Abstract
Background
Despite refinements in the management of choledochal cysts in children, an increasing number of patients present with ongoing symptoms in adult life. The aim of this study was to review the management of adult patients with choledochal cysts in a tertiary referral centre.
Method
A retrospective review was carried out of all adult patients presenting with choledochal cysts to this department between 1992 and 2000. Patient records were reviewed and detailed analyses were made of the clinical presentation, radiological and biochemical findings, anatomical anomalies, management, complications and outcomes.
Results
Of 16 patients (12 women and 4 men; median age 23 years), 8 had undergone previous upper gastrointestinal operations before referral, including 5 who had had previous cyst drainage procedures. All patients underwent elective complete cyst excision with Roux-en-Y hepaticojejunostomy. There were no operative deaths and there was a low early postoperative morbidity rate (25%). There was no evidence of biliary malignancy in any cyst. During a median postoperative follow-up of 44 months, five patients (31%) continued to experience cholangitis and two of these required additional revisional procedures, but are now symptom-free.
Conclusion
Patients with choledochal cysts should be referred to specialised tertiary surgical units. Total choledochal cyst excision with Roux-en-Y hepaticojejunostomy is the treatment of choice. Patients with previous inadequate cyst excisional procedures should undergo revisional surgery, to reduce recurrent symptoms and the risk of developing cholangiocarcinoma.
Keywords: choledochal cyst, cholangitis, hepaticojejunostomy, cholangiocarcinoma, cystduodenostomy
Introduction
Choledochal cysts are rare cystic transformations of the biliary tree that are increasingly diagnosed in adult patients 1,2,3,4. These congenital lesions have a female:-male preponderance of 4:1, with an incidence in the West of between 1 in 50 000 and 1 in 200 000 live births 3; they are much more frequent in Asia 5,6