Abstract
Objective: To identify resource use patterns and costs incurred during new episodes of bipolar disorder.
Method: Researchers examined Medstat MarketScan databases covering the interval of January 1, 1998, to December 31, 2002, to identify 6148 patients with new episodes of bipolar disorder as defined by the International Classification of Diseases, Ninth Revision. Resource utilization patterns and costs for the 6 months prior to the index date and for the 30 days and 1 year after the index date were examined. Differences among subcategories of bipolar patients in terms of the resources used before and after the index date were also examined.
Results: The majority of the individuals in the study were female (61.3%) and the mean age was 41.9 years. Patients diagnosed as manic had higher bipolar treatment costs (p < .01) and were more likely to be hospitalized for mental health diagnoses 30 days (p < .01) and 1 year after the index diagnosis (p = .02) compared with individuals diagnosed as depressive, mixed, or other/ unknown. Median total medical costs in the 1 year after the index date were highest for those diagnosed as depressed (p = .02), while patients diagnosed as mixed bipolar had significantly more psychiatrist visits after the index date (p < .01). Approximately 15% of patients were not treated with any central nervous system medication, and over 50% of patients were treated with antidepressants.
Conclusion: The subcategory of bipolar disorder that an individual is diagnosed as having significantly affects resource use and costs after such diagnosis. Patients diagnosed as manic generally used more resources than other individuals. In addition, results suggest that a large proportion of individuals are not being treated in accordance with recommended treatment guidelines.
Bipolar disorder is conservatively estimated to affect approximately 2.6% of the population in the United States,1 and may affect as many as 6.4% if individuals with at least 2 lifetime manic or hypomanic episodes below the threshold for at least 1 week in duration are included.2 The total annual cost of bipolar disorder in the United States has been estimated to be about $45.2 million in 1991 dollars, or about $67.2 million if expressed in 2004 dollars.3 Worldwide, bipolar disorder is the sixth leading cause of disability.4
Patterns of treatment for bipolar disorder are highly complex and varied. Although treatment guidelines have been established,5,6 divergence from these recommendations in usual clinical practice is widespread.7 For example, Lim et al.7 found that only one third of patients who were admitted to psychiatric inpatient units were discharged on medications recommended by expert guidelines as preferred or alternative recommended treatment. Thus, a better understanding of the patterns of treatment received by bipolar patients in usual care is an important initial step in developing interventions to improve the process of care for bipolar disorder.
The objective of this study was to identify patterns of resource use and costs among privately insured patients during new episodes of bipolar disorder. This study used Medstat MarketScan claims data to analyze differences in patterns of resource use and costs across patients grouped by type of index bipolar diagnosis. To the extent possible in claims data, the study team compared the observed patterns of care with treatment guidelines and noted the implications of apparent divergence from treatment guidelines.
PATIENTS AND METHOD
Medstat's MarketScan Commercial Claims and Encounters (CCE) databases provided the data for these analyses. The CCE database is a Health Insurance Portability and Accountability Act (HIPAA)–compliant, fully de-identified medical claims database that includes private sector health data from approximately 100 payers and contains data on clinical utilization, expenditures, and enrollment across inpatient, outpatient, prescription drug, and carve-out services. The database links paid claims and encounter data to detailed patient information across sites and types of providers over time.
The researchers examined MarketScan data over the interval of January 1, 1998, to December 31, 2002, to identify a population of patients with at least 1 claim for bipolar disorder (as defined by International Classification of Diseases, Ninth Revision [ICD-9] codes 296.4x–296.8x). Note that there were no restrictions placed on where the diagnosis of bipolar disorder occurred, so this analysis considers both inpatient and outpatient diagnoses, as well as diagnoses from general practitioners and specialists. From this initial population, the researchers included in the study only those individuals aged 18 through 64 years who had at least 18 months of continuous eligibility and received at least 2 claims with a bipolar diagnosis code on different dates of service during a 365-day period (with first such date identified as the index date). In addition, to examine “new episodes” of bipolar disorder and to increase the homogeneity of the sample, individuals were required to have no previous diagnosis of bipolar disorder or schizophrenia in the 6 months prior to the index date. There were 6194 patients who fit all the above criteria.
