an 85% overall accuracy in diagnosing drug abuse or dependence (according to DSM-III criteria), as compared with the Diagnostic Interview Schedule. Both 20-item and 10-item versions of the DAST have been developed. The DAST-20 correlates almost perfectly with the original DAST, and the DAST-10 correlates highly with the 20-item version (r = .98).17 The DAST-10, due to its similarity in structure, has been frequently used with the AUDIT to screen for drug and alcohol–related problems.16
Norbeck Social Support Questionnaire (NSSQ). The NSSQ18 is used to measure multiple dimensions of social support, with the mean (SD) score for the normative population equal to 201.9 (95.9) and higher scores suggesting greater social support. The NSSQ has good internal reliability (correlations ranging from .69 to .98) and test-retest reliability (correlations ranging from .86 to .92).18 The test yields 3 scores (total functional support, total network support, and total loss). The total functional support score was used in this study. The NSSQ has been used in studies of low-income populations and in numerous studies to identify correlations between social support and rehospitalization among patients with ischemic heart disease.18,19
Short Form-12 Health Survey (SF-12). The SF-1220 was developed as a valid abbreviation of the widely used Short Form-36 questionnaire that was designed to accurately measure the physical and mental components of health-related quality of life. Administration of the survey yields 2 scores: the physical component summary (PCS) and the mental component summary (MCS). These scores are scaled on a range of 0 to 100 designed to produce mean scores of 50 and standard deviations of 10 in a representative sample of the U.S. population; higher scores suggest greater functional status. The 2 summary scores offer excellent reliability as measured by the internal consistency method (PCS = 89% and MCS = 86%).20
Independent Variables
Age, length of stay, number of prior admissions, Charlson Comorbidity Index, NSSQ functional scale, and SF-12 PCS and MCS were characterized as continuous variables. The PHQ-9 (major depression), AUDIT (score ≥ 6), and DAST-10 (score ≥ 3) were dichotomized using standardized scoring systems.
Data
Dependent variables. The outcome studied was the rehospitalization status within 90 days of the index hospitalization. Rehospitalization refers to the first hospitalization that occurred for any reason within 90 days after discharge from the index admission. Rehospitalization was determined by review of the hospital database that is available for all patients. To determine if subjects were rehospitalized at another hospital, we contacted all subjects by telephone. If we were unable to contact subjects after 5 telephone calls, then we contacted the alternate contacts, whose information was obtained during study enrollment.
Statistical analyses. Analysis included (1) comparison of subjects who agreed to enroll in the study versus those who refused participation, (2) bivariate comparison of baseline characteristics of rehospitalized subjects versus those not rehospitalized, and (3) bivariate comparison of risk factors for rehospitalization comparing those subjects rehospitalized and not rehospitalized. In these analyses, t test, χ2 test, Fisher exact test, and Wilcoxon rank sum test were used where appropriate, with a p value ≤ .05 used as level of significance.
The final analysis included a series of multivariate logistic regression analyses to determine the odds of rehospitalization after controlling for all independent variables. We used a 3-stage process to develop our logistic models. Model 1 includes risk factors known to be associated with rehospitalization (age, length of index hospital stay, number of hospital admissions in the past year, and Charlson Comorbidity Index score). Model 2 includes all of the psychosocial and functional scales that were hypothesized to contribute to rehospitalization, which included the PHQ-9 (major depression), PHQ-9 (anxiety), AUDIT (alcohol abuse), DAST-10 (drug abuse), NSSQ (social support), and SF-12 PCS and MCS (physical and mental components of health-related quality of life). Finally, model 3 incorporates independent variables found to be related to rehospitalization at the p = .05 level of significance in either the bivariate analysis or in model 1 or model 2. This model includes the number of hospital admissions in the prior year and Charlson Comorbidity Index, SF-12 PCS, and PHQ-9 (major depression) scores. Model 3 is the preferred model, as it provides the most conservative assessment of risk factor performance.
