Abstract
Background
Appropriate utilization of acute reperfusion therapy is not a national performance measure for ST-elevation myocardial infarction at this time, and the extent of its contemporary use among ideal patients is unknown.
Methods
From the National Registry of Myocardial Infarction, we identified 238,291 patients enrolled from June 1994 to May 2003 who were ideally suited for acute reperfusion therapy with fibrinolytic therapy or primary percutaneous coronary intervention. We determined rates of not receiving therapy across 3 time periods (June 1994–May 1997, June 1997–May 2000, June 2000–May 2003) and evaluated factors associated with underutilization.
Results
The proportion of ideal patients not receiving acute reperfusion therapy decreased by one-half throughout the past decade (time period 1: 20.6%; time period 2: 11.4%; time period 3: 11.6%; P<0.001). Utilization remained significantly lower in key subgroups in the most recent time period: those without chest pain (OR, 0.29; 95% CI, 0.27–0.32); those presenting 6 to 12 hours after symptom onset (OR, 0.57; 95% CI, 0.52–0.61); those 75 years or older (OR, 0.63 compared with patients <55 years old; 95% CI, 0.58–0.68); women (OR, 0.88; 95% CI, 0.84–0.93); and non-whites (OR, 0.90; 95% CI, 0.83–0.97).
Conclusions
Utilization of acute reperfusion therapy in ideal patients has improved over the last decade, but more than 10% remain untreated. Measuring and improving its use in this cohort represents an important opportunity to improve care.
Keywords: ST-elevation myocardial infarction, reperfusion, fibrinolytic therapy, primary angioplasty
Introduction
In the U.S., recent quality improvement efforts for patients with ST-elevation myocardial infarction (STEMI) have focused primarily on measuring the timely delivery of acute reperfusion therapy.1, 2 Although shorter times-to-reperfusion are associated with better outcomes,3 the use of measures that focus on time alone fails to capture the degree to which acute reperfusion therapy is appropriately administered to all eligible patients. Earlier studies from the 1990s noted that approximately 25–40% of STEMI patients did not receive acute reperfusion therapy despite considerable evidence that its use lowers mortality.4–7 Although substantial improvements may have occurred in the intervening decade, recent data on its use in the U.S. are limited. If potential gaps in the use of acute reperfusion therapy are still present – particularly in high-risk patients who are otherwise eligible – this would argue for renewed efforts to measure and improve its utilization.
Accordingly, we assessed the contemporary use of acute reperfusion therapy in an ‘ideal’ cohort of patients using the National Registry of Myocardial Infarction (NRMI), a longstanding U.S. registry. To identify a population with the clearest indications for acute reperfusion therapy and one that will most likely reflect the target of national quality improvement efforts, our focus on ideal patients was intentionally selective. NRMI was designed in part to address this specific issue, containing detailed clinical information about indications and contraindications for acute reperfusion therapy, including patient refusal. In addition to examining overall trends, we specifically assessed use in several high-risk subgroups.4 Recognizing gaps in the actual receipt of acute reperfusion therapy among ideal patients has broad implications for patient care and future quality improvement efforts that currently overlook this important measure.
Methods
Study population
We used data in the NRMI-2, -3, and -4 cohorts collected from June 1994–May 2003. NRMI is an ongoing registry of patients with acute myocardial infarction admitted to participating hospitals in the U.S., and details of NRMI hospitals, cohorts and data collection have been described elsewhere.8 Briefly, the NRMI protocol specifies that all consecutive patients with the diagnosis of acute myocardial infarction are enrolled at participating hospitals. Cases are typically screened using the International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) discharge diagnosis code of 410.X1. Myocardial infarction is then confirmed based on a suggestive patient history and 1 or more of the following criteria: 1) cardiac biomarker (e.g., creatine kinase MB or troponin) elevation; 2) electrocardiographic evidence; and 3) scintigraphic, echocardiographic or autopsy evidence. The validity of NRMI data has been established through a comparison with the Cooperative Cardiovascular Project.8 Institutional review board approval is obtained at participating centers as required by the hospital.
