Abstract
Background
Conventional abdominal surgery in grossly obese patients is associated with an increased rate of postoperative complications; thus, laparoscopic surgery may be preferred in these patients.
Patients and methods
A prospective analysis was performed of 20 grossly obese patients who underwent laparoscopic cholecystectomy between April 1996 and April 2000 for symptomatic non-complicated gallstone disease.
Results
Technical problems at operation included difficulty with induction of pneumoperitoneum and introduction of the most lateral subcostal port, retraction of the gallbladder fundus, the need for longer instruments and the closure of the fascia. Laparoscopic cholecystectomy was successfully completed in 19 patients, but one patient required conversion to open operation. There were no anaesthetic difficulties. Two patients developed minor chest infections. The mean hospital stay was 2.9 days.
Conclusion
Laparoscopic cholecystectomy is feasible and can be recommended for symptomatic gallstone disease in grossly obese patients.
Keywords: Laparoscopic cholecystectomy, obesity
Introduction
Conventional abdominal surgery in the grossly obese is associated with an increased rate of wound infection, atelectasis, respiratory tract infection and deep vein thrombosis (DVT) in the postoperative period 6. Furthermore, operations in the obese are also associated with technical problems such as difficulty with access and retraction of the abdominal wall and viscera 1,2,3,4. For these reasons, grossly obese patients pose considerable anaesthetic and surgical risks to the extent that many referring doctors and indeed surgeons often postpone elective operation indefinitely. This policy will expose these patients with symptomatic non-malignant disease to the increased risks of potential emergency procedure.
Laparoscopic cholecystectomy (LC) results in less postoperative pain, a decreased incidence of atelectasis and chest infection, rapid mobilisation and early discharge from hospital 5. Clearly LC has attributes, but are of benefit to the majority of patients, but can the grossly obese share these benefits?
We prospectively studied and report on a group of 20 grossly obese patients with gallstone disease undergoing cholecystectomy.
Patients and methods
Between April 1996 and April 2000 patients with a body mass index (BMI) greater than 35 were studied [BMI = Weight(kg)/Height(m2)]. The minimum BMI level chosen represents patients in the upper range of group II and group III obesity as defined by Garrow 6. The major inclusion criteria for this study were gross obesity and symptomatic gallstone disease needing cholecystectomy. Patients were excluded from the study if there was a history of jaundice, deranged liver function tests, acute cholecystitis, the need for pre-operative ERCP or ultrasongraphic findings to suggest biliary obstruction. All patients were admitted one day preoperatively for investigations including full blood count, urea and electrolytes, blood glucose, liver function tests, chest x-ray, electrocardiogram and abdominal ultrasound scan. Date of admission, discharge, hospital stay, operative time, operative difficulties, conversion to open procedure and any immediate postoperative complications were recorded. All patients were seen in outpatients clinic at 6 weeks, 6 months and one year postoper-atively, when any symptoms were recorded.
A senior anesthetist (consultant or senior registrar) examined all patients on the eve of the operation. When deemed necessary, oral premedication with temazepam was given 2 hours before operation. Prophylaxis against DVT was provided in the form of thromboembolic deterrent stockings (TEDS) plus 5000 units of subcutaneous heparin (Minihep Calcium Syringe; Calcium Heparin: Leo Laboratories Ltd, Bucks, UK) given with the premedication. Each patient received cefuroxime lg intravenously at the time of induction of anaesthesia, or erythromycin lg if sensitive to penicillin.