In addition, the researchers screened for extreme outliers. Specifically, patients were excluded from the analysis if (1) total medical care costs during the 6 months prior to the index date were greater than $1 million; (2) total inpatient days during the 6 months prior to the index date were greater than 90 days; (3) more than 9 hospitalizations occurred during the 6 months prior to the index date; or (4) total medical costs during the initial 6 months of therapy were greater than $10 million. There were 46 individuals excluded from the analyses using the above criteria, resulting in a final sample of 6148 individuals.
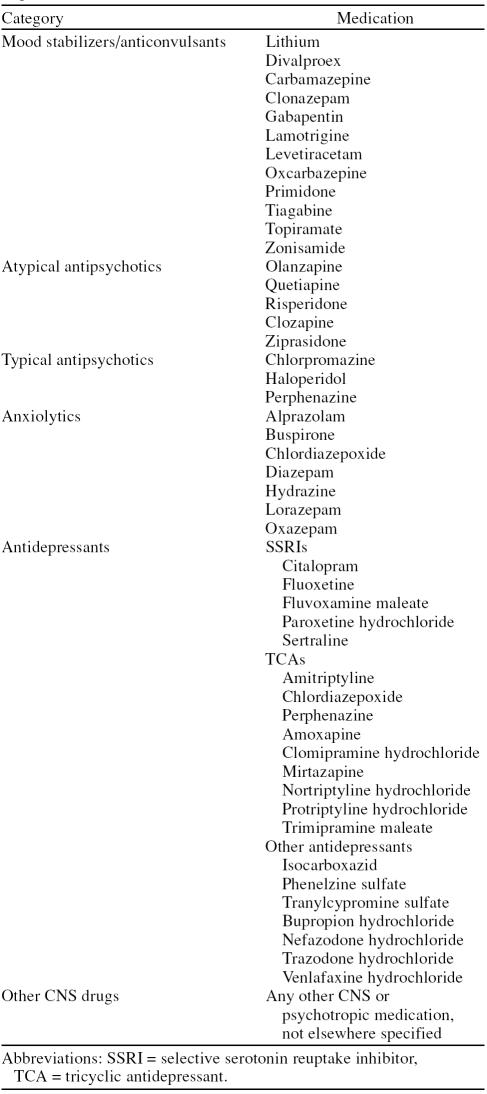
The study team examined medical utilization in the 30 days postdiagnosis, use of inpatient and outpatient services in the 30 days and 1 year postdiagnosis, and medical costs in the 6 months prior to diagnosis and in the 30 days and 1 year postdiagnosis. For medical utilization we examined patient use of mood stabilizers, atypical antipsychotics, typical antipsychotics, anxiolytics, anti-depressants, and other central nervous system (CNS) medications. Table 1 provides a complete list of these CNS medications. Inpatient and outpatient services measured in the analysis include physician visits (primary care and psychiatrist), group therapy sessions, outpatient visits (mental health and all diagnoses), and hospitalizations (for bipolar, mental health, and all diagnoses). Medical care costs consisted of all inpatient, outpatient, emergency room, and prescription drug costs.
Table 1.