Model performance was assessed by the concordance statistic (c statistic) for discriminative ability (refers to the ability to distinguish high-risk subjects from low-risk subjects). A value of 0.5 indicates no discriminatory power, whereas a c statistic of 1.0 indicates perfect discrimination. Model calibration (refers to whether the predicted probabilities agree with the observed probabilities) was assessed by the Hosmer and Lemeshow goodness-of-fit test. Lack of fit in our models was considered statistically significant if the p value was less than .05. All analyses were done using SAS version 8.02 software (SAS Institute, Inc., Cary, N.C.).
RESULTS
Sample Characteristics
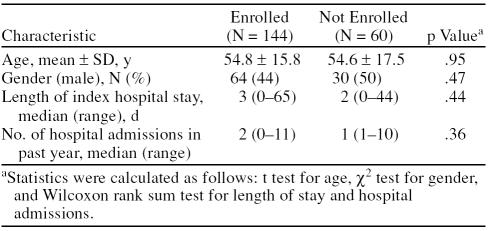
Of 204 eligible subjects who were approached and asked to participate in the study, 144 (71%) were enrolled and 60 (29%) refused. The age, gender, length of index hospital stay, and number of prior admissions in the past year did not differ among enrolled subjects when compared with those who chose not to participate (Table 1). Eligible subjects who previously refused were reapproached at each admission. Enrolled subjects were admitted a mean of 2.5 times in the year before the index admission.
Table 1.
Characteristics of Eligible Subjects Enrolled in the Study Compared With Those Who Refused Participation (N = 204)
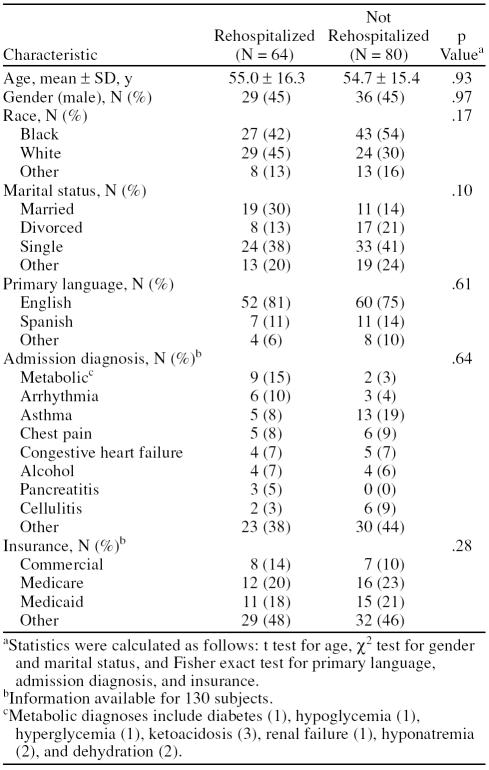
Table 2 shows baseline characteristics of enrolled subjects by rehospitalization status within 90 days of the index hospitalization. For all 144 enrolled subjects, the mean age was 54.8 years, 49% were black, 45% were male, and 78% spoke English as a primary language. Nearly all subjects were insured through commercial insurance, Medicare, or Medicaid. The remainder were either self-pay or covered by the Massachusetts system that provides care to those who otherwise lack coverage.
Table 2.
Baseline Characteristics of Subjects Grouped by Rehospitalization Status Within 90 Days of the Index Hospitalization (N = 144)
Of 144 subjects enrolled, 64 (44%) had at least 1 rehospitalization in the 90 days after discharge from the index admission (median = 1.0, mean = 1.8, range, 1–6). While there were no statistically significant differences, rehospitalized subjects tended to be white, married, and English speaking compared with those not rehospitalized. Nearly half of rehospitalized subjects were originally hospitalized for metabolic diseases (hypoglycemia, hyperglycemia, ketoacidosis, renal failure, hyponatremia, and dehydration), arrhythmias, asthma, chest pain, and congestive heart failure. In subjects who were not rehospitalized, the most common diagnoses included asthma, chest pain, cellulitis, and congestive heart failure.