Surgical technique
In each case operation was commenced using the standard method of insufflation, with the Veress needle inserted through an infra-umbilical stab incision. Once a 3.5 litre pneumoperitoneum had been established with a maximum intra-abdominal pressure of 12mm Hg, the Veress needle was replaced by a 10mm port and a camera was introduced. The other standard ports were subsequently inserted under direct vision. The procedure was performed with the patient in the reverse Trendelenberg position with the operating table rotated to the left. Because of the large size of these patients it was felt necessary to strap them to the operating table with appropriate cushioning of the pressure areas. The operations were performed in the standard way, with identification of the cystic duct and the cystic artery in the triangle of Calot and their subsequent division between clips. The gall bladder was then dissected off its bed using either a Dubois hook or endoshears according to the surgeon's preference. There was no need to perform an operative cholangiogram in any patient in this study and this was not done routinely. Drainage of the pouch of Morrison was not needed. The gallbladder was in all instances retrieved via the epigastric port. Deflation of the peritoneal cavity was always carried out via the epigastric port and all ports were removed under direct vision making sure that no loops of bowel were pulled into port sites. The infra-umbilical and epigastric wounds were both routinely closed using Vicryl sutures on a J-shaped needle (Ethicon Ltd., Edinburgh, U.K.) for the fascial layer and the skin was closed with subcuticular Vicryl.
Oral fluid intake was commenced upon transfer of the patients to the ward and patients were commenced on a light diet on the evening of the operation. Prophylaxis against DVT was continued for 24 hours postoperatively or until full mobilisation was attained.
Results
Over the four-year period elective LC was attempted in 20 consecutive patients with a BMI greater than 35 kg/m2. Seventeen women and three men were recruited. Their mean age was 50 years [range 30–70 years] and their mean (SD) BMI was 38.2 kg.m2 (2.7) [range 35.1–42.6].
Laparoscopic cholecystectomy was successfully completed in 19 patients. In one 35-year-old woman with a BMI of 39.5 kg/m2, conversion to open cholecystectomy was required owing to an inability to establish a pneumoperitoneum. The range of operating time was 73-183 minutes (median 97.6 minutes). The range of hospital stay was 2-9 days (median 2.9 days). No patient required chest physiotherapy postoperatively. There were no anaesthetic problems either intraoperatively or postoperatively, and no patient required admission to a high dependency or intensive care unit. There were no episodes of clinical DVT or wound infection but patients had minor chest infections which delayed discharge from hospital. No port site hernia was recorded after a median follow up time of 25.1 months (range 6–54 months).
Technical problems at operation
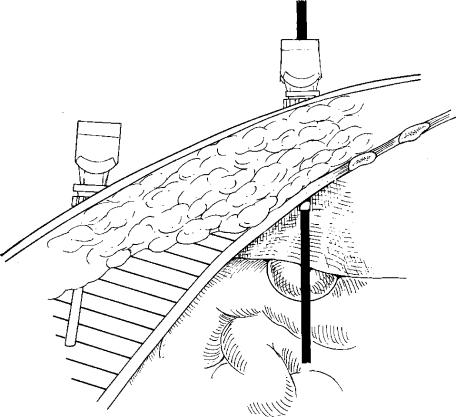
Difficulty with insertion of the Veress needle was encountered in 5 of the 20 patients. There was one complete failure in which attempted cutdown for direct introduction of the port (Hassan technique) also failed. This was the reason for converting the only case to open operation in this series. Open insertion of the trocar can be virtually impossible when a thick layer of fat is present, especially when the pendulous nature of the abdomen causes the umbilicus to descend almost to the level of the pubic symphysis. To circumvent this problem we introduced the needle via a sub-costal stab incision (Figure 1).
Figure 1. .
Pleumoperitoneum is best achieved by inserting the Veress needle via a subcostal stab incision (open insertion of a trocar at the umbilicus is not recommended).
