Abstract
Background
Previously surgical operation was the only accepted treatment for hydatid liver cysts. Recently percutaneous management has become more preferable because of its low morbidity rate and lower cost.
Patients and methods
In all, 101 patients harbouring 120 hydatid cysts of the liver were treated by percutaneous drainage between October 1994 and December 1997. Of these cysts, 89 were in the right liver and 31 in the left liver.Thirty-one patients had had previous operations for hydatid disease. All cysts had an anechoic or hypoechoic unilocular appearance on ultrasound scan. The mean dimension of the cysts was 7.5±2.9 cm (range 3–10.4 cm). All patients received oral albendazole 10 mg/kg perioperatively. After aspiration under sonographic guidance, cysts were irrigated with 95% ethanol.
Results
The amount of cyst fluid aspirated was 220±75 ml and the amount of irrigation solution used was 175±42 ml. Four patients developed mild fever and three had urticaria. Mean length of hospital stay was 2.1±0.7 (range 1–4) days, and patients were followed up for 43–62 months (mean 54±5.4 months). Maximal cyst diameter decreased from 7.5±2.9 cm to 3.2±15 cm (p<0.001). Sonographic examinations revealed high-level heterogeneous echoes in the cyst cavity (heterogeneous echo pattern), while the cyst cavity was completely obliterated by echogenic material (pseudotumour echo pattern).
Discussion
Most hydatid cysts of the liver can be managed successfully by a combination of drug therapy and percutaneous drainage.
Keywords: hydatid disease, percutaneous drainage, ultrasound.
Introduction
Ultrasonography is considered the method of first choice in the diagnosis of hydatid liver cyst, and different sonographic appearances of the disease have been described extensively 1,2,3. Although percutaneous needle puncture or aspiration of hepatic hydatid cysts has supposedly been contraindicated because of the potential complications of anaphylactic shock or spread of hydatid daughter cysts to the peritoneum 4,5,6,7, aspiration of such cysts without these complications has been reported 8,9.
We report the long-term results of percutaneous drainage of 120 hydatid cysts of the liver in 101 patients.
Patients and methods
In all, 101 patients with 120 hydatid cysts of the liver were treated by percutaneous drainage between October 1994 and December 1997.
Ultrasound scan was used for imaging and follow-up in all patients. According to Gharbi's classification 1, type 1 cysts (pure fluid collection) and type 2 cysts (fluid collection with a split wall) were included, whereas type 3 cysts (fluid collection with daughter cysts) and type 4 cysts (heterogeneous echo pattern) were excluded.
Of the cysts, 89 were in the right liver and 31 in the left liver; 31 patients had had previous operations for hydatid disease of the liver; 85 patients had a single cyst, while 13 patients had two cysts and another three had 3 cysts in the liver. The indirect haemaglutination test was positive in 87 patients (87%).
Right upper quadrant pain and abdominal discomfort were the most common symptoms at presentation (36 and 22 patients, respectively). The other patients were asymptomatic at the time of diagnosis. The commonest physical finding was hepatomegaly (21 patients). Other cyst data are shown in Table 1.
Table 1. Characteristics of 101 patients with hydatid disease of the liver.
| Characteristic | No. |
|---|---|
| Number of the cysts in the liver | |
| 1 | 85 |
| 2 | 13 |
| 3 | 3 |
| Type of cyst | |
| Type 1 | 38 |
| Type 2 | 82 |
| Dimension | |
| < 5 cm | 14 |
| 5–10 cm | 91 |
| > 10 cm | 15 |
| Clinical presentation | |
| Asymptomatic | 43 |
| Upper right quadrant pain | 36 |
| Abdominal discomfort | 22 |
| Physical finding | |
| Hepatomegaly | 21 |
Percutaneous drainage was performed under aseptic conditions with continuous sonographic guidance and intensive monitoring to treat any complications. Using a transhepatic approach, the cyst was punctured by a 20-gauge needle and cyst contents were aspirated rapidly. After aspiration, the cyst was filled with a near-equal volume of 95% ethanol which was left in the cavity for 20 min. Finally the cyst was reaspirated and irrigated and was left partially filled with sterile 0.9% saline. Before and after injection of 95% ethanol, cyst fluid was sent immediately for cytological and microbiological examination. Staining with neutral red indicated a viable cyst, while staining with methylene blue and eosin indicated a non-viable cyst 10.