The group of patients rehospitalized within 90 days was admitted frequently (median of 2 admissions in the past 6 months) and had a high degree of medical and psychosocial risk: 27% met criteria for major depression on the PHQ-9, 18% were at risk of hazardous drinking (AUDIT score ≥ 6), and 6% were at risk of drug-related problems (DAST-10 score ≥ 3). The rehospitalized sample had poor social support (median score of 71 on the NSSQ, while a score of 201.9 was average for a normative population) and reported poor physical health (mean score of 34.2 on the SF-12 PCS, while the mean score of the U.S. population is 50) and poor mental health (mean score of 41.8 on the SF-12 MCS, while the mean score of the U.S. population is 50).
Bivariate Analyses
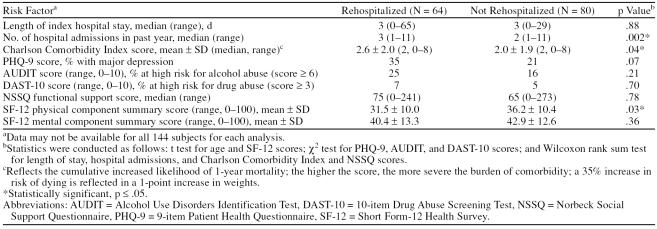
Table 3 shows results of unadjusted bivariate analyses of risk factors for rehospitalization grouped by rehospitalization status. Rehospitalized subjects had a greater number of admissions in the prior year (median of 3.0 vs. 2.0, p = .002), greater medical comorbidity (mean Charlson Comorbidity Index score of 2.6 vs. 2.0, p = .04), and poorer health-related quality of life as measured by the SF-12 PCS (mean score of 31.5 vs. 36.2, p = .03). Rehospitalized subjects also had a greater length of the index admission (mean of 5.1 vs. 4.4 days), were more at risk of hazardous drinking (24.6% vs. 16.0%), or met criteria for major depression (35.0% vs. 21.1%), although these variables were not statistically significant.
Table 3.
Risk Factors for Rehospitalization Grouped by Rehospitalization Status
Predictive Models
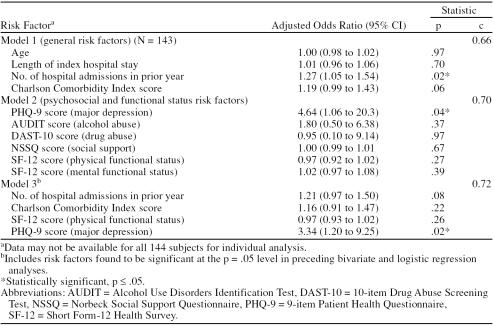
Table 4 shows the adjusted odds ratios from the logistic regression models of risk factors for rehospitalization. In model 1, only the number of hospital admissions in the prior year was significantly related to rehospitalization (OR = 1.27, 95% CI = 1.05 to 1.54). In model 2, major depression was a significant risk factor (OR = 4.6, 95% CI = 1.06 to 20.3). Model 3 included the 4 variables found to be significant in the bivariate analysis or in models 1 or 2. These variables were (1) number of hospital admissions in the prior year, (2) Charlson Comorbidity Index (medical comorbidity), (3) SF-12 PCS (health-related quality of life, physical component summary), and (4) PHQ-9. The odds of rehospitalization were again significantly greater in subjects who screened positive for major depression (OR = 3.3, 95% CI = 1.20 to 9.25). For models 1, 2, and 3, the c statistics were 0.66, 0.70, and 0.72, respectively, and the p values for the Hosmer and Lemeshow goodness-of-fit test were 0.58, 0.15, and 0.35, respectively.
Table 4.
Adjusted Odds Ratios of Risk Factors for Rehospitalization
DISCUSSION
In patients who had a history of hospitalizations in the 6 months prior to the index hospitalization, we found that a positive screen for major depression at admission tripled the odds of being rehospitalized within 90 days of discharge among adult inpatients in an urban academic medical center. While we await further study in randomized intervention trials, clinicians should consider screening for and treating depression in their frequently readmitted inpatients in an effort to reduce medical rehospitalization.