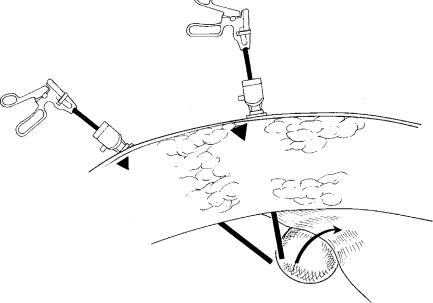
Another difficulty was encountered in pushing the fundus of the gallbladder upwards into the suprahepatic space with grasping forceps placed in the lower or most lateral of the subcostal ports. This manoeuvre is important because the traction thus obtained helps expose the structures in calot's triangle. If the lateral subcostal port is placed too close to the costal margin and inserted perpendicular to the skin, manipulation of the grasping forceps is made very difficult by the depth of subcutaneous fat. By inserting the port further caudally and at an angle towards gallbladder (Figure 2), the need for manipulating the forcepts is much reduced. Once the gallbladder is grasped, it need only be pushed along the axis of the port.
Figure 2. .
Subcostal ports are best introduced at an angle towards the gallbladder (not perpendicular to the skin). The lateral subcostal port is inserted further caudally (not too close to the costal margin).
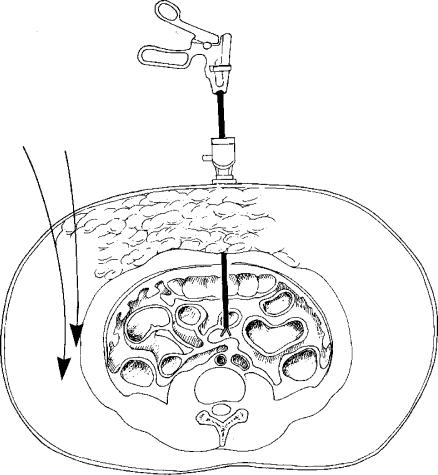
Problems were encountered on insertion of the lateral subcostal port in 3 patients. The port was placed too far laterally and the cannula skirted the peritoneal cavity without entering it (Figure 3). Inserting a long spinal needle or the Veress needle under direct vision to pre-judge the direction before the definitive port is introduced was found to be helpful.
Figure 3. .
If the lateral subcostal port is inserted too far laterally, it may be difficult to enter the peritoneal cavity.
In another 3 patients, additional strategically placed ports were required because of difficulty in reaching the gallbladder using standard instruments via the standard ports. Usually changing ports and introducing grasping instruments via the epigastric port and scissors or hook via the medial subcostal port circumvented the problem. However in these 3 patients these manoeuvres did not solve the problem and an extra port was therefore required at a strategic site.
Finally some difficulty was encountered in all 19 patients when it came to closure of the fascia in the epigastric and infraumbilical wounds. The importance of closure of the fascia has been stressed by recent reports of intestinal obstruction and umbilical hernia following laparoscopic surgery 7,15. It is therefore routinely performed in all patients in our unit. Some difficulty in this regard was encountered in this group of grossly obese patients. We managed the problem by withdrawing the infraumbilical port and camera simultaneously until the fascia came into view. The fascia was then picked up under direct vision by Kocher's forcepts inserted alongside the port. The camera and port were then removed, and closure was effected using Kocher's forceps as a guide.
Discussion
This prospective analysis studied 20 grossly obese patients undergoing laparoscopic cholecystectomy, concentrating on the technical difficulties, operative time, conversion rate, complications and hospital stay. The study shows that there are several technical problems associated with the large size of these patients. These problems can be overcome by modifying standard surgical techniques, however. The only technical problem that necessitated conversion to operation was failure to establish a pneumoperitoneum. Once a pneumoperitoneum was established, each operation followed lines similar to LC in normal-size patients. Although the amount of fat in the triangle of Calot may be greater in the grossly obese, careful dissection still allows identification of the relevant structures and their safe management. The availability of longer instruments would have been useful, but they are not absolutely necessary for the safe conduct of LC in this special group of patients.
The ventilatory problems that are posed by creation of a pneumoperitoneum during laparoscopy – increased PaCO2, risks of pneuothorax and pneumomediastinum, gas embolism – are compounded by obesity. Up to 23% of the obese population have coexisting respiratory diseases 9. The decrease in pulmonary compliance together with ventilation-perfusion mismatching and intra-pulmonary shunting of blood predisposes to hypoxia. Against the background of an increased oxygen consumption and carbon dioxide production in the obese 10, this hypoxia may prove difficult to correct. Obesity is also a major risk factor for ischaemic heart disease 11,12 and hypertension 13, both of which serve to increase the risk from general anaesthesia. A high incidence of hiatus hernia and gastroesophageal reflux has been reported in this population 14. Nonetheless, our patients did not require ventilation, and there were no anaesthetic difficulties.