Central Nervous System (CNS) Medications Used by Bipolar Disorder Patients
In the descriptive analyses, the researchers grouped patients by type of bipolar disorder at the index diagnosis. The statistical analyses assess differences in sample proportions across groups using χ2 tests, differences in group means for continuous variables using unbalanced analysis of variance, and differences in group medians using the Brown-Mood median test. We considered findings of a p value of ≤ .05 to indicate statistically significant differences between the groups. All analyses were conducted using SAS Version 8.1.8
RESULTS
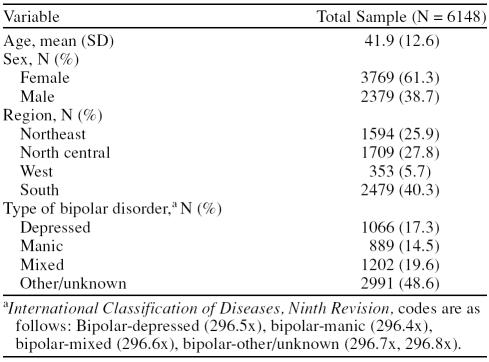
Table 2 reports descriptive sample statistics. The mean age in the sample is 41.9 years, and 61.3% of the sample is female. In terms of geographic representation, the MarketScan overrepresents the southern region of the United States and underrepresents the western region, and our sample is reflective of this fact. The initial type of bipolar diagnosis is other/unknown (as defined by ICD-9 code 296.7x or 296.8x) for almost half of the sample (48.6%). The least common index diagnosis (14.5%) is the manic subtype (ICD-9 code 296.4x).
Table 2.
Demographic Characteristics of Patients With New Episodes of Bipolar Disorder
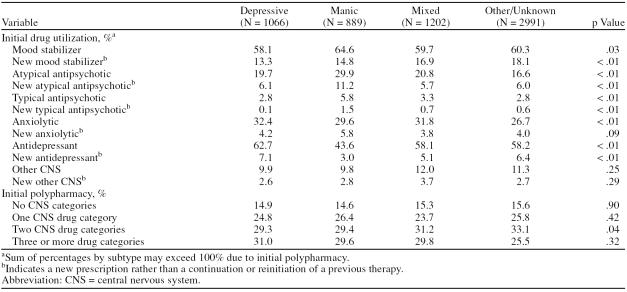
Data on prescription drug use within 30 days of the index diagnosis (Table 3) reveal that, overall, about 15% of all patients did not receive any category of CNS drug, whereas about 60% overall received drugs in 2 or more CNS categories. Most patients used a mood stabilizer within 30 days of diagnosis, with use being most common among patients in the manic subtype (64.6%). While antidepressant use also was common overall, a greater percentage of patients in the depressive subtype (62.7%) used antidepressants compared with 43.6% among patients in the manic subtype. The use of antipsychotics (both typical and atypical) was most common among patients in the manic subtype. Anxiolytics were most commonly used by patients in the depressive and mixed subtypes (32.4% and 31.8%, respectively), but were almost as commonly used by those in the manic and other/ unknown subtypes (29.6% and 26.7%, respectively). However, in most cases, across all of the CNS drug categories examined, drug use during the first 30 days represented the continuation or reinitiation of drug therapy observed during the 6 month preperiod, rather than the initiation of a new drug therapy.
Table 3.
Medication Utilization in the 30 Days Postdiagnosis by Type of Bipolar Disorder
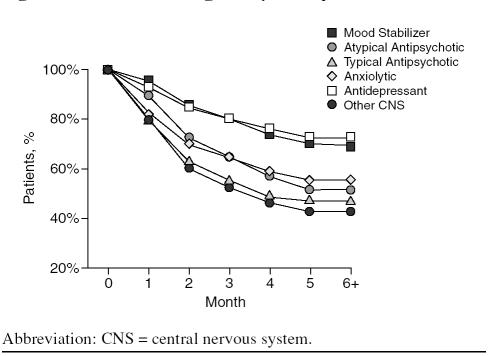
As shown in Figure 1, many patients discontinued the use of prescription drugs over the first 6 months of therapy. Typical antipsychotic and “other CNS” drugs were most likely to be discontinued, whereas antidepressants and mood stabilizers were least likely to be discontinued over this period. Of patients using typical antipsychotics after the index diagnosis, 62.8% continued therapy for more than 60 days, compared with 85.8% for patients using mood stabilizers and 84.4% of patients using anti-depressants. After 6 months, 42.8% of patients using “other CNS” drugs continued to use the drugs, compared with 72.4% of patients using antidepressants and 69.5% of patients using mood stabilizers.
Figure 1.