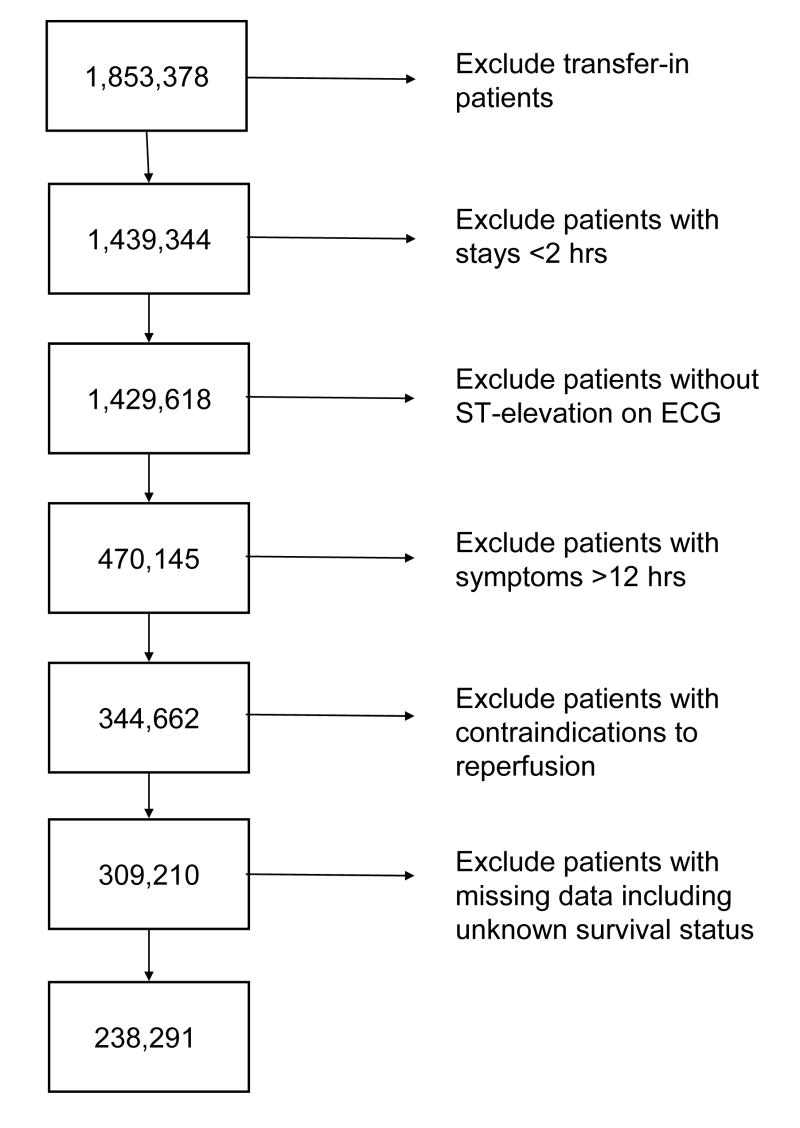
To construct a cohort of eligible patients ‘ideally’ suited for acute reperfusion therapy, we limited our analysis to non-transfer-in patients with: 1) symptoms of STEMI within 12 hours of presentation, 2) associated ST-elevation in 2 or more contiguous leads, and 3) no contraindications to either fibrinolytic therapy or percutaneous coronary intervention (PCI). A list of the contraindications to acute reperfusion therapy and the distribution of the population excluded for these reasons is listed in the Appendix. To focus on those patients with the clearest indications for acute reperfusion therapy, we excluded patients with left-bundle branch block pattern on their electrocardiogram, given the possibility that treatment was appropriately withheld. We also excluded those: 1) who did not receive acute reperfusion therapy with brief hospitalizations (<2 hours) due to death or emergent transfer because of insufficient time for treatment and 2) with any missing data elements. We also excluded cases where acute reperfusion therapy was withheld due to patient or family refusal; quality of life decision; and an unclear clinical diagnosis of STEMI. Figure 1 shows the sample selection process and specific exclusion criteria used to identify the final study population.
Figure 1.
Flow diagram displaying criteria for selection of study population
Outcome measures and data
The primary outcome assessed was whether a patient received acute reperfusion therapy with either fibrinolytic therapy or primary PCI. The key independent variables represented 3 time periods based on the date of hospital arrival: June 1994–May 1997 (time period 1), June 1997–May 2000 (time period 2), and June 2000–May 2003 (time period 3). We chose these 3 time periods to create an even distribution of patients and to ensure uniform data collection methods across the study period.
Patient-level characteristics that were also included in this analysis were: demographics (age [<55, 55–64, 65–74, >75], gender, race [white, non-white], insurance status [private, Medicare, other]; cardiovascular risk factors [smoking, hypertension, dyslipidemia, diabetes mellitus, family history of premature coronary artery disease]; prior coronary artery disease (prior angina, myocardial infarction, PCI, or coronary artery bypass grafting); prior congestive heart failure; prior stroke; presenting clinical variables (presence of chest pain, delayed presentation [>6–12 hours after symptom onset], systolic blood pressure [<90, >180], pulse [<50, >100], Killip classification [rales, pulmonary edema, cardiogenic shock], admission during off-hours [weekends and 7PM-7AM weekdays]); and electrocardiographic findings (anterior STEMI, number of leads involved). Hospital-level characteristics included type of ownership, teaching status, urban or rural location, U.S. Census region, and the availability of onsite cardiac surgery.
Statistical analysis
We performed univariate analyses to evaluate differences in baseline patient characteristics across the 3 time periods, with analysis of variance tests used for continuous variables and chi-squared tests used for categorical variables. We used multivariable logistic regression to determine the likelihood of receiving acute reperfusion therapy across the 3 time periods after adjusting for baseline differences in patient- and hospital-level characteristics. We calculated rates of not receiving acute reperfusion therapy by time period in the overall study population and key patient subgroups including those without chest pain or delayed presentation, those aged >75 years, women, and non-whites.4 To ensure that our results were not biased by differential hospital enrollment over the study period, we repeated the analysis only using patients at hospitals that enrolled during all 3 study periods (n=188,333) and showed similar results in general.