Percutaneous drainage was successful if the endocyst separated from the pericyst and if the reaspirated fluid showed a non-viable cyst. If not, percutaneous drainage was repeated at the same sitting to obtain success.
After percutaneous drainage had been performed, all patients received albendazole 10 mg/kg body weight for 6 weeks.
The patients were observed for 24 hours and were then discharged from the hospital if the procedure had been uneventful.
Statistical analysis was performed by the χ2 test, p values <0.05 were accepted as significant.
Results
All cysts were treated successfully by means of percutaneous drainage and ethanol instillation. After puncture the aspirated fluid was clear in all patients. During the procedure the endocyst separated from the pericyst (Figures 1 and 2). The amount of cyst fluid aspirated was 220±75 ml and the amount of ethanol infused into the cyst cavity was 175±42 ml.
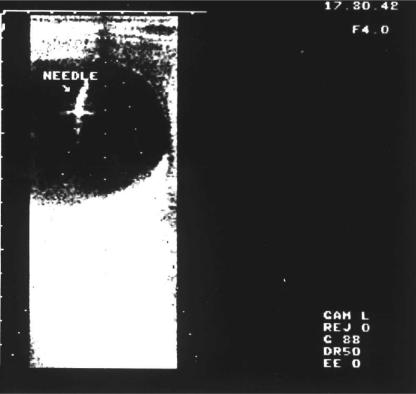
Figure 1. .
Ultrasonographic appearance of type 1 liver hydatid cyst during percutaneous drainage.
Figure 2. .
Separation of the endocyst 20 min after injection ofscoliddal agent.
Four (4%) patients developed mild fever and three (3%) patients had urticaria. There were no other complications. The mean hospital stay was 2.1±0.7 days (range 1–4 days).
Follow-up ranged between 43 and 62 months (mean 54±5.4 months). In the first 6-month period sonographic examination was performed monthly, then once a year for the next 5 years. Repeated sonographic examinations revealed a progressive decrease in cyst size and an alteration in cyst appearance. The initial cyst diameter of 7.5±2.9 cm decreased to 3.2±1.5 cm (p < 0.001). Ultrasound scans revealed either high-level heterogeneous echoes in the cyst cavity (heterogeneous echo pattern) (Figure 3), or the cyst cavity was completely obliterated by echogenic material (pseudotumour echo pattern) (Figure 4).
Figure 3. .
Heterogeneous echo pattern of the cyst 6 months after percutaneous drainage.
Figure 4. .
Echogenic pattern (pseudotumour) obtained 18 months after the procedure.
All patients were relieved of symptoms related to their hydatid cyst in the liver. They noticed relief of pain in the abdomen, and the liver span decreased in those with hepatomegaly.
Discussion
Operative treatment used to be accepted as the first choice in the treatment of hepatic hydatid cysts 11. Percutaneous needle puncture and aspiration was thought to be dangerous because of complications such as anaphylactic shock or spread of hydatid daughter cysts to the peritoneum 4,5,6,7. Although anaphylactic shock from rupture of an echinococcal cyst has been documented 12, its exact frequency and mechanism have not been studied 13. Lewall and McCorkell reported 20 patients who had hepatic hydatid cyst rupture without anaphylaxis 14.
Since percutaneous radiological catheter drainage of abdominal abscesses and fluid collections is well established as a safe alternative to surgical therapy 15,16,17, Mueller and colleagues treated hepatic echinococcal cysts successfully by means of aspiration and alcohol injection 13. Subsequently percutaneous drainage has been accepted as an alternative treatment to surgery.