Duration of Drug Use by Therapeutic Class
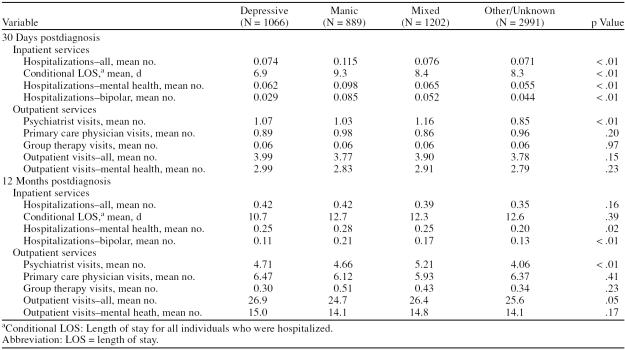
In terms of outpatient and inpatient resource utilization (Table 4), patients with a manic subtype were more likely than patients with other subtypes to be hospitalized for any cause, for any mental health diagnosis, or for bipolar disorder over the first 30 days of therapy. Conditional on having at least 1 hospitalization within the first 30 days, patients with a manic subtype had the longest mean length of stay (9.3 days), and patients with a depressive subtype had the shortest mean length of stay (6.9 days). By contrast, at 1 year following the index diagnosis, the subtypes have the same overall rate of hospitalization and similar rates of hospitalization for general mental health–related conditions (ranging from 0.20 to 0.28); however, at 1 year following the index diagnosis, patients within the manic subtype have a higher rate of hospitalization specifically related to bipolar disorder. In terms of outpatient care, during the first month of therapy, patients initially diagnosed with a mixed subtype had the most frequent psychiatric office visits (mean = 1.16), and patients with other or unspecified subtypes had the least frequent psychiatric office visits (0.85). There were no statistically significant differences across groups in primary care physician visits, group therapy sessions, or outpatient care visits during the first 30 days of therapy. A similar pattern holds for outpatient care during the first year after the index diagnosis.
Table 4.
Inpatient and Outpatient Services by Type of Bipolar Disorder
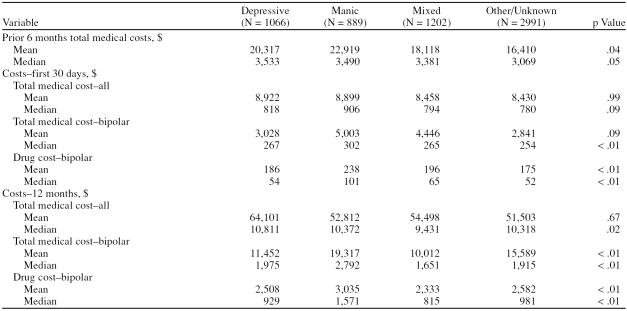
Table 5 summarizes the medical care costs for patients grouped by subtype for the index bipolar diagnosis. During the 6-month period prior to the index diagnosis, patients diagnosed with a manic subtype had the highest mean preperiod medical costs, and patients with an other/ unknown subtype had the lowest mean preperiod costs. The pattern in median preperiod costs is less apparent, though patients with an other/unknown subtype also had the lowest median preperiod costs. Over a 30-day period following the index diagnosis, there were no statistically significant differences in mean or median total medical costs (all diagnoses) across subtypes. However, if only costs directly related to a bipolar diagnosis are considered, there is a statistically significant difference in median costs, with the highest median bipolar costs among patients with a manic subtype ($302) and the lowest median bipolar costs among patients with an other/unknown subtype ($254). There is a trend toward a similar pattern in differences in mean bipolar costs, but the differences are not statistically significant at standard levels (p = .09). Over the first year following the index diagnosis, there were no statistically significant differences in mean total medical costs (all diagnoses) across subtypes, but median total costs were lowest among patients with a mixed subtype ($9431). Data on costs directly related to a bipolar diagnosis over the first year reveal that mean and median bipolar costs were highest among patients in the manic subtype (mean = $19,317; median = $2792) and lowest among patients in the mixed subtype (mean = $10,012; median = $1651).