We also used multivariable logistic regression to identify patient-level characteristics associated with receiving acute reperfusion therapy in the cohort enrolled from June 2000 to May 2003 (i.e., time period 3). All models used generalized estimating equations (GEE) to account for clustering of patients at the hospital level. A P-value <0.05 was considered statistically significant. We report odds ratios for all associations from the multivariable models including their 95% confidence intervals. Statistical analyses were performed using SAS version 9.1 (SAS Institute, Cary, NC).
Results
Between June 1994 and May 2003, we identified 238,291 patients with STEMI who met our inclusion criteria and were ideally suited for acute reperfusion therapy. Overall, the mean age of these patients was 62.6 (±13.3) while 74,571 (31.3%) were women and 32,904 (14.0%) were non-white. Additional patient characteristics are displayed in Table 1. Due to the large size of the data set, statistically significant differences were found across the 3 time periods for several patient characteristics; however, for many variables absolute differences were small and not clinically significant. The proportion of patients with prior PCI increased from 7.8% to 12.1% during the study period, while the proportion of patients with Killip classification II, III, or IV decreased from 15.0% to 10.4%. The proportion of patients admitted at hospitals with on-site cardiac surgery increased from 46.8% to 56.5%.
Table 1.
Baseline characteristics of STEMI patients across the 3 time periods
| Period 1 6/94–5/97 N=80,481 882 Hospitals | Period 2 6/97–5/00 N=90,927 1,563 Hospitals | Period 3 6/00–5/03 N=66,883 1,262 Hospitals | P-Value | |
|---|---|---|---|---|
| No reperfusion therapy | 16,566 (20.6) | 10,406 (11.4) | 7,729 (11.6) | <0.001 |
|
| ||||
| Received fibrinolytic therapy | 54,299 (67.5) | 63,174 (69.5) | 37,129 (55.5) | <0.001 |
|
| ||||
| Received primary PCI | 9,616 (12.0) | 17,347 (19.1) | 22,025 (32.9) | <0.001 |
| Age, years | 63.2 ± 13.3 | 62.6 ± 13.2 | 61.8 ± 13.3 | <0.001 |
| Women | 26,377 (32.8) | 28,306 (31.1) | 19,888 (29.7) | <0.001 |
| Non-white | 10,463 (13.0) | 12,650 (13.9) | 9,791 (14.6) | <0.001 |
| Smoking | 28,895 (35.9) | 33,948 (37.3) | 26,779 (40.0) | <0.001 |
| Hypertension | 35,933 (44.6) | 42,302 (46.5) | 33,163 (49.6) | <0.001 |
| Diabetes mellitus | 15,956 (19.8) | 17,946 (19.7) | 12,746 (19.1) | <0.001 |
| Prior angina | 10,271 (12.8) | 8,231 (9.1) | 4,891 (7.3) | <0.001 |
| Myocardial infarction | 15,789 (19.6) | 16,007 (17.6) | 11,320 (16.9) | <0.001 |
| PCI | 6,263 (7.8) | 9,036 (9.9) | 8,076 (12.1) | <0.001 |
| CABG | 5,735 (7.1) | 6,270 (6.9) | 4,483 (6.7) | 0.006 |
| Congestive heart failure | 4,493 (5.6) | 4,206 (4.6) | 2,614 (3.9) | <0.001 |