Screening and diagnostic studies of hydatid disease have improved, and satisfactory diagnostic criteria have now been established with the help of imaging methods 18. Among imaging methods, ultrasonography is favoured for guidance of percutaneous drainage because of its low cost and repeatability. As suitable drugs are not available in liquid phase 19, the residual fluid of the cyst must be inactivated by a scolicidal agent. Many agents have been tried, but 95% alcohol and hypertonic saline are used most frequently nowadays. In the present study, 95% alcohol was chosen because of its documented safety and efficacy 19,20.
Mueller et al.13 reported one patient who underwent successful percutaneous drainage of hydatid cyst of the liver; the catheter was left in place in the cavity for 3 months. In later reports percutaneous drainage was performed in a single stage. After drainage of the cysts and irrigation with a scolicidal agent, the catheter was removed 21,22. We aspirated all 120 cysts in a single stage and removed the catheter after aspiration and irrigation.
We performed percutaneous drainage in Gharbi type 1 and type 2 hydatid cysts 1. The procedure could not have been successful in cysts with a hyperechoic solid pattern.
Infected cysts and cysts that communicate with the biliary tree still require operation to evacuate the infected cyst contents and drain the biliary tree.
Although percutaneous drainage has been accepted as a safe procedure in hydatid disease of the liver 19,22,23, the long-term clinical outcome is not yet clear. The unresolved question as to whether cyst growth can occur locally or in the peritoneal cavity as a result of fluid spillage and dissemination indicated the use of a transhepatic approach with routine administration of oral albendazole (10 mg/kg body weight).
The possibility of infection of the cyst cavity, local recurrence, biliary rupture and sclerosing cholangitis led us to repeat monthly sonographic examinations for the first 6 months, and to follow the patients for as long as possible. At follow-up ranging from 43 to 62 months, repeated sonographic examinations revealed a progressive decrease in cyst size and alteration in cyst appearance. The cyst cavity was completely obliterated by echogenic material, giving the appearance of a pseudotumour. Local or peritoneal cyst growth has not been seen.
We conclude that percutaneous drainage is a safe method for treating uncomplicated hydatid cysts. It has a lower morbidity and a lower cost than traditional surgical operation.
References
- 1.Gharbi HA, Hassine W, Brauner MW, Dupuch K. Ultrasound examination of the hydatid liver. Radiology. 1981;139:459–63. doi: 10.1148/radiology.139.2.7220891. [DOI] [PubMed] [Google Scholar]
- 2.Hadidi A. Sonography of hepatic echinococcal cyst. Gastrointest Radiol. 1982;7:349–54. doi: 10.1007/BF01887669. [DOI] [PubMed] [Google Scholar]
- 3.Lewall DB, McCorkell SJ. Hepatic echinococcal cyst: sono graphic appearance and classification. Radiology. 1985;155:773–5. doi: 10.1148/radiology.155.3.3890008. [DOI] [PubMed] [Google Scholar]
- 4.Hankins J, Werner D, Kobout E. Surgical treatment of ruptured and unruptured hydatid cyst of the lung. Ann Surg. 1968;167:336–41. doi: 10.1097/00000658-196803000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pissiotis CA, Wander JV, Condon RE. Surgical treatment of hydatid disease. Arch Surg. 1972;104:454–9. doi: 10.1001/archsurg.1972.04180040068012. [DOI] [PubMed] [Google Scholar]
- 6.Rutledge R, Benson M, Thomas CG., Jr A technique for drainage, irrigation, and sterilization of intrahepatic echinococcal cyst. Surg Rounds. 1984;2:56–61. [Google Scholar]