Our findings are supported by the few studies that have examined the association between depression and rehospitalization. A study of medical and surgical inpatients found that depressed patients spent twice as many days rehospitalized over a 4-year period.21 A Swiss study in elderly inpatients found that patients with depressive symptoms had higher inpatient service utilization over a 6-month period.22 Similarly, a case-control study of elderly patients in a Medicare managed care plan found increased odds of unplanned rehospitalization within 30 days if patients had a history of depression (OR = 3.2, 95% CI = 1.4 to 7.9).23 Taken together, our study adds to the literature indicating that depression is a powerful risk factor for rehospitalization. Depression is also associated with worse outcomes after myocardial infarction.24
In a prospective registry of myocardial infarction, depressive symptoms were measured in 1873 patients with the PHQ during hospitalization and 1 month after discharge. In this study, all categories of depression were associated with higher rehospitalization, more frequent angina, more physical limitations, and worse quality of life.24 Depression might lead to rehospitalization through a variety of mechanisms. The neuroendocrine changes seen in depression can worsen physical illness. Depression may impair health-related quality of life leading to lower thresholds for admission. Somatization may be misinterpreted, thereby complicating diagnosis and management.19 Medication nonadherence among patients with mental health diagnoses could lead to rehospitalization.25 Finally, depressed patients might have a reduced social support network leading to increasing stress and worsening of symptoms, thereby lengthening time to recovery and necessitating rehospitalization.26
An array of clinical and administrative factors have been associated with rehospitalization including age, length of stay, number of prior hospital admissions, comorbid medical illness, admitting diagnosis, male sex, white race, Medicaid coverage, single marital status, and laboratory data such as glycosylated hemoglobin.27 However, these factors tend to explain very little of the variation in rehospitalizations.6 Therefore, in this study, we explored the contributions of mental health, substance abuse, social support, and perceived health-related quality of life, which we proposed to be related to rehospitalization and which have been suggested in the medical literature.28–30 Although much of the variability in rehospitalization remains unexplained, these findings support our approach to combine psychosocial and functional determinants of rehospitalization to better understand these complex interactions.
We were successful in identifying a group at high risk of rehospitalization (overall 44% were rehospitalized within 90 days of the index admission). Three factors might explain this finding: (1) the population enrolled had a high degree of medical and psychosocial comorbidities (27% screened positive for major depression, 18% for alcohol abuse, and 6% for risk of drug abuse; many had poor social support and physical health); (2) we only enrolled subjects who had been hospitalized in the last 6 months, a powerful risk factor for rehospitalization3,6; and (3) we reapproached subjects who had declined enrollment at prior admissions at each hospitalization, resulting in a study group with a mean of 2.5 hospitalizations in the year before the index hospitalization. As a result of these 3 factors, we studied subjects at very high risk of rehospitalization. While our inclusion criteria might somewhat limit the generalizability of our results, it is relevant to many hospitals that provide care to similar innercity populations who are frequently hospitalized.
Finally, while our data suggest that more prior admissions, greater length of stay, poorer physical functioning, anxiety disorders, and alcohol use are related to rehospitalizations, we could not confirm our hypotheses regarding these factors in multivariate analysis. Interestingly, we did not find a relationship between social support and rehospitalization. It is possible that our subjects used their supports to facilitate health-seeking behavior leading to rehospitalization. Also, we used the functional support score of the NSSQ in our analyses. If the effect of social support is primarily from aspects of social support we did not analyze (network properties and recent losses), it is possible that we may not have fully accounted for the variance in rehospitalization explained by social support.
A major strength of this study is its prospective design that permits us to describe both the magnitude and direction of causal relationships between factors. This is in favorable contrast to the retrospective designs that are used by a number of prior studies. Limitations of this study include the modest enrollment rate of eligible subjects; however, the fact that age, gender, length of stay, and number of prior admissions did not differ between groups may suggest that subjects were not entirely dissimilar. Finally, we did not consider the quality of care received during the index admission, which has been associated with rehospitalization.31 Despite these limitations, we conclude that hospitalized adults with a history of recent previous hospitalizations who screen positive for major depression are at a 3 times greater risk of being rehospitalized within 90 days of discharge. Future randomized controlled trials designed to treat patients screening positive for major depression in an attempt to reduce rehospitalization should be undertaken. While we await further study in randomized intervention trials, clinicians should consider screening for and treating depression in their frequently readmitted inpatients before discharge in an effort to reduce rehospitalization.