| Stroke | 3,371 (4.2) | 3,493 (3.8) | 2,432 (3.6) | <0.001 |
| Chest pain | 74,025 (92.0) | 85,212 (93.7) | 63,032 (94.2) | <0.001 |
| Symptom duration before hospital arrival | 2.9 ± 2.4 | 2.7 ± 2.2 | 2.7 ± 2.3 | <0.001 |
| Anterior STEMI | 28,789 (35.8) | 31,786 (35.0) | 22,811 (34.1) | <0.001 |
| Killip classification II, III or IV | 12,090 (15.0) | 11,178 (12.3) | 6,935 (10.4) | <0.001 |
| SBP, mmHg | 0.27 | |||
| <90 | 3,708 (4.6) | 4,084 (4.5) | 3,123 (4.7) | |
| 90 to 180 | 68,698 (85.4) | 77,704 (85.4) | 56,915 (85.1) | |
| >180 | 8,075 (10.0) | 9,139 (10.1) | 6,845 (10.2) | |
| Pulse, beats per minute | <0.001 | |||
| <50 | 3,847 (4.8) | 4,421 (4.9) | 3,396 (5.1) | |
| 50 to 100 | 65,807 (81.8) | 75,097 (82.6) | 55,340 (82.7) | |
| >100 | 10,287 (13.5) | 11,409 (12.6) | 8,147 (12.2) | |
| Admitted off-hours (7PM-7AM & weekends) | 44,482 (55.3) | 50,426 (55.5) | 36,920 (55.5) | 0.56 |
| Hospital ownership | <0.001 | |||
| Private-Not-For-Profit | 65,131 (80.9) | 73,181 (80.5) | 53,807 (80.5) | |
| Private-For-Profit | 5,325 (6.6) | 5,934 (6.5) | 4,503 (6.7) | |
| Public (non-federal) | 9,852 (12.2) | 11,660 (12.8) | 8,548 (12.8) | |
| Public (federal) | 173 (0.2) | 152 (0.2) | 25 (0.04) | |
| Teaching hospital | 7,536 (9.4) | 7,686 (8.5) | 5,470 (8.2) | <0.001 |
| Primary PCI at hospital | 39,998 (49.7) | 45,907 (50.5) | 42,374 (63.4) | <0.001 |
|
| ||||
| On-site cardiac surgery | 37,698 (46.8) | 43,472 (47.8) | 37,806 (56.5) | <0.001 |
CABG, coronary artery bypass graft surgery; PCI, percutaneous coronary intervention; SBP, systolic blood pressure; STEMI, ST-elevation myocardial infarction
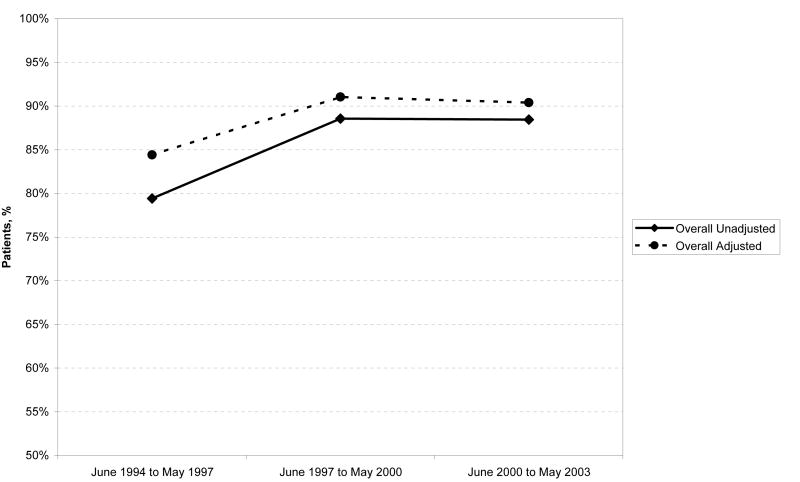
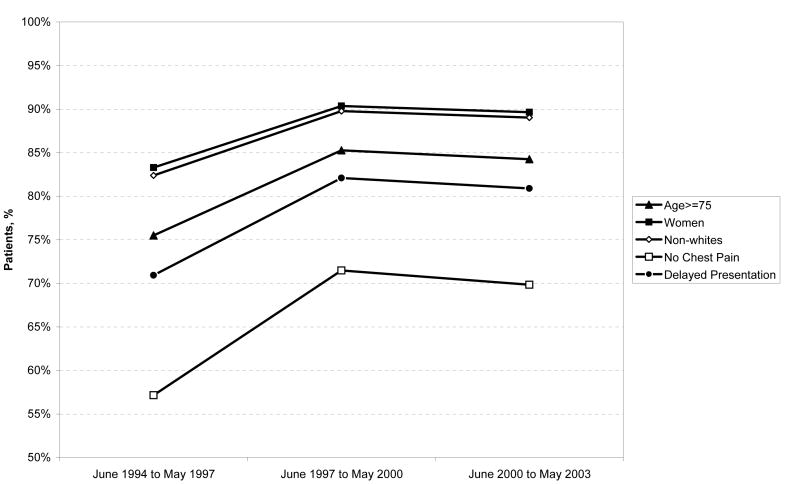
During the study period, 34,701 (14.6%) patients ideally suited for acute reperfusion therapy did not receive either fibrinolytic therapy or primary PCI. The proportion of patients who did not receive acute reperfusion therapy decreased significantly between time periods 1 and 2 but remained stable between time periods 2 and 3 (20.6% in time period 1 to 11.4% in time period 2 to 11.6% in time period 3; P <0.001 across all 3 time periods). This pattern of decline in the proportion of patients who did not receive acute reperfusion therapy remained after adjusting for baseline differences in patient and hospital characteristics across the 3 study periods (Figure 2). Similarly, in the key subgroups evaluated, the proportion of patients who did not receive acute reperfusion therapy decreased throughout the study period, although utilization in these patients remained generally lower than in the overall cohort (Figure 3).
Figure 2.
Unadjusted and adjusted rates of receiving reperfusion therapy in patients with STEMI
Figure 3.