Conversion rate and complications associated with LC depend on the experience of the surgeon 8. This study showed a low rate of conversion to open cholecystectomy (5%). Champault and colleagues reviewed 110 obese patients who underwent (LC); the conversion rate was 4.5% in obese patients and 1.8% in non-obese patients 16. The conversion rate reported in grossly obese ranges from 1.1% 17 to 11.4% 18 depending on surgical experience and the inclusion of gallstone complications, notably acute cholecystitis. Although some studies have shown a higher conversion rate in grossly obese patients 16, most reports show no significant difference from the rate in the non-obese 17,18,21.
Likewise, obesity increased the difficulty of LC and prolonged the operative time in some reports 18,20, but not in others 17,21. In this study the median operative time was 97.6 minutes, which compared favourably with other published data 16,21.
The long-held assumption that morbid obesity is associated with an increased incidence of postoperative complications is supported by few objective data. The incidence of wound infection 22 and pulmonary complications 23 may be higher following open abdominal operations, but most recent reports of LC in obese and non-obese patients showed no significant difference in complication rate or hospital stay 16,17,20,21,24. In our series of patients there were no wound infections, no ventilatory problems and no episodes of DVT. Two patients developed minor chest infection which was treated successfully by antibiotics.
Acknowledgements
The authors would like to thank Mrs Jan Sharpe, Department of Medical Illustration, University Hospital of Wales, for preparing the figures.
References
- 1.Burnand KG. Taylor I. Vol. 3 Churchill Livingstone; Edinburgh: 1989. The current management and complications of venous thrombosis, Progress in Surgery. [Google Scholar]
- 2.Bergqvist D. Springer-Verlag; Berlin: 1983. Post operative Thromboembolism. [Google Scholar]
- 3.Bothe AJR, Bistrian BR, Greenberg I, Blackburn GL. Energy regulation in morbid obesity by multidisciplinary therapy. Surg Clin N Am. 1979;59:1017–31. doi: 10.1016/s0039-6109(16)41981-x. [DOI] [PubMed] [Google Scholar]
- 4.Sawyer RG, Pruett TL. Wound infections. Surg Clin N Am. 1994;74:519–536. [PubMed] [Google Scholar]
- 5.Delicata RJ, Rees BI, Carey PD. Physiological responses in laparoscopic surgery. In:Laparoscopic Colorectal Surgery. ISIS Medical Media (in press), Oxford: [Google Scholar]
- 6.Garrow JS. Churchill Livingstone; Edinburgh: 1981. Treat obesity seriously – a clinical manual. [Google Scholar]
- 7.Boyce D, Fligelstone L, Wheeler M. Unusual complication of laparoscopic cholecystectomy. Ann R Coll Surg Engl. 1992;74:254–5. [PMC free article] [PubMed] [Google Scholar]
- 8.Schrenk P, Woisetschlager R, Rieger R, Wayand WU. A diagnostic score to predict the difficulty of a laparoscopic chole cystectomy from pre-operative variables. Surg Endosc. 1998;12:148–50. doi: 10.1007/s004649900616. [DOI] [PubMed] [Google Scholar]
- 9.Buckley FP, Robinson NB, Simonowitz DA, Dellinger EP. Anaesthesia in the morbidly obese. A comparison of anaesthetic and analgesic regimens for upper abdominal surgery. Anaesthesia. 1983;38:840–51. doi: 10.1111/j.1365-2044.1983.tb12249.x. [DOI] [PubMed] [Google Scholar]
