Dr. Otto: There have been a number of population-based studies on the association between exercise and mental health. What is generally found in these large-scale studies?
Dr. Church: These population-based studies vary in size, population, and the way they assess physical activity and fitness. In general, the data1 indicate that people who participate in regular physical activity are less likely to either have depression or develop depression in the future.
Dr. Otto: It could be that individuals with disorders do not feel like exercising. Do you have a sense that causation is driven in both directions or in one direction in particular?
Dr. Church: When it comes to epidemiologic studies of depression and exercise, one can rarely claim causation. Depressed patients may be disinclined to exercise,2 a fact that makes causation even more difficult to determine. In depressed individuals, an internal bias concerning exercise often exists, which is precisely why it is important to have clinical trials with rigorous methodology.
Dr. Trivedi: An interesting clinical aspect of exercise and depression studies is that some of the studies3–5 that have examined population-based data have not evaluated depression as a diagnosis or as a disorder. Most of the studies6,7 have evaluated symptoms of depression that include not only major depression, but mood disorders other than major depression. The data from these studies4–7 suggest that patients who are physically active have psychological well-being in addition to physical well-being. Whether or not the results of these large-scale population studies are related to depressive disorders remains unclear. Few prospective studies have been conducted to answer this question.
Dr. Otto: This lack of clarity in the epidemiologic studies introduces the idea that exercise may promote general well-being, but once well-being is lost, individuals may find maintaining exercise difficult.
THE ANTIDEPRESSANT EFFECTS OF EXERCISE AS APPLIED TO PARTICULAR PATIENT SUBTYPES
Dr. Trivedi: The relationship between exercise and depression is pivotal. This relationship must be considered when using exercise for the treatment of depression or other mood or anxiety disorders.
Dr. Otto: As compared to epidemiologic studies, clinical trials examining the relationship between exercise and depression move clinicians and researchers closer to understanding the efficacy of exercise as a bona fide treatment of depression.
Dr. Trivedi: Blumenthal et al.8 examined pharmaco-therapy in combination with exercise, but only in the elderly. In this study, patients (N = 156) who exercised did so in a group setting, which raises a possible methodological issue in that some of the effect that was seen could have been the result of socialization. An important line of future research in this area is the development of well-controlled clinical trials to compare the efficacy of exercise to well-established treatments for depression.
Dr. Otto: Dr. Smits and Dr. Craft have each been involved in separate meta-analyses1–9 of the literature on the relationship between exercise and depression. How effective is exercise as a treatment for depression and to which patient subtypes has exercise been applied?
Dr. Smits: My colleagues and I recently completed a meta-analysis1 that examined 11 studies with patients diagnosed with major depression and who were prescribed exercise or a nonactive comparator. Most of the patients included in the meta-analysis had moderate depression. The data from the meta-analysis show promise for the effectiveness of exercise for the treatment of depression, in 2 to 4 exercise sessions per week for 12 weeks. The individuals in the studies made significant improvements, for an effect size of 1.42 (95% CI = 0.92 to 1.93) versus control. The studies included in the meta-analysis had average attrition rates of 19.9%, rates that are comparable to attrition rates found in antidepressant trials, cognitive-behavioral therapy trials, and interpersonal therapy trials.8
Dr. Craft: In 1998, I conducted a meta-analysis with Daniel M. Landers9 and found that the majority of studies supported the efficacy of exercise as an antidepressant. Our examination of different potential moderator variables, including subject characteristics such as age, gender, and severity of depression and exercise characteristics such as intensity, duration, and frequency of exercise, showed that very few variables other than the length of the exercise program impact the relationship between exercise and depression. Exercise is effective for many different patient subtypes across genders and ages, regardless of the severity of depression.
Dr. Otto: The strength of the effect sizes in these meta-analyses1,9 is surprising. Why has the effectiveness of exercise not been featured in psychological and psychiatric literature until recently?
Dr. Craft: The early literature was positive for exercise as a treatment for depression, but it suffered from a variety of methodological flaws10 and may have dampened clinicians' enthusiasm toward implementing exercise programs in their practices. Recent controlled clinical trials11–14 examining the relationship between depression and exercise have surprised many clinicians by showing how effective exercise is, but exercise has not yet been implemented in the treatment plans of most clinicians. Implementation should be the primary goal.
HOW DO EXERCISE INTERVENTIONS COMPARE TO OTHER TREATMENTS FOR DEPRESSION?
Dr. Otto: A common question posed clinicians is how well exercise works in the treatment of depression relative to psychosocial treatments and pharmacotherapy. What is the evidence for exercise as a treatment for depression?
The methodology of studies on exercise has improved over time: the studies have been controlled better and the populations have been larger. In other meta-analyses, the effect size seemed to taper off as larger, better-controlled trials were conducted. In contrast, studies8,11–13,15,16 of exercise and depression, continue to show strong efficacy findings over time.
Dr. Craft: While there have been very few studies that directly examined pharmacotherapy in combination with exercise, data subsets in these studies can be used to compare treatment with pharmacotherapy alone to treatment with pharmacotherapy in combination with exercise. Even if the subset comparisons were not present in the primary research studies, the studies so far show that exercise for depression compares favorably with traditional treatments for depression.9,17
Dr. Trivedi: Some of the meta-analyses1,9 performed on exercise and depression have included data from small studies, raising concerns about their reliability and hence their full relevance to the armamentarium for treatment.