Adjusted rates of receiving reperfusion therapy in key patient subgroups
Table 2 displays the patient characteristics independently associated with use of acute reperfusion therapy in the most recent time period between June 2000 and May 2003. In these patients, we identified several subgroups that were significantly less likely to receive acute reperfusion therapy including: those with advanced age (odds ratio [OR] for patients aged ≥75 years compared with patients aged <55 years, 0.63; 95% confidence interval (CI) 0.58–0.68); women (OR, 0.88; 95% CI, 0.84–0.93); non-whites (OR, 0.90; 95% CI, 0.83–0.97); those without chest pain (OR, 0.29; 95% CI, 0.27–0.32); and those presenting 6 to 12 hours after symptom onset (OR, 0.57; 95% CI, 0.52–0.61). We also found less utilization associated with co-morbidities like prior bypass surgery (OR, 0.67; 95% CI, 0.62–0.74), heart failure (OR, 0.69; 95% CI, 0.63–0.77) and angina (OR, 0.82; 95% CI, 0.75–0.90) as well as diabetes mellitus (OR, 0.87; 95% CI, 0.82–0.92) and hypertension (OR, 0.92; 95% CI, 0.87–0.97).
Table 2.
Adjusted odds ratios for receiving reperfusion therapy for patients with STEMI enrolled between June 2000 and May 2003
| Patient characteristic | Odds ratio (95% CI) |
|---|---|
| No chest pain on admission | 0.29 (0.27–0.32) |
| Delayed presentation (>6 hrs) | 0.57 (0.52–0.61) |
| Age ≥75 years* | 0.63 (0.58–0.68) |
| Prior CABG | 0.67 (0.62–0.74) |
| Pulse >100 beats per minute | 0.67 (0.62–0.71) |
| Prior heart failure | 0.69 (0.63–0.77) |
| Prior myocardial infarction | 0.71 (0.66–0.76) |
| Killip class III on admission† | 0.72 (0.62–0.83) |
| Systolic blood pressure >180 mmHg | 0.73 (0.68–0.78) |
| Prior angina | 0.82 (0.75–0.90) |
| Killip class II on admission† | 0.84 (0.77–0.92) |
| Diabetes mellitus | 0.87 (0.82–0.92) |
| Women | 0.88 (0.84–0.93) |
| Hypertension | 0.92 (0.87–0.97) |
| Non-white | 0.90 (0.83–0.97) |
| Smoking | 1.12 (1.06–1.19) |
| Prior PCI | 1.29 (1.18–1.41) |
| Systolic blood pressure <90 mmHg | 1.60 (1.38–1.85) |
| Pulse <50 beats per minute | 2.13 (1.84–2.48) |
| ST-segment elevation 3 or 4 leads | 2.55 (2.39–2.72) |
| ST-segment elevation ≥5 leads | 4.45 (4.01–4.94) |
Compared with age <55 years
Compared with Killip class I
CABG, coronary artery bypass graft surgery; CI, confidence interval; PCI, percutaneous coronary intervention; STEMI, ST-segment elevation myocardial infarction
Discussion
We found substantial improvement in the use of acute reperfusion therapy among ideal patients with STEMI between 1994 and 2003 in the U.S. Most of this improvement appeared to occur during the late 1990s and has leveled off over recent years. It could be that a ‘ceiling’ effect has been reached, since an expectation of perfect utilization (i.e., 100%) may be unrealistic even in patients without identifiable contraindications. However, it is concerning that we found substantial and persistent gaps in utilization for several key subgroups such as those without chest pain or with delayed presentations, the very elderly, women, and minorities. Patients with co-morbidities such as prior bypass surgery, heart failure or angina as well as diabetes mellitus and hypertension were also less likely to receive acute reperfusion therapy. The disparities in utilization across these groups of patients who are either at high-risk for complications following STEMI (e.g., the elderly) or less likely to receive reperfusion therapy (e.g., women) suggest that there is still substantial room for improving use of this life-saving therapy.
Recently time-to-reperfusion has received much attention as an important quality standard for assessing care in STEMI patients.1, 2 While important, time-to-reperfusion does not assess the appropriate use of acute reperfusion therapy in eligible patients, and current measures from the Joint Commission on Accreditation of Healthcare Organizations and the Centers for Medicare & Medicaid Services do not consider it in their overall evaluations of hospital quality.1, 2 A recent statement by the American College of Cardiology (ACC)/American Heart Association (AHA) on performance measures for STEMI and non-STEMI patients recognizes the potential limitation of excluding the use of reperfusion in national quality improvement efforts, and recommends including such a measure in the future.9
Our findings support the incorporation of a measure of reperfusion use into national quality improvement efforts for STEMI patients. Approximately 10% of patients who appear otherwise ideally suited for acute reperfusion therapy do not receive it. Improving this figure could lead to substantial improvements in mortality especially when compared with other interventions proposed for STEMI patients. For example, the use of fibrinolytic therapy is associated with absolute mortality reductions of 30 per 1000 treated in patients presenting within 6 hours of symptom onset and 20 per 1000 treated in those presenting 6 to 12 hours after symptom onset.10 In contrast, improving time-to-reperfusion by 3 to 6 hours in patients presenting late after symptom onset is associated with an absolute mortality reduction of 11 per 1000.11 Shifting patients from fibrinolytic therapy to primary PCI may be associated with absolute mortality reductions of 12 to 20 per 1000 patients treated if performed in a timely manner.12, 13
Including measures of the use of acute reperfusion therapy in assessments of hospital quality will also help to highlight persistent disparities in its utilization in high-risk subgroups. We noted that patients without chest pain or those with delayed presentation continue to have a much lower likelihood of receiving acute reperfusion therapy. Similarly, we found lower utilization of acute reperfusion therapy among very elderly patients, women, and non-whites as well as those with co-morbidities such as prior bypass surgery, heart failure and angina. For the most part, these discrepancies were present to a comparable degree in earlier analyses from NRMI and others.4, 14–17 Thus, while absolute rates of utilization of acute reperfusion therapy in high-risk subgroups generally have improved over time, relative differences remain.4
There are a number of factors that may contribute to underutilization of acute reperfusion therapy particularly in high-risk subgroups that are otherwise ideally suited for it. Previous arguments have suggested that some clinicians may be uncomfortable with its use in certain patients due to perceptions of less benefit or greater risk, contributing to underutilization.18, 19 This is a possible explanation for its low use in patients without chest pain or even those with delayed presentation, although it contradicts available clinical evidence.10, 19–21 In addition, this argument fails to explain its underutilization in groups like the very elderly, women and non-whites.