- 7.Schiller CF. Complications of Echinococcus cyst rupture. JAMA. 1966;195:158–60. [PubMed] [Google Scholar]
- 8.Livraghi T, Bosoni A, Giordano F, et al. Diagnosis of hydatid cyst by percutaneous aspiration: value of electrolyte determinations. J Clin Ultrasound. 1985;13:333–7. doi: 10.1002/jcu.1870130507. [DOI] [PubMed] [Google Scholar]
- 9.Bret PM, Fond L, Bretagnolle M, et al. Percutaneous aspiration and drainage of hydatid cysts in the liver. Radiology. 1988;168:617–20. doi: 10.1148/radiology.168.3.3043542. [DOI] [PubMed] [Google Scholar]
- 10.Gori S, Campatellis A, Luchi S, et al. Cytology in the percutaneous treatment of hydatid cysts. A report of four cases. Acta Cytol. 1993;30:423–6. [PubMed] [Google Scholar]
- 11.Lewis JV, Koss N, Kerstein MD. A review of echinococcal disease. Ann Surg. 1975;181:390–6. doi: 10.1097/00000658-197504000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yahya Al, Przybylski J, Foud A. Anaphylactic shock in a patient with ruptured hydatid liver cyst owing to trivial abdominal trauma. J R Coll Surg Edinb. 1997;42:423–4. [PubMed] [Google Scholar]
- 13.Mueller PR, Dawson SL, Ferruci JT, Jr, Nardi GL. Hepatic echinococcal cyst: successful percutaneous drainage. Radiology. 1985;155:627–8. doi: 10.1148/radiology.155.3.3890001. [DOI] [PubMed] [Google Scholar]
- 14.Lewall DB, McCorkell SJ. Rupture of echinococcal cyst: diagnosis, classification, and clinical implications. AJR. 1986;146:391–4. doi: 10.2214/ajr.146.2.391. [DOI] [PubMed] [Google Scholar]
- 15.Gerzof SG, Robbins AH, Johnson WC, et al. Percutaneous catheter drainage of abdominal abscesses guided by ultrasound and computed tomography. AJR. 1979;133:1–8. doi: 10.2214/ajr.133.1.1. [DOI] [PubMed] [Google Scholar]
- 16.van Sonnenberg E, Mueller PR, Ferruci JT., Jr Percutaneous drainage of 250 abdominal abscesses and fluid collections. Part I. Results, failures, and complications. Radiology. 1984;151:337–41. doi: 10.1148/radiology.151.2.6709901. [DOI] [PubMed] [Google Scholar]
- 17.Mueller PR, van Sonnenberg E, Ferruci JT., Jr Percutaneous drainage of 250 abdominal abscesses and fluid collections. Part II. Current procedural concepts. Radiology. 1984;151:343–7. doi: 10.1148/radiology.151.2.6709903. [DOI] [PubMed] [Google Scholar]
- 18.Suwan Z. Sonographic findings in hydatid disease of the liver, comparison with other diagnostic methods. Ann Trop Med Parasitol. 1995;89:261–9. doi: 10.1080/00034983.1995.11812951. [DOI] [PubMed] [Google Scholar]
- 19.Filicie C, Pirpla F, Brunetti E, et al. A new therapeutic approach for hydatid liver cysts. Aspiration and alcohol injec tion under sonographic guidance. Gastroenterology. 1990;98:1366–8. doi: 10.1016/0016-5085(90)90358-8. [DOI] [PubMed] [Google Scholar]
- 20.Bean WJ, Rodan BA. Hepatic cysts, treatment with alcohol. AJR. 1985;144:237–41. doi: 10.2214/ajr.144.2.237. [DOI] [PubMed] [Google Scholar]
- 21.Bastid C, Azar C, Doyer M, Sahel J. Percutaneous treatment of hydatid cyst under sonographic guidance. Dig Dis Sci. 1994;39:1576–80. doi: 10.1007/BF02088067. [DOI] [PubMed] [Google Scholar]
- 22.Khuroo MS, Zargar SA, Mahajan RM. Echinococcus granulosus cysts in the liver: management with percutaneous drainage. Radiology. 1991;180:141–5. doi: 10.1148/radiology.180.1.2052682. [DOI] [PubMed] [Google Scholar]
- 23.Akhan O, Ozmen MN, Dincer A, et al. Liver hydatid disease: long term results of percutaneous treatment. Radiology. 1996;198:259–64. doi: 10.1148/radiology.198.1.8539390. [DOI] [PubMed] [Google Scholar]