EXERCISE AS A TREATMENT IN CLINICAL PRACTICE
Dr. Trivedi: My colleagues and I have published a study that may answer the question raised earlier: how do clinicians use exercise to treat patients in their practices? In our study,11 we compared different doses of exercise to a control condition, which was a stretching exercise program. Stretching exercises worked as a control for high-impact exercises, because, although stretching increases flexibility, it does not elevate the heart rate or require the same amount of caloric energy as high-impact cardiovascular exercises. High-dose exercise was more effective in treating depression compared with stretching, but low-dose exercise did not produce the desired benefits.
We found no noticable difference in results between physical activity spread over 3 days and physical activity spread over 5 days. (Table 1). Some patients have asked if they could receive their entire dose of exercise all in 1 day, but 1 day of exercise may not be possible or desirable for most patients. Spreading the exercise dose over 3 to 5 days puts less stress on the patient's body and helps integrate the exercise routine into the patient's schedule.
Table 1.
Response and Remission Rates in 12-Week Trial of Exercise as Augmentation of Pharmacologic Antidepressantsa
Exercise should also be considered as an augmentation to standard pharmacotherapy. Remission rates with selective serotonin reuptake inhibitors and other commonly used antidepressants are approximately 30%,14 which means there is a large percentage of patients with depression for whom antidepressant pharmacotherapy is not enough. For these patients, adding exercise to pharmaco-therapy or vice versa, or starting both in combination are worthwhile clinical approaches.18
Dr. Otto: Dr. Trivedi, do the patients in your clinic in the exercise trial share similar characteristics with the patients treated with traditional pharmacotherapy?
Dr. Trivedi: My colleagues at the clinic and I have not directly compared the patient samples for the 2 treatments, but the patients' sociodemographic characteristics, clinical illness characteristics, and symptom profiles seem comparable. There may be some differences between the groups; for example, the patients who come in for exercise studies may have a slightly higher socioeconomic standing and may be more educated about the relationship between exercise and depression. Patients like these may enter the study with an expectation that exercise is likely to benefit them. This sample variation is not that different from sample variations that occur in other nonpharmacologic psychotherapy studies. Patients who participate in psychotherapy are generally similar to those in pharmacotherapy studies, but the psychotherapy patients may be better educated about the potential benefits of psychotherapy.
Dr. Otto: So, at your clinic, Dr. Trivedi, patients make a choice to receive psychotherapy, pharmacotherapy, or exercise before they participate in the study?
Dr. Trivedi: Patient preference is becoming an important variable in the choice of antidepressant in practice. In the Sequenced Treatment Alternatives to Relieve Depression (STAR*D) results that my colleagues and I published recently,19 at the second and third steps of the algorithm, patients often exhibited a strong preference as to whether to switch treatments or to augment antidepressant treatment after the first treatment failed. If patient preference is introduced as a key variable in deciding treatment method, treatment may be more effective.
Dr. Craft: Individuals who are willing to participate in trials of exercise as a treatment for depression are at least interested in exercise, which may be different from the attitude of the average person who seeks treatment for depression. In ongoing research, I have found that minority individuals, who have not historically been included in some studies on exercise and depression, are highly interested in exercise as an option for treatment of depression. This trend seems particularly true of minority individuals who are not interested in or who wish to augment traditional pharmacologic treatments.
Research20–25 shows that despite the fact that depression rates among minority women are quite similar to the rates among their Caucasian peers, minority women are less likely to take antidepressants or receive specialty care. Therefore, it is important that we identify efficacious treatments for depressed minority women, who often do not fully embrace or have access to traditional therapies.26 The majority of studies examining the use of exercise to reduce symptoms of depression have been conducted on Caucasian samples. Consequently, a primary gap in this literature centers on how well these findings generalize to depressed women of diverse racial and ethnic backgrounds. While exercise may be just as effective for minority women as Caucasian women, research is needed to verify that assumption.
In a recently completed randomized clinical trial (L.L.C.; K. M. Freund, M.D.; L. Culpepper, M.D., M.P.H.; et al., unpublished data, 2006), we enrolled 32 depressed sedentary women and randomly assigned them to either a facility-based or home-based exercise intervention. Just over 80% of the women enrolled were minority (African-American and Latina) and about half were not receiving any treatment for their depression at study entry. By 6-month follow-up, women in both groups had significantly increased (p < .05) time spent in physical activity. Further, both groups also experienced significant reductions (p < .05) in depression. Study results support the efficacy of exercise to reduce depression among minority women, and researchers should continue to investigate the use of exercise as an adjunct treatment in this subset of patients. However, this is the first study to examine the exercise-depression relationship utilizing a predominantly minority sample and results need replication.
Dr. Greer: Not only are minority individuals interested in exercise for the treatment of their depression, but they want to exercise to improve their global health as well. For example, the prevalence of diabetes, which is frequently comorbid with depression is increased in some minority groups.27 With increasing efforts to raise public awareness of the health benefits of exercise, individuals of all racial and ethnic groups are beginning to desire physical activity to benefit both mental and physical health. We have found that the interest in our exercise studies has been very high, and patients seem to be increasingly aware of the overall health benefits of exercise, in addition to their hope of relief from depressive symptoms.