- 10.Luce MJ. Respiratory complications of obesity. Chest. 1980;78:626–31. doi: 10.1378/chest.78.4.626. [DOI] [PubMed] [Google Scholar]
- 11.Hubert HB, Feinleib M, McNamara PM, Casteli WB. Obesity as an independent risk factor for cardiovascular disease; A 26 year follow up of patients in the Framingham heart study. Circulation. 1983;67:968–77. doi: 10.1161/01.cir.67.5.968. [DOI] [PubMed] [Google Scholar]
- 12.Rabkin SW, Mathewson FAL, Hsu PH. Relation of body weight to development of ischaemic heart disease in a cohort of young North American men after a 26 year observation period: The Manitoba study. Am J Cardiol. 1977;39:452–8. doi: 10.1016/s0002-9149(77)80104-5. [DOI] [PubMed] [Google Scholar]
- 13.Dunstan HP. Obesity and hypertension. Ann Intern Med. 1985;103:1047–9. doi: 10.7326/0003-4819-103-6-1047. [DOI] [PubMed] [Google Scholar]
- 14.Krai G. Morbid obesity and related health risks. Ann Intern Med. 1985;103:1043–7. doi: 10.7326/0003-4819-103-6-1043. [DOI] [PubMed] [Google Scholar]
- 15.Azurin DJ, Go LS, Arroyo LR, Kirkland ML. Trocar site herniation following laparoscopic cholecystectomy and the significance of an incidental pre-existing umbilical hernia. Am Surg. 1995;61:718–20. [PubMed] [Google Scholar]
- 16.Champault G, Colon A, Rizk N, Benoit J, Fabre F, Boutelier P. Laparoscopic cholecystectomy in obese patients: 110 cases. Chirurg. 1996;121:15–8. [PubMed] [Google Scholar]
- 17.Phillips EH, Carroll BJ, Fallas MJ, Pearlstein AR. Comparison of laparoscopic cholecystectomy in obese and non-obese patients. Am Surg. 1994;60:316–21. [PubMed] [Google Scholar]
- 18.Nies C, Bartsch D, Rothmund M. Laparoscopic cholecystectomy in morbid obesity. Indicators or contradictions? Chirurg. 1994;65:29–32. [PubMed] [Google Scholar]
- 19.Sakuramoto S, Sato S, Okuri T, Sato K, Hiki Y, Kakita A. Pre-operative evaluation to predict technical difficulties of laparoscopic cholecystectomy on the basis of histological inflammation findings on resected gall bladder. Am J Surg. 2000;179:114–21. doi: 10.1016/s0002-9610(00)00248-8. [DOI] [PubMed] [Google Scholar]
- 20.Angrisani L, Lorenzo M, De Palma G, Sivero L, Catanzano C, Tesauro B, Persico G. Laparoscopic cholecystectomy in obese patients compared with non-obese patients. Surg Laparosc Endosc percut Techn. 1995;5:197–201. [PubMed] [Google Scholar]
- 21.Gatsoulis N, Koulas S, Kiparos G, Tzafestas N, Pangratis K, Pandis K, Mavrakis G. Laparoscopic cholecystectomy in obese and non-obese patients. Obesity Surg. 1999;9:459–61. doi: 10.1381/096089299765552756. [DOI] [PubMed] [Google Scholar]
- 22.Garrow JS, Hastings EJ, Cox AG. Obesity and post operative complications of abdominal operations. Br Med J. 1988;297:181. doi: 10.1136/bmj.297.6642.181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Poe RH, Kallay MC, Dass T, Celebic A. Can post operative pulmonary complications after cholecystectomy be predicted? Am J Med Sci. 1988;295:29–34. doi: 10.1097/00000441-198801000-00007. [DOI] [PubMed] [Google Scholar]
- 24.Schirmer BD, Die J, Edge SB. Laparoscopic cholecystectomy in the obese patients. Ann Surg. 1992;216:146–52. doi: 10.1097/00000658-199208000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]