Despite considerable debate, reasons for lower use of treatment in these patients are unknown and clearly not endorsed by current guidelines.22 Many of these groups have been shown to receive less aggressive therapy in other settings, such as those providing invasive cardiovascular procedures, with possible explanations including differences in eligibility or other clinical factors.16 However, our analyses demonstrated persistent disparities even after multivariable adjustment. In the very elderly, another possibility for underutilization is concern about overall frailty and the higher likelihood for complications even though these higher risk patients may benefit more from acute reperfusion therapy.19, 23, 24 Such a “risk-treatment” paradox has been described recently regarding heart failure and dyslipidemia.25, 26 This may also explain its lower use in patients with pre-existing conditions including heart failure, prior myocardial infarction, diabetes mellitus, and hypertension.27
Our analysis should be interpreted in the context of the following study design issues. First, NRMI collects voluntarily reported data from participating hospitals. While NRMI hospitals do include a wide variety of acute-care hospitals, these centers generally tend to be larger than non-participating hospitals. Our results therefore may not be generalizable to all U.S. hospitals. Second, this was an observational study and there is the potential for residual confounding despite adjustment for several patient- and hospital-level covariates. We lacked data, for example, on some patient characteristics that may have contributed to underutilization, including the presence of chronic renal insufficiency or socioeconomic factors.
Despite these limitations, this study has unique strengths. In particular, we were able to use the extensive data available in NRMI to establish an ‘ideal’ cohort that was eligible for acute reperfusion therapy. In contrast to other studies, we were able to exclude patients with non-clinical contraindications such as patient or family refusal, or a quality of life decision. We also excluded patients with left bundle branch block patterns, focusing on those with ST-elevation on their presenting electrocardiograms (similar to the strategy proposed by the ACC/AHA).9 Patients with left bundle branch block pattern remain a challenging subset in which determining whether treatment was appropriately withheld is often difficult.28 Finally, we excluded those patients who did not receive acute reperfusion therapy with brief hospitalizations (<2 hours) due to death or emergent transfer because of insufficient time for initiating treatment. As a result of these factors, our estimates of underutilization are more conservative than those found in prior reports from NRMI and others.4–7
While utilization of acute reperfusion therapy has improved over the last decade, approximately 10% of ideal patients do not receive adequate treatment. Measuring its appropriate utilization in this population will be important to assess hospital performance in acute myocardial infarction and possibly improve quality of care. In particular, it may be valuable for quality efforts to focus on high-risk subgroups such as those without chest pain or with delayed presentation that continue to have significantly lower rates of utilization. Recent recommendations by the ACC/AHA Task Force on Performance Measures have also endorsed incorporating a measure of reperfusion use into national quality improvement efforts for STEMI patients and are supported by our findings.
Clinical significance
While use of acute reperfusion therapy has improved over the last decade, more than 10% of eligible patients with STEMI still do not receive it.
Substantial gaps in utilization are most prominent in high-risk groups like STEMI patients without chest pain or with delayed presentations, the very elderly, women and minorities.
Improving use of acute reperfusion therapy could lead to substantial improvements in mortality compared with other interventions proposed for STEMI patients.
National quality improvement efforts should consider incorporating a measure of reperfusion use for assessing hospital performance in acute myocardial infarction.
Acknowledgments
Disclosures: Dr. Barron reports that he is the Chief Medical Officer of Genentech, the developer of tPA and TNK and the sponsor of NRMI. Dr. Canto reports that he receives research funds from Pfizer and Schering-Plough; is on speakers’ bureaus for Pfizer, Sanofi-Aventis, Bristol-Myers Squibb, and GlaxoSmithKline; consults for Pfizer, Sanofi-Aventis, Bristol-Myers Squibb, and GlaxoSmithKline; and is on the NRMI/Genentech advisory board. Drs. Morris and Blaney report that they are employed by Genentech. Ms. Parsons and Mr. Miller report that they are employed by Ovation Research Group, a company that receives research funding from Genentech. Dr. Krumholz reports that he has research contracts with the Colorado Foundation for Medical Care and the American College of Cardiology, serves on the advisory boards for Amgen, Alere and UnitedHealthcare, is a consultant for Centegen, is a subject matter expert for VHA, Inc., and is Editor-in-Chief of Journal Watch Cardiology of the Massachusetts Medical Society.