Global Health Benefits of Exercise: Treating the Whole Patient
Dr. Otto: We should discuss the additional health benefits of exercise further. Aside from mental health benefits, what are some of the other health benefits associated with exercise?
Dr. Church: Exercise is extremely powerful in fighting cardiovascular disease.28,29 Physical activity reduces the risk of heart attack and stroke,30 which is particularly important for individuals who have hypertension, diabetes, or cholesterol abnormalities. Physical activity also reduces the risk of developing certain cancers, such as colon cancer31 and breast cancer.32 Also, if aging people are physically active, their overall quality of health and quality of life are improved.
Traditional risk factors do not explain the benefits of exercise in treating cardiovascular disease. There are some hypotheses as to why exercise is powerful in the prevention and reoccurrence of cancer, but there are no concrete answers. The current inability to discover the exact mechanism by which exercise helps with mood disorders should not be a concern. If the history of cancer research and cardiovascular disease has given us a research paradigm, it could be decades before we understand why physical activity works for mental health.
Dr. Greer: Depression itself is an independent risk factor for cardiovascular disease. Cardiovascular disease is a common, chronic physical disease that is often comorbid with depression. Individuals who have had cardiac events and who also have depression exhibit poorer outcomes than individuals without comorbid depression.33,34 Increasing a depressed patient's physical activity is an outstanding opportunity to use exercise as a treatment for mental health and to possibly garner some physical health benefits as well.
Health Risks of Exercise Prescription
Dr. Otto: With all of the positive effects already discussed, possible adverse effects also need to be discussed. What particular health risks should be attended to when making the decision to prescribe an exercise program?
Dr. Church: The risks are relatively minimal if the individual understands the importance of starting slowly and building up the activity over time. The people who typically experience adverse effects are males in their 40s who try to perform the same workout they performed in high school. The goal of treatment should be physical activity, not necessarily buying a pair of running shoes and joining a gym, although joining a gym does motivate some patients.
Before initial treatment, the clinician should identify high-risk individuals, such as patients with histories of stroke, heart attack, or diabetes. These patients should be medically cleared before beginning physical activity. For the vast majority of people, the risk of sudden cardiac events is minimal, as long as they start at a realistic pace. For example, a walking program at light to moderate intensity is safe for most people. Intensity can be increased over time, and the patient should pay attention to symptoms such as chest pain or shortness of breath. Common problems patients face when beginning exercise are bone and joint issues, such as sore knees and ankles, and more chronic problems, such as old injuries that are developing into arthritis. If a patient starts an exercise program slowly, joint stiffness, soreness, and pain can be minimized.
Dr. Otto: A key idea in using exercise as a treatment for depression is that of building up intensity over time. How can a clinician convince a patient who has not recently participated in regular physical activity to start an exercise program and adhere to it?
Dr. Greer: One recommendation is to have patients who are interested in exercise record the frequency, the duration, and the modality of each exercise session and then solve any issues that arise from integrating an exercise regimen into everyday life. A sample exercise log that includes many of the desired data to be recorded is available in our recent pilot study of exercise augmentation.2
Dr. Craft: Research shows that self-monitoring exercise behavior and addressing key psychosocial issues, such as barriers to exercise, exercise self-efficacy, and social support for exercise, as well as providing brief and supportive follow-up contact, can improve exercise adherence by up to 25% in the general population.13
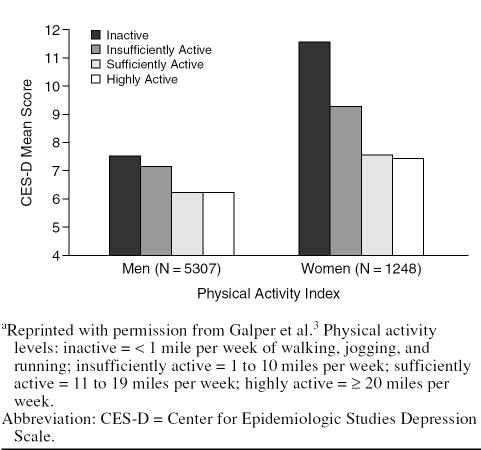
Although studies3,12 have found a greater reduction in depression with a greater intensity of exercise, it is important to keep in mind that exercise does not have to be lengthy or intense for an individual to benefit (Figure 1).
Figure 1.
Physical Activity Reduces Depression Scores on the CES-Da
Dr. Church: A useful tool for self-monitoring and for incorporating physical activity into individuals' daily lives is the step counter, which is a device that clips on to the belt and shakes with every step. It supplies readouts of how many steps are taken during the day. The step counter is inexpensive, easy to use, and provides a simple way to quantify daily physical activity. They can be bought for around $20 at most sporting goods stores.
Activity: The Proper Dose
Dr. Otto: Many clinicians may have heard in media reports that a proper dose of activity is 10,000 steps per day. Is 10,000 steps the range that we are recommending to clinicians in practice?