Footnotes
This project was supported by grants numbered 1UC1HS014289-01 and 1U18HS015905-01 from the Agency for Healthcare Research and Quality (Dr. Jack) and grant numbered T32-HP-10028-06 from the U.S. Department of Health and Human Services (Drs. Kartha and Anthony).
Dr. Culpepper has served as a consultant to Wyeth, Pfizer, Forest, and Neurogen and has served on the speakers or advisory boards of Wyeth, Forest, and Pfizer. Drs. Kartha, Anthony, Manasseh, Greenwald, Chetty, Burgess, and Jack report no other financial affiliations relevant to the subject of this article.
REFERENCES CITED
- Smith DM, Giobbie-Hurder A, and Weinberger M. et al. Predicting non-elective hospital readmissions: a multi-site study. Department of Veterans Affairs Cooperative Study Group on Primary Care and Readmissions. J Clin Epidemiol. 2000 53:1113–1118. [DOI] [PubMed] [Google Scholar]
- Kohn LT, Corrigan JM, and Donaldson MS. et al. To Err is Human: Building a Safer Health System. Washington, DC: National Academy Press. 2000 [PubMed] [Google Scholar]
- Hasan M.. Readmission of patients to hospital: still ill defined and poorly understood. Int J Qual Health Care. 2001;13:177–179. doi: 10.1093/intqhc/13.3.177. [DOI] [PubMed] [Google Scholar]
- Centers for Medicare & Medicaid Services. National Health Expenditures Aggregate Amounts and Average Annual Percent Change. by Type of Expenditure: Selected Calendar Years 1980–2003: Office of the Actuary, National Health Statistics Group. 2005 [Google Scholar]
- Friedman B, Basu J.. The rate and cost of hospital readmissions for preventable conditions. Med Care Res Rev. 2004;61:225–240. doi: 10.1177/1077558704263799. [DOI] [PubMed] [Google Scholar]
- Soeken KL, Prescott PA, and Herron DG. et al. Predictors of hospital readmission: a meta-analysis. Eval Health Prof. 1991 14:262–281. [DOI] [PubMed] [Google Scholar]
- Phillips RS, Safran C, and Cleary PD. et al. Predicting emergency readmissions for patients discharged from the medical service of a teaching hospital. J Gen Intern Med. 1987 2:400–405. [DOI] [PubMed] [Google Scholar]
- Librero J, Peiro S, Ordinana R.. Chronic comorbidity and outcomes of hospital care: length of stay, mortality, and readmission at 30 and 365 days. J Clin Epidemiol. 1999;52:171–179. doi: 10.1016/s0895-4356(98)00160-7. [DOI] [PubMed] [Google Scholar]
- Weissman JS, Stern RS, Epstein AM.. The impact of patient socioeconomic status and other social factors on readmission: a prospective study in four Massachusetts hospitals. Inquiry. 1994;31:163–172. [PubMed] [Google Scholar]
- Charlson MEPP, Ales KL, McKenzie CR.. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chron Dis. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JB.. The PHQ-9: validity of a brief depression severity measure. J Gen Int Med. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer RL, Kroenke K, and Williams JB. et al. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA. 1999 282:1737–1744. [DOI] [PubMed] [Google Scholar]
- Allen JP, Litten RZ, and Fertig JB. et al. A review of research on the Alcohol Use Disorders Identification Test (AUDIT). Alcohol Clin Exp Res. 1997 21:613–619. [PubMed] [Google Scholar]
- Bernstein E, Bernstein J, Levenson S.. Project ASSERT: an ED-based intervention to increase access to primary care, preventive services and the substance abuse treatment system. Ann Emerg Med. 1997;30:181–189. doi: 10.1016/s0196-0644(97)70140-9. [DOI] [PubMed] [Google Scholar]
- Fiellin DA, Reid MC, O'Connor PG.. Outpatient management of patients with alcohol problems. Ann Int Med. 2000;133:815–827. doi: 10.7326/0003-4819-133-10-200011210-00015. [DOI] [PubMed] [Google Scholar]