Table 5.
Medical Costs by Type of Bipolar Disorder
DISCUSSION
As might be expected given the complexity of bipolar disorder, the observed patterns of treatment are highly complex and vary considerably across patients. The use of multiple CNS drug agents is common, visits to both primary care physicians and psychiatrists are frequent, and the risk of hospitalization is significant.
Despite the fact that treatment guidelines recommend drug treatment using 1 or more types of CNS drugs for virtually all forms of bipolar disorder,5 about 15% of the patients in the sample received no CNS drugs within 30 days of the index diagnosis. Given that combination therapy is commonly recommended,5,9–11 it also is interesting that about one quarter of the sample received only 1 type of CNS drug. Obviously, drug treatment might be contraindicated for some patients, or some patients might have refused to initiate the recommended therapy. Nonetheless, this small but not insignificant percentage of patients receiving no drug therapy may be a suitable target for quality improvement initiatives. Furthermore, among individuals who used medication, discontinuation rates in the 6 months after the index date ranged from 5% to 57%.
Treatment guidelines also recommend the use of mood stabilizers for most cases of bipolar disorder,5,9–11 yet only about 65% of patients with a manic subtype received a mood stabilizer, and only about 60% of other patients in the sample received a mood stabilizer.
About 44% of patients with a manic subtype received an antidepressant during the first 30 days following the index diagnosis. About 58% of patients with a mixed subtype received an antidepressant. These high rates of observed antidepressant use predate the publication of the American Psychiatric Association treatment guidelines, which indicate that “antidepressants should be tapered and discontinued if possible.”5(p4) This recommendation was based upon evidence that antidepressants have not been shown to be more effective in preventing depressive relapse than mood stabilizers and are associated with an increased risk of antidepressant-induced mood cycling.12 The high use of antidepressants among these patients prior to the index diagnosis also is likely to reflect the potential for an initial misdiagnosis during an episode of bipolar disorder.
Guidelines also state that psychotherapy may be useful in helping an individual cope with life problems and deal with bipolar disorder.7 In addition, guidelines suggest that psychotherapy may help prevent future manic and depressive episodes by helping to reduce stress and improve medication compliance. However, in the 1 year after the index diagnosis, patients have a higher mean number of primary care physician visits than psychiatrist visits and the mean number of psychiatrist visits is approximately 5. These results suggest that many patients may not be regularly meeting with a psychiatrist.
Taken together, the above results suggest that it is not uncommon for individuals diagnosed with bipolar disorder to not be treated in accordance with recommended treatment guidelines. Since medication not only has a significant impact on quality of life, but also significantly enhances the effectiveness of other treatments, inappropriate use of medication can have serious implications for the patient.13 While treatment guidelines will not fit all individuals, it is important to note that, in general, such guidelines are thought to improve the quality of treatment and increase the accountability of medication treatment.13 Specifically, it has been argued that the advantages of treatment algorithms for the treatment of mental illness include reducing unnecessary variation in clinical practice patterns, making clinical decision explicit, reducing costs, and improving outcomes.13
As to be expected, given the increased resource utilization associated with a diagnosis of bipolar mania or with the use of 2 or more CNS medications before bipolar diagnosis, bipolar manic patients had the highest medical costs. The estimates of bipolar-related medical care costs during 1 year of treatment reported here are substantially greater than the 1-year treatment cost in another recent study using U.S. managed care data.14 From Table 5, the estimated mean bipolar cost for patients with a depressive subtype is $11,452, compared with $5130 in the prior study. Estimates reported in Table 5 for manic and mixed subtypes are $19,317 and $10,012, respectively, compared with $4775 and $3350 in the prior study. In part, these differences might be attributable to the fact that the costs reported in Table 5 focus on new episodes of bipolar disorder, whereas the prior study calculated costs for a prevalent pool of patients with bipolar disorder. Thus, one might expect higher costs during the initial, more acute phase of treatment than in the maintenance phase of therapy.