Dr. Church: The round number “10,000 steps” sounds scientific in the media, but there is little research to support that number. People with step counters should wear the counter for a few days to find the average number of steps they take each day. A sedentary American will average between 3000 and 5000 steps.35 Once people know their average, they should add 1000 to 2000 steps per week. For sedentary people, a realistic goal is approximately 8000 steps per day. For those who want to be more active, the goal may be closer to 10,000 steps per day. Finally, for people truly interested in losing weight and seeing physiologic changes, the number of steps desired may be greater than 10,000.
Dr. Craft: From a research perspective, a goal of 10,000 steps a day is unrealistic for most individuals with depression. Depressed people tend to be sedentary, be overweight, and have reduced work capacities.17 In my experience, the baseline number of steps for individuals with depression tends to be a range of 2000 to 3000 steps per day. The number popular in the media, 10,000 steps, equals about 5 miles per day. Walking 5 miles per day is an unrealistic goal for a sedentary, depressed person. Find the individual's baseline and then gradually add steps.
Dr. Otto: What sort of dose and duration should be suggested for the average depressed patient?
Dr. Church: The general consensus for treatment is about 30 minutes of physical activity a day, at least 5 days a week.15,18 I recommend that physical activity be performed once every 3 days.
Dr. Otto: Exercise 3 to 5 days a week seems to be the most effective dose. How long does it take for the average patient to see benefits from exercise? When do patients tend to report feeling better?
Dr. Craft: In the study I published in 2005,15 depressive symptoms were evaluated at baseline, at week 3, and at week 9. By week 3, individuals who exercised (N = 9) had reduced their mean scores on the Beck Depression Inventory-II scale from 21.2 to 9.3, while the mean scores of the control individuals (N = 10) remained approximately the same (with significant differences between these groups).
Clinicians should emphasize to patients the short-term benefits of exercise: improvements in mood, energy level, the ability to concentrate and focus, and quality of sleep. Many individuals are focused on the distant outcomes, such as weight loss, so emphasizing short-term benefits can help patients adhere to a new exercise regimen.
While 150 minutes of physical activity per week is the ultimate goal of treatment, for depressed individuals, 3 to 5 periods of exercise a week for 30 minutes per period is overwhelming at first. When starting a depressed individual on an exercise program, a reasonable and attainable goal can be as minimal as 10, 15, or 20 minutes of physical activity at a time. A good tool in the beginning is to reinforce frequency so that physical activity becomes habitual. The clinician can then work with the patient to increase the duration of the activity, and later work on building the intensity of the activity.15
EXERCISE ALSO BENEFITS PATIENTS WITH ANXIETY DISORDERS
Dr. Otto: Is there literature that shows that physical activity can provide benefits for patients with disorders other than depression, for example, anxiety?
Dr. Smits: The qualitative review1 that my colleagues and I performed found that not much work has been done on the use of exercise as a treatment for other mental disorders. We found a few randomized, controlled trials on alcohol abuse,36 eating disorders,37–39 and anxiety disorders.40 The literature shows some promise for exercise as a treatment for anxiety disorders and for panic disorder40 in particular.
The exercise model for panic disorder is different from the exercise model for depression. Physical activity may serve as exposure treatment for panic disorder. Exercise may create physical sensations that produce fear in people with panic disorder. The activity may provide necessary exposure to these sensations so that patients with panic disorder can begin to recover.41 Preliminary work40 on the relationship between exercise and panic disorder showed that exercise outperformed placebo in the reduction of panic disorder symptoms, and approached the level of benefit offered by clomipramine.
Dr. Otto: The side effects from exercise such as sweating, light-headedness, and rapid heartbeat are useful tools for treating panic disorder. Clearly, clinicians should not fear comorbid disorders when treating patients with exercise.
THE WELL-BEING EFFECT ACROSS MULTIPLE SYMPTOM DOMAINS
Dr. Otto: Exercise has been discussed as having far-reaching effects, including improving resiliency to stress and treating panic disorder. Are the same effects seen in clinical applications or, since exercise trials for depression are more prominent than exercise trials for other mood disorders, are researchers in those trials commenting on broad-based changes? Has an effect on well-being been observed across multiple symptom domains, either in trials or in clinical practice?
Dr. Greer: Our work in this area suggests that in addition to reductions in depressive symptom severity, exercise augmentation produces psychosocial benefits and improved quality of life. Participants who received 12 weeks of exercise augmentation showed a mean increase of 14 points on the Quality of Life Enjoyment and Satisfaction Questionnaire (short form, general activities).2
Dr. Craft: In my current clinical trial work, patients tend to readily report reduction in depression and those patients who have an anxiety component to their depression often say that their feelings of anxiety diminish as well when they exercise regularly. In patients who exercise, an overall sense of well-being is enhanced.
Dr. Otto: Why does exercise lead to these improvements? Dr. Smits has already mentioned that the mechanism of action for exercise in the treatment of panic disorder may be different from the mechanism of action in depression. What does the literature show about the mechanism of action in depression?
Dr. Greer: Animal studies42–44 have observed increases in neuromodulators, like serotonin and norepinephrine, when the animals exercised. The increased production of neuromodulators caused by exercise is consistent with the target of antidepressant pharmacotherapy. Exercise is likely to play an important role in mood elevation.