- Gavin DR, Ross HE, Skinner HA.. Diagnostic validity of the drug abuse screening test in the assessment of DSM-III drug disorders. Br J Addict. 1989;84:301–307. doi: 10.1111/j.1360-0443.1989.tb03463.x. [DOI] [PubMed] [Google Scholar]
- Maisto SA, Carey KB, and Gordon CM. et al. Use of the AUDIT and the DAST-10 to identify alcohol and drug use disorders among adults with a severe and persistent mental illness. Psychol Assess. 2000 12:186–192. [DOI] [PubMed] [Google Scholar]
- Norbeck JS, Lindsey AM, Carrieri VL.. Further development of the Norbeck Social Support Questionnaire: normative data and validity testing. Nurs Res. 1983;32:4–9. [PubMed] [Google Scholar]
- Gigliotti E.. A confirmation of the factor structure of the Norbeck Social Support Questionnaire. Nurs Res. 2002;51:276–284. doi: 10.1097/00006199-200209000-00002. [DOI] [PubMed] [Google Scholar]
- Ware JE, Kosinski M, Keller SD.. A 12-item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34:220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- Saravay SM, Pollack S, and Steinberg MD. et al. Four-year follow-up of the influence of psychological comorbidity on medical rehospitalization. Am J Psychiatry. 1996 153:397–403. [DOI] [PubMed] [Google Scholar]
- Bula CJ, Wietlisbach V, and Burnand B. et al. Depressive symptoms as a predictor of 6-month outcomes and services utilization in elderly medical inpatients. Arch Intern Med. 2001 161:2609–2615. [DOI] [PubMed] [Google Scholar]
- Marcantonio ER, McKean S, and Goldfinger M. et al. Factors associated with unplanned hospital readmission among patients 65 years of age and older in a Medicare managed care plan. Am J Med. 1999 107:13–17. [DOI] [PubMed] [Google Scholar]
- Parashar S, Rumsfeld JS, and Spertus JA. et al. Time courses of depression and outcomes of myocardial infarction. Arch Intern Med. 2006 166:2035–2043. [DOI] [PubMed] [Google Scholar]
- Haywood TW, Kravitz HM, and Grossman LS. et al. Predicting the “revolving door” phenomenon among patients with schizophrenic, schizoaffective, and affective disorders. Am J Psychiatry. 1995 152:856–861. [DOI] [PubMed] [Google Scholar]
- Tse WS, Bond AJ.. The impact of depression on social skills. J Nerv Ment Dis. 2004;192:260–268. doi: 10.1097/01.nmd.0000120884.60002.2b. [DOI] [PubMed] [Google Scholar]
- Benbassat J, Taragin M.. Hospital readmissions as a measure of quality of health care: advantages and limitations. Arch Intern Med. 2000;160:1074–1081. doi: 10.1001/archinte.160.8.1074. [DOI] [PubMed] [Google Scholar]
- Brennan PL, Kagay CR, and Geppert JJ. et al. Elderly Medicare inpatients with substance use disorders: characteristics and predictors of hospital readmissions over a four-year interval. J Stud Alcohol. 2000 61:891–895. [DOI] [PubMed] [Google Scholar]
- Pearson S, Stewart S, Rubenach S.. Is health-related quality of life among older, chronically ill patients associated with unplanned readmission to hospital? Aust N Z J Med. 1999;29:701–706. doi: 10.1111/j.1445-5994.1999.tb01618.x. [DOI] [PubMed] [Google Scholar]
- Stewart MJ, Hirth AM, and Klassen G. et al. Stress, coping, and social support as psychosocial factors in readmissions for ischaemic heart disease. Int J Nurs Stud. 1997 34:151–163. [DOI] [PubMed] [Google Scholar]
- Ashton CM, Del Junco DJ, and Souchek J. et al. The association between the quality of inpatient care and early readmission: a meta-analysis of the evidence. Med Care. 1997 35:1044–1059. [DOI] [PubMed] [Google Scholar]