It is important to note that this analysis examines new episodes of bipolar disorder and not a new onset of the illness. For example, research has shown that the median age at onset for bipolar disorder is 25 years,15 while the mean age of individuals in this study is 42. The results presented here may not be typical of individuals with new onset of bipolar disorders.
The findings of this study should be interpreted in the context of the limitations of the study design. For inclusion in this study, individuals had to have been continuously insured for at least 18 months and have no bipolar diagnosis in the 6 months prior to index date. As such, results from this study may not be generalizable to other populations. Second, the use of diagnostic codes to identify individuals with bipolar disorder is not as rigorous as formal diagnostic assessments. In addition, use of a diagnosis of bipolar disorder with no prior diagnosis in the prior 6 months may not accurately reflect a new episode of bipolar disorder. However, it should be noted that similar types of criteria have been used in other studies that examine mental illness in a retrospective claims database.16–18 Third, the analysis depends upon prescriptions filled to examine medication use. However, such data may not reflect actual prescriptions issued. Fourth, the use of medical claims data records precludes the inclusion of potentially important factors for consideration, such as the individual's age at onset or substance and/or alcohol abuse. Fifth, the exclusion of very high cost outliers is likely to result in conservative mean costs estimates, but the resulting estimates may be more generalizable. Finally, it is important to note that the analysis focuses on resource utilization and direct medical costs for individuals diagnosed with bipolar disorder, and hence does not include other costs associated with bipolar disorder, such as morbidity, mortality, unemployment, or incarceration.
CONCLUSION
Although treatment for bipolar disorder is highly complex and varied, some patterns emerge as we examine mental health diagnoses, treatments, hospitalization rates, and costs in the periods immediately preceding and following the bipolar diagnosis. Specifically, a patient's existing mental health diagnosis and his or her use of CNS medications before beginning treatment for bipolar disorder significantly affect resource use and costs after beginning treatment. Patients diagnosed as manic and those who received more than 2 CNS medications prior to their bipolar diagnosis generally used more resources than other individuals. As a result, extra effort in early diagnosis of bipolar disorder and treatment options that improve outcomes for bipolar mania could have large implications for those who bear the burdens—in terms of costs, resources, and quality of life—for bipolar disorder.
Drug names: alprazolam (Xanax, Niravam, and others), bupropion (Wellbutrin, Zyban, and others), buspirone (BuSpar and others), carbamazepine (Carbatrol, Equetro, and others), chlordiazepoxide (Librium and others), chlorpromazine (Thorazine, Sonazine, and others), citalopram (Celexa and others), clomipramine (Anafranil and others), clonazepam (Klonopin and others), clozapine (FazaClo, Clozaril, and others), diazepam (Diastat, Valium, and others), divalproex (Depakote), fluoxetine (Prozac, Sarafem, and others), gabapentin (Neurontin and others), haloperidol (Haldol and others), isocarboxazid (Marplan), lamotrigine (Lamictal and others), levetirac-etam (Keppra), lithium (Eskalith, Lithobid, and others), lorazepam (Ativan and others), mirtazapine (Remeron and others), nortriptyline (Pamelor and others), olanzapine (Zyprexa), oxcarbazepine (Trileptal), paroxetine (Paxil, Pexeva, and others), phenelzine (Nardil), primidone (Mysoline and others), protriptyline (Vivactil), quetiapine (Seroquel), risperidone (Risperdal), sertraline (Zoloft and others), tiagabine (Gabitril), topiramate (Topamax and others), tranylcypromine (Parnate and others), trimipramine (Surmontil and others), venlafaxine (Effexor and others), ziprasidone (Geodon), zonisamide (Zonegran and others).
Footnotes
This research was supported by AstraZeneca, Wilmington, Del. Dr. Ohsfeldt is a consultant for Auger and Pfizer and has received grant/research support from AstraZeneca. Dr. Lage is a consultant for AstraZeneca, Johnson and Johnson, Amgen, and Eli Lilly. Dr. Rajagopalan has no additional financial or other relationships relevant to the subject of this article.