Dr. Otto: In effect, exercise produces the same neuro-chemical changes that are often targeted by pharmaco-therapy.
Dr. Trivedi: In addition to the neurochemical changes, inherent in exercise is the attainment of self-efficacy. Patients play a large part in the successful achievement of the correct dose of treatment.12 Self-efficacy, the belief that one has the ability to produce a desired effect, may enhance the antidepressant effect and may even be the cause of the neurochemical changes.
Dr. Otto: Activity assignments alone are effective for the treatment of depression. Simply initiating physical activity in a goal-driven way may relieve depression. Could a simple increase in activity level relate to self-efficacy?
Dr. Trivedi: In studies,45,46 self-efficacy has been shown to have some antidepressant effect. A randomized trial could confirm whether self-efficacy is an additional benefit of exercise or not.
Dr. Smits: Changing patients' action tendencies, getting people to take action that is inconsistent with how they feel, is a common theme of psychotherapy for depression and anxiety disorders and may improve patients' moods.
Dr. Otto: The proposed mechanisms of action for anti-depressant agents have changed over the years as researchers learned more about the brain. A treatment may be known to be effective for many years without us knowing the mechanism of action.
Dr. Church: Lack of a mechanism of action is part of the reason physical activity has not gained acceptance in the mental health arena.
CLINICAL TOOLS FOR EXERCISE MAINTENANCE
Dr. Trivedi: The effectiveness of exercise as a treatment for depression is gaining recognition. Interest in exercise, especially as an augmentation to pharmacotherapy, is increasing. Exercise needs to become an accepted treatment option.
Once the patient has accepted physical activity as a treatment option, the challenge for the physician is to help each patient find the right dose of exercise and maintain it. This question of dose and maintenance has not been well studied. In our studies,2,3,11,12 my colleagues and I have focused on trying to make sure that the patients followed through with the prescribed dose of exercise. The clinical challenge will be to find strategies that ensure patients continue to exercise after the first several weeks, when their motivation declines.
Dr. Church: Maintenance of physical activity is a challenge, but ongoing research may soon give clinicians scientifically proven tools to encourage maintenance of activity. Clinicians should emphasize the incorporation of regular physical activity, not just vigorous activity, into daily life.
Dr. Craft: In clinical work, I have found that once patients begin to feel better as a result of exercise, they are eager to continue their exercise if the clinician can help them attribute their improved mood to the exercise regimen. Improved mood as a result of increased physical activity may be obvious to the researcher or clinician, but the connection is not always obvious to the patient.
Dr. Smits: Reinforcing the connection between mood change and exercise is particularly relevant for patients with panic disorder. The prescription for exercise for panic disorder requires patients to engage in intense exercise in order to elevate their heart rates so that they can become accustomed to sensations that will help them overcome their fear of panic.
If patients do not have a sense of how exercise is going to work to treat their disorder, or if patients fail to see improvement after the first few sessions, then it will be exceedingly difficult to maintain the program. Giving patients a model of exercise as treatment before beginning therapy and reminding patients to maintain their exercise program once they have started are important in treating patients with panic disorder effectively.
Dr. Otto: Clinicians already have a variety of skills relevant for enhancing adherence to exercise. Psychosocial therapists and cognitive-behavioral therapists have developed strategies introducing and maintaining behavior change. Likewise, psychopharmacologists have strategies to introduce patients to medication treatment: developing the routine of taking a pill daily and maintaining the use of the medication for long-term treatment. Clinicians can apply related strategies for promoting adherence to this new intervention, exercise.
Dr. Craft: Many of the strategies used with cognitive-behavioral therapy could easily be applied to exercise: self-monitoring, goal-setting, homework activities, and supportive follow-up. All of these strategies will help maintain the new behavior.
Dr. Otto: What advice would you give a clinician who wants to add exercise as an adjunctive treatment for depression? What is a good way to start a patient with a prescription for exercise?
Dr. Trivedi: My colleagues and I18 recently discussed some tools that clinicians can use to implement exercise as a treatment augmentation. The most important part of beginning exercise treatment is to motivate patients. Motivation ensures adherence to the treatment, just as a patient treated with pharmacologic agents is motivated to take his or her medication on the prescribed basis. Patients may need to be educated about the fact that exercise effectiveness truly depends on dose, and if a patient does not receive the right dose of exercise, the patient will not attain the desired benefits.
In our article,18 we provided a sample dose calculation by weight, which allows patients to recognize how many hours per week they need to spend walking, jogging, or participating in other physical activities (Table 2). Applicable and practical pointers for clinicians are included in the article.
Table 2.
Sample Exercise Dose Calculationsa
Dr. Otto: Patients have some leeway in working up to the exercise dose. What matters is not that the patient achieves the goal right away, but that the individual reaches the optimum dose over time.
NEW RESEARCH FOR EXERCISE AND CLINICAL PRACTICE
Dr. Otto: What do you see in the near future for exercise research and practice?
Dr. Church: Using neuroimaging, researchers are comparing the neurologic changes associated with pharmacotherapy in people who are depressed with the neurologic changes in people who have used exercise as an antidepressant. The results can be viewed using neuro-imaging.