Funding Sources: This project was supported by the National Heart, Lung, and Blood Institute (R01 HS072575). Genentech, Inc. (South San Francisco, CA) approved the study and provided access to NRMI data without charge.
Appendix. Distribution of contraindications to reperfusion therapy in overall cohort
| Contraindication | No. of patients |
|---|---|
| Active internal bleeding or known bleeding diathesis | 5,173 |
| History of stroke | 5,662 |
| History of intracranial neoplasm, AVM or aneurysm | 392 |
| Recent surgery or trauma | 3,939 |
| Severe uncontrolled hypertension | 1,297 |
| Traumatic cardiopulmonary resuscitation | 2,944 |
| Patient or family refusal | 2,826 |
| Refusal due to quality of life decision | 5,025 |
| An unclear clinical diagnosis of STEMI | 5,493 |
| Other or not clearly specified | 9,709 |
| Total | 35,412* |
Total is less than the sum of the individual components due to overlap AVM, arteriovenous malformation; STEMI, ST-elevation myocardial infarction
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Williams SC, Schmaltz SP, Morton DJ, et al. Quality of care in U.S. hospitals as reflected by standardized measures, 2002–2004. N Engl J Med. 2005;353:255–64. doi: 10.1056/NEJMsa043778. [DOI] [PubMed] [Google Scholar]
- 2.Jha AK, Li Z, Orav EJ, Epstein AM. Care in U.S. hospitals--the Hospital Quality Alliance program. N Engl J Med. 2005;353:265–74. doi: 10.1056/NEJMsa051249. [DOI] [PubMed] [Google Scholar]
- 3.Williams DO. Treatment delayed is treatment denied. Circulation. 2004;109:1806–8. doi: 10.1161/01.CIR.0000126892.17646.83. [DOI] [PubMed] [Google Scholar]
- 4.Barron HV, Bowlby LJ, Breen T, et al. Use of reperfusion therapy for acute myocardial infarction in the United States: data from the National Registry of Myocardial Infarction 2. Circulation. 1998;97:1150–6. doi: 10.1161/01.cir.97.12.1150. [DOI] [PubMed] [Google Scholar]
- 5.Rogers WJ, Canto JG, Lambrew CT, et al. Temporal trends in the treatment of over 1.5 million patients with myocardial infarction in the US from 1990 through 1999: the National Registry of Myocardial Infarction 1, 2 and 3. J Am Coll Cardiol. 2000;36:2056–63. doi: 10.1016/s0735-1097(00)00996-7. [DOI] [PubMed] [Google Scholar]
- 6.Eagle KA, Goodman SG, Avezum A, et al. Practice variation and missed opportunities for reperfusion in ST-segment-elevation myocardial infarction: findings from the Global Registry of Acute Coronary Events (GRACE) Lancet. 2002;359:37–7. doi: 10.1016/S0140-6736(02)07595-5. [DOI] [PubMed] [Google Scholar]
- 7.Hasdai D, Behar S, Wallentin L, et al. A prospective survey of the characteristics, treatments and outcomes of patients with acute coronary syndromes in Europe and the Mediterranean basin; the Euro Heart Survey of Acute Coronary Syndromes (Euro Heart Survey ACS) Eur Heart J. 2002;23:1190–201. doi: 10.1053/euhj.2002.3193. [DOI] [PubMed] [Google Scholar]
- 8.Every NR, Frederick PD, Robinson M, et al. A comparison of the National Registry of Myocardial Infarction 2 with the Cooperative Cardiovascular Project. J Am Coll Cardiol. 1999;33:1886–94. doi: 10.1016/s0735-1097(99)00113-8. [DOI] [PubMed] [Google Scholar]
- 9.Krumholz HM, Anderson JL, Brooks NH, et al. ACC/AHA clinical performance measures for adults with ST-elevation and non-ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Performance Measures (Writing Committee to Develop Performance Measures on ST-Elevation and Non-ST-Elevation Myocardial Infarction) Circulation. 2006;113:732–61. doi: 10.1161/CIRCULATIONAHA.106.172860. [DOI] [PubMed] [Google Scholar]
- 10.Fibrinolytic Therapy Trialists’ (FTT) Collaborative Group. Indications for fibrinolytic therapy in suspected acute myocardial infarction: collaborative overview of early mortality and major morbidity results from all randomised trials of more than 1000 patients. Lancet. 1994;343:311–22. [PubMed] [Google Scholar]
- 11.Boersma E, Maas AC, Deckers JW, Simoons ML. Early thrombolytic treatment in acute myocardial infarction: reappraisal of the golden hour. Lancet. 1996;348:771–5. doi: 10.1016/S0140-6736(96)02514-7. [DOI] [PubMed] [Google Scholar]
- 12.Melandri G. The obsession with primary angioplasty. Circulation. 2003;108:e162. doi: 10.1161/01.CIR.0000102947.33318.E8. [DOI] [PubMed] [Google Scholar]