REFERENCES CITED
- Kessler RC, Chiu WT, and Demier O. et al. Prevalence, severity, and comorbidity of twelve-month DSM-IV disorders in the National Comorbidity Survey Replication (NCS-R). Arch Gen Psychiatry. 2005 62:617–627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Judd LL, Akiskal HS.. The prevalence and disability of bipolar spectrum disorders in the US population: re-analysis of the ECA database taking into account subthreshold cases. J Affect Disord. 2003;73:123–131. doi: 10.1016/s0165-0327(02)00332-4. [DOI] [PubMed] [Google Scholar]
- Kleinman L, Lowin A, and Flood E. et al. Costs of bipolar disorder. Pharmacoeconomics. 2003 21:601–622. [DOI] [PubMed] [Google Scholar]
- Woods SW. The economic burden of bipolar disease. J Clin Psychiatry. 2000 61suppl 13. 38–41. [PubMed] [Google Scholar]
- American Psychiatric Association. Part A: treatment recommendations for patients with bipolar disorder. Am J Psychiatry. 2002 159suppl 4. 4–15. [PubMed] [Google Scholar]
- Keck PE Jr, Perlis RH, and Otto MW. et al. The expert consensus guideline series: treatment of bipolar disorder 2004. Postgrad Med Special Report. December2004 1–120. [Google Scholar]
- Lim PZ, Tunis SL, and Edell WS. et al. Medication prescribing patterns for patients with bipolar I disorder in hospital settings: adherence to published practice guidelines. Bipolar Disord. 2001 3:165–173. [PubMed] [Google Scholar]
- SAS User's Guide. SAS/STAT User's Guide: Version 8. Cary, NC: SAS Institute. 1999 [Google Scholar]
- Suppes T, Dennehy EB, and Swann AC. et al. Report of the Texas Consensus Conference Panel on Medication Treatment of Bipolar Disorder 2000. J Clin Psychiatry. 2002 63:288–299. [DOI] [PubMed] [Google Scholar]
- The World Federation of Societies of Biological Psychiatry (WFSBP) Guidelines for the biological treatment of bipolar disorders, pt 1: treatment of bipolar depression. World J Biol Psychiatry. 2002;3:115–124. doi: 10.3109/15622970209150612. [DOI] [PubMed] [Google Scholar]
- The World Federation of Societies of Biological Psychiatry (WFSBP) Guidelines for the biological treatment of bipolar disorders, pt 2: treatment of mania. World J Biol Psychiatry. 2003;4:5–13. doi: 10.3109/15622970309167904. [DOI] [PubMed] [Google Scholar]
- Ghaemi SN, Hsu DJ, and Soldani F. et al. Antidepressants in bipolar disorder: the case for caution. Bipolar Disord. 2003 5:421–433. [DOI] [PubMed] [Google Scholar]
- Algorithms and the medication treatment of people with serious mental illnesses. [National Association of State Mental Health Program Directors Web site]. Dec 1997. Available at: http://www.nasmhpd.org/general_files/publications/med_directors_pubs/meddir2.htm. Accessed Aug 2006. [Google Scholar]
- Bryant-Comstock L, Stender M, Devercelli G.. Health care utilization and costs among privately insured patients with bipolar I disorder. Bipolar Disord. 2002;4:398–405. doi: 10.1034/j.1399-5618.2002.01148.x. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, and Demler O. et al. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005 62:593–602. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Practice guidelines for major depressive disorder in adults. Am J Psychiatry. 1993;150:1–26. doi: 10.1176/ajp.150.4.1. [DOI] [PubMed] [Google Scholar]
- Birnbaum HG, Cremieux PY, and Greenberg PE. et al. Management of major depression in the workplace. Dis Manage Health Outcomes. 2002 7:163–171. [Google Scholar]
- Marciniak MD, Lage MJ, and Dunayevich E. et al. The cost of treating anxiety: the medical and demographic correlates that impact total medical costs. Depress Anxiety. 2005 21:178–184. [DOI] [PubMed] [Google Scholar]