Dr. Trivedi: In practice, although exercise may be helpful as a single agent, most clinicians are likely to use exercise as an augmentation agent for partial responders or as an adjunct for patients who have very specific residual symptoms. Partial responders are the ideal patient sample to which physicians and clinicians will prescribe goal-directed exercise interventions. Once goal-directed exercise interventions are a practice that clinicians can readily implement, as Dr. Church suggested, goal-directed exercise may become commonly used in clinical care.
Drug name: clomipramine (Anafranil and others).
Disclosure of off-label usage: The chair has determined that, to the best of his knowledge, clomipramine is not approved by the U.S. Food and Drug Administration for the treatment of panic disorder.
Affiliations: From the Department of Clinical Psychology, Boston University, Boston, Mass. (Dr. Otto); The Cooper Institute, Dallas, Tex. (Dr. Church); Feinberg School of Medicine, Northwestern University, Chicago, Ill. (Dr. Craft); the Department of Psychiatry, University of Texas Southwestern Medical Center, Dallas (Drs. Greer and Trivedi); the Department of Psychology, Southern Methodist University, Dallas, Tex. (Dr. Smits).
Faculty disclosure: In the spirit of full disclosure and in compliance with all ACCME Essential Areas and Policies, the faculty for this CME article were asked to complete a statement regarding all relevant financial relationships between themselves or their spouse/partner and any commercial interest (i.e., a proprietary entity producing health care goods or services) occurring within the 12 months prior to joining this activity. The CME Institute has resolved any conflicts of interest that were identified. The disclosures are as follows: Dr. Otto is a consultant for Organon and is a member of the speakers or advisory boards for Sanofi-Aventis. Dr. Trivedi is a consultant for or member of the speakers bureaus for Akzo (Organon), Bristol-Myers Squibb, Cyberonics, Eli Lilly, Forest, Janssen, Johnson & Johnson, Organon, Pfizer, Pharmacia, Sepracor, Solvay, and Wyeth and has received grant/research support from Abbott, Akzo (Organon), Bayer, Bristol-Myers Squibb, Cephalon, Corcept Therapeutics, Cyberonics, Eli Lilly, Forest, GlaxoSmithKline, Janssen, Johnson & Johnson, Mead Johnson, Merck, the National Alliance for Research on Schizophrenia and Depression, the National Institute of Mental Health, Novartis, Parke-Davis, Pfizer, Pharmacia, Predix, Solvay, and Wyeth. Drs. Church, Craft, Greer, and Smits have no personal affiliations or financial relationships with any proprietary entity producing health care goods or services consumed by, or used on, patients to disclose relative to the Commentary.
Footnotes
In this month's commentary, which also appears in the May 2007 issue of The Journal of Clinical Psychiatry (2007;68:669–676), 5 experts on exercise and psychiatric disorders discuss the rationale and evidence for using exercise to treat mood and anxiety disorders. This commentary covers a topic that is particularly relevant to primary care physicians, who are increasingly called upon to meet the mental as well as physical health care needs of patients. –Larry Culpepper, M.D., M.P.H.
Physicians discuss practical strategies for clinicians inspired to implement exercise as a prescribed treatment for patients with mood and anxiety disorders.
Exercise is not only beneficial for overall health and well-being, but is proving to be highly effective in the treatment of depression, anxiety, and other psychiatric disorders. Past methodological problems with the examination of exercise efficacy in treating depression, such as not distinguishing between depressed mood and depressive disorders, have helped temper the enthusiasm for exercise interventions in clinical practice and have left open a number of crucial questions. Is exercise more beneficial for some patient subgroups and less so for other patients? Should exercise be prescribed as an augmentation strategy or as monotherapy? As most depressed patients are sedentary and disinclined to exercise, how might a clinician initiate and maintain patient adherence to an exercise intervention? Unanswered questions such as these have left exercise on the fringe of traditional treatments for depression and its benefits largely overlooked. This Commentary provides an overview of the benefits offered by exercise interventions as well as specific strategies for implementing exercise prescriptions in psychiatric practices.
On August 22, 2006, Michael W. Otto, Ph.D., an expert in cognitive-behavioral treatment of anxiety and mood disorders, assembled a group of experts in order to share and debate specific knowledge and strategies concerning the prescription of exercise as treatment for affective disorders. Their discussion appears here.
This special Commentary is another in a series of independently developed projects undertaken by the CME Institute of Physicians Postgraduate Press, Inc., as a service to its members and the broader academic community.
Faculty affiliations and financial disclosures appear at the end of this Commentary.
The opinions expressed herein are those of the faculty and do not necessarily reflect the views of the CME provider and publisher.