- 13.Keeley EC, Boura JA, Grines CL. Primary angioplasty versus intravenous thrombolytic therapy for acute myocardial infarction: a quantitative review of 23 randomised trials. Lancet. 2003;361:13–20. doi: 10.1016/S0140-6736(03)12113-7. [DOI] [PubMed] [Google Scholar]
- 14.Gurwitz JH, Gore JM, Goldberg RJ, et al. Recent age-related trends in the use of thrombolytic therapy in patients who have had acute myocardial infarction. National Registry of Myocardial Infarction. Ann Intern Med. 1996;124:283–91. doi: 10.7326/0003-4819-124-3-199602010-00001. [DOI] [PubMed] [Google Scholar]
- 15.Canto JG, Allison JJ, Kiefe CI, et al. Relation of race and sex to the use of reperfusion therapy in Medicare beneficiaries with acute myocardial infarction. N Engl J Med. 2000;342:1094–100. doi: 10.1056/NEJM200004133421505. [DOI] [PubMed] [Google Scholar]
- 16.Vaccarino V, Rathore SS, Wenger NK, et al. Sex and racial differences in the management of acute myocardial infarction, 1994 through 2002. N Engl J Med. 2005;353:671–82. doi: 10.1056/NEJMsa032214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Krumholz HM, Murillo JE, Chen J, et al. Thrombolytic therapy for eligible elderly patients with acute myocardial infarction. JAMA. 1997;277:1683–1688. [PubMed] [Google Scholar]
- 18.Ayanian JZ, Hauptman PJ, Guadagnoli E, et al. Knowledge and practices of generalist and specialist physicians regarding drug therapy for acute myocardial infarction. N Engl J Med. 1994;331:1136–42. doi: 10.1056/NEJM199410273311707. [DOI] [PubMed] [Google Scholar]
- 19.Alter DA, Ko DT, Newman A, Tu JV. Factors explaining the under-use of reperfusion therapy among ideal patients with ST-segment elevation myocardial infarction. Eur Heart J. 2006;27:1539–49. doi: 10.1093/eurheartj/ehl066. [DOI] [PubMed] [Google Scholar]
- 20.Cox DA, Rogers WJ, Aguirre FV, et al. Effect on outcome of the presence or absence of chest pain at initiation of recombinant tissue plasminogen activator therapy in acute myocardial infarction. The Thrombolysis in Myocardial Infarction Investigators. Am J Cardiol. 1994;73:729–36. doi: 10.1016/0002-9149(94)90872-9. [DOI] [PubMed] [Google Scholar]
- 21.Canto JG, Shlipak MG, Rogers WJ, et al. Prevalence, clinical characteristics, and mortality among patients with myocardial infarction presenting without chest pain. JAMA. 2000;283:3223–9. doi: 10.1001/jama.283.24.3223. [DOI] [PubMed] [Google Scholar]
- 22.Antman EM, Anbe DT, Armstrong PW, et al. ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction--executive summary. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 1999 Guidelines for the Management of Patients with Acute Myocardial Infarction) J Am Coll Cardiol. 2004;44:671–719. doi: 10.1016/j.jacc.2004.07.002. [DOI] [PubMed] [Google Scholar]
- 23.Mehta RH, Granger CB, Alexander KP, et al. Reperfusion strategies for acute myocardial infarction in the elderly: benefits and risks. J Am Coll Cardiol. 2005;45:471–8. doi: 10.1016/j.jacc.2004.10.065. [DOI] [PubMed] [Google Scholar]
- 24.Krumholz HM, Pasternak RC, Weinstein MC, et al. Cost effectiveness of thrombolytic therapy with streptokinase in elderly patients with suspected acute myocardial infarction. N Engl J Med. 1992;327:7–13. doi: 10.1056/NEJM199207023270102. [DOI] [PubMed] [Google Scholar]
- 25.Lee DS, Tu JV, Juurlink DN, et al. Risk-treatment mismatch in the pharmacotherapy of heart failure. JAMA. 2005;294:1240–7. doi: 10.1001/jama.294.10.1240. [DOI] [PubMed] [Google Scholar]
- 26.Ko DT, Mamdani M, Alter DA. Lipid-lowering therapy with statins in high-risk elderly patients: the treatment-risk paradox. JAMA. 2004;291:1864–70. doi: 10.1001/jama.291.15.1864. [DOI] [PubMed] [Google Scholar]
- 27.Parker AB, Naylor CD, Chong A, Alter DA. Clinical prognosis, pre-existing conditions and the use of reperfusion therapy for patients with ST segment elevation acute myocardial infarction. Can J Cardiol. 2006;22:131–9. doi: 10.1016/s0828-282x(06)70252-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Shlipak MG, Lyons WL, Go AS, et al. Should the electrocardiogram be used to guide therapy for patients with left bundle-branch block and suspected myocardial infarction? JAMA. 1999;281:714–9. doi: 10.1001/jama.281.8.714. [DOI] [PubMed] [Google Scholar]