REFERENCES CITED
- Stathopoulou G, Powers M, and Berry A. et al. Exercise interventions for mental health: a quantitative and qualitative review. Clin Psychol Sci Pract. 2006 13:179–193. [Google Scholar]
- Trivedi M, Greer T, and Grannemann B. et al. TREAD: treatment and exercise augmentation for depression: study rationale and design. Soc Clin Trials. 2006 3:291–305. [DOI] [PubMed] [Google Scholar]
- Galper DI, Trivedi MH, and Barlow CE. et al. Inverse association between physical inactivity and mental health in men and women. Med Sci Sports Exerc. 2006 38:173–178. [DOI] [PubMed] [Google Scholar]
- Allgower A, Wardle J, Steptoe A.. Depressive symptoms, social support, and personal health behaviors in young men and women. Health Psychol. 2001;20:223–227. [PubMed] [Google Scholar]
- Van Gool CH, Kempen GI, and Penninx BW. et al. Relationship between changes in depressive symptoms and unhealthy lifestyles in late middle aged and older persons: results from the Longitudinal Aging Study Amsterdam. Age Aging. 2003 32:81–87. [DOI] [PubMed] [Google Scholar]
- Goodwin RD.. Association between physical activity and mental disorders among adults in the United States. Prev Med. 2003;36:698–703. doi: 10.1016/s0091-7435(03)00042-2. [DOI] [PubMed] [Google Scholar]
- Strawbridge WJ, Deleger S, and Roberts RE. et al. Physical activity reduces the risk of subsequent depression in older adults. Am J Epidemiol. 2002 156:328–334. [DOI] [PubMed] [Google Scholar]
- Blumenthal J, Babyak M, and Moore K. et al. Effects of exercise training on older patients with major depression. Arch Intern Med. 1999 159:2349–2356. [DOI] [PubMed] [Google Scholar]
- Craft L, Landers D.. The effects of exercise on clinical depression and depression resulting from mental illness: a meta-analysis. J Sport Exerc Psychol. 1998;20:339–357. [Google Scholar]
- Lawlor D, Hopker S.. The effectiveness of exercise as an intervention in the management of depression: systematic review and meta-regression analysis of randomized controlled trials. BMJ. 2001;322:763–767. doi: 10.1136/bmj.322.7289.763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunn A, Trivedi M, and Kampert J. et al. The DOSE study: a clinical trial to examine efficacy and dose response of exercise treatment for depression. Control Clin Trials. 2002 23:584–603. [DOI] [PubMed] [Google Scholar]
- Dunn AL, Trivedi MH, and Kampert JB. et al. Exercise treatment for depression: efficacy and dose response. Am J Prev Med. 2005 28:1–8. [DOI] [PubMed] [Google Scholar]
- Dunn A, Trivedi M, O'Neal H.. Physical activity dose-response effects on outcomes of depression and anxiety. Med Sci Sports Exerc. 2001;33:S587–S597. doi: 10.1097/00005768-200106001-00027. [DOI] [PubMed] [Google Scholar]
- Trivedi MH, Fava M, and Wisniewski SR. et al. Medication augmentation after the failure of SSRIs for depression. N Engl J Med. 2006 354:1243–1252. [DOI] [PubMed] [Google Scholar]
- Craft LL.. Exercise and clinical depression: examining two psychological mechanisms. Psychol Sport Exerc. 2005;6:151–171. [Google Scholar]
- Hassmen P, Koivula N, Uutela A.. Physical exercise and psychological well-being: a population study in Finland. Prev Med. 2000;30:17–25. doi: 10.1006/pmed.1999.0597. [DOI] [PubMed] [Google Scholar]
- Craft LL, Perna FM.. The benefits of exercise for the clinically depressed. Prim Care Companion J Clin Psychiatry. 2004;6:104–111. doi: 10.4088/pcc.v06n0301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trivedi M, Greer T, and Granneman B. et al. Exercise as an augmentation strategy for treatment of major depression. J Psychiatric Pract. 2006 12:205–213. [DOI] [PubMed] [Google Scholar]
- Rush A, Trivedi M, and Wisniewski S. et al. Acute and longer-term outcomes in depressed outpatients requiring one or several treatment: a STAR*D report. Am J Psychiatry. 2006 163:1905–1917. [DOI] [PubMed] [Google Scholar]
- Cooper LA, Gonzales JJ, and Gallo JJ. et al. The acceptability of treatment for depression among African-American, Hispanic, and white primary care patients. Med Care. 2003 41:479–489. [DOI] [PubMed] [Google Scholar]
- Dwight-Johnson M, Sherbourne CD, and Liao D. et al. Treatment preferences among depressed primary care patients. J Gen Intern Med. 2000 15:527–534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melfi C, Croghan T, and Hanna M. et al. Racial variation in antidepressant treatment in a medicaid population. J Clin Psychiatry. 2000 61:16–21. [DOI] [PubMed] [Google Scholar]
- Miranda J, Cooper LA.. Disparities of care for depression among primary care patients. J Gen Intern Med. 2004;19:1–10. doi: 10.1111/j.1525-1497.2004.30272.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olfson M, Marcus SC, and Druss B. et al. National trends in the outpatient treatment of depression. JAMA. 2002 287:203–209. [DOI] [PubMed] [Google Scholar]
- US Department of Health and Human Services. Mental health: culture, race, and ethnicity-a supplement to mental health: a report of the Surgeon General-executive summary. Rockville, Md: US Department of Health and Human Services, PHS Office of the Surgeon General; 2001 Available at http://www.surgeongeneral.gov/library/mentalhealth/cre/. [PubMed] [Google Scholar]
- Stein MB.. Sweating away the blues: can exercise treat depression? Am J Prev Med. 2005;28:140–141. doi: 10.1016/j.amepre.2004.09.024. [DOI] [PubMed] [Google Scholar]
- Cowie CC, Rust KF, and Byrd-Holt DD. et al. Prevalence of diabetes and impaired fasting glucose in adults in the US population: National Health and Nutrition Examination Survey 1999–2002. Diabetes Care. 2006 29:1263–1268. [DOI] [PubMed] [Google Scholar]
- Berlin J, Colditz G.. A meta-analysis of physical activity in the prevention of coronary heart disease. Am J Epidemiol. 1990;132:612–628. doi: 10.1093/oxfordjournals.aje.a115704. [DOI] [PubMed] [Google Scholar]
- Haennel R, Lemire F.. Physical activity to prevent cardiovascular disease: how much is enough? Can Fam Physician. 2002;48:65–71. [PMC free article] [PubMed] [Google Scholar]
- Wannamethee G, Shaper AG.. Physical activity and stroke in British middle aged men. BMJ. 1992;304:597–601. doi: 10.1136/bmj.304.6827.597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McTiernan A, Yasui Y, and Sorensen B. et al. Effect of a 12-month exercise intervention on patterns of cellular proliferation in colonic crypts: a randomized controlled trial. Cancer Epidemiol Biomarkers Prev. 2006 15:1588–1597. [DOI] [PubMed] [Google Scholar]
- Pinto B, Clark MM, and Maruyama NC. et al. Psychological and fitness changes associated with exercise participation among women with breast cancer. Psych-Oncology. 2003 12:118–126. [DOI] [PubMed] [Google Scholar]
- Van der Kooy K, Van Hout H, and Marwijk H. et al. Depression and the risk for cardiovascular diseases: systematic review and meta analysis. Int J Geriatr Psychiatry. 2007 epub ahead of print. [DOI] [PubMed] [Google Scholar]
- Blumenthal J, Babyak M, and Carney R. et al. Exercise, depression, and mortality after myocardial infarction in the ENRICHD trial. Med Sci Sports Exerc. 2004 36:746–755. [DOI] [PubMed] [Google Scholar]
- Jordan AN, Jurca GM, and Locke CT. et al. Pedometer indices for weekly physical activity recommendations in postmenopausal women. Med Sci Sports Exerc. 2005 37:1627–1632. [DOI] [PubMed] [Google Scholar]
- Murphy T, Pagano R, Marlatt G.. Lifestyle modification with heavy alcohol drinkers: effects of aerobic exercise on medication. Addict Behav. 1986;11:175–186. doi: 10.1016/0306-4603(86)90043-2. [DOI] [PubMed] [Google Scholar]
- Sundgot-Borgen J, Rosenvinge J, and Bahr R. et al. The effect of exercise, cognitive therapy, and nutritional counseling in treating bulimia nervosa. Med Sci Sports Exerc. 2002 34:190–195. [DOI] [PubMed] [Google Scholar]
- Fossati M, Armatti D, and Painot M. et al. Cognitive-behavioral therapy with simultaneous nutritional and physical activity education in obese patients with eating disorders. Eating Weight Disord. 2004 9:134–138. [DOI] [PubMed] [Google Scholar]
- Pendelton V, Goodrick G, and Poston W. et al. Exercise augments the effects of cognitive-behavioral therapy in the treatment of binge eating. Int J Eat Disord. 2002 31:172–174. [DOI] [PubMed] [Google Scholar]
- Broocks A, Bandelow B, and Pekrun G. et al. Comparison of aerobic exercise, clomipramine, and placebo in the treatment of panic disorder. Am J Psychiatry. 1998 155:603–609. [DOI] [PubMed] [Google Scholar]
- Otto MW, Smits JAJ, and Reese HE. Cognitive-behavioral therapy for the treatment of anxiety disorders. J Clin Psychiatry. 2004 65suppl 5. 34–41. [PubMed] [Google Scholar]
- Dishman R.. Brain monoamines, exercise, and behavioral stress: animal models. Med Sci Sports Exerc. 1997;29:63–74. doi: 10.1097/00005768-199701000-00010. [DOI] [PubMed] [Google Scholar]
- Dunn AL, Reigle TG, and Youngstedt SD. et al. Brain norepinephrine and metabolites after treadmill training and wheel running in rats. Med Sci Sports Exerc. 1996 28:204–209. [DOI] [PubMed] [Google Scholar]
- Zheng H, Liu Y, and Li W. et al. Beneficial effects of exercise and its molecular mechanisms on depression in rats. Behav Brain Res. 2006 15:168–171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sotsky S, Glass S, and Shea M. et al. Patient predictors of response to psychotherapy and pharmacotherapy: findings in the NIMH Treatment of Depression Collaborative Research Program. Am J Psychiatry. 1991 148:997–1008. [DOI] [PubMed] [Google Scholar]
- Ludman E, Katon W, and Bush T. et al. Behavioral factors associated with symptom outcomes in a primary care-based depression prevention intervention trial. Psychol Med. 2003 33:1061–1070. [DOI] [PubMed] [Google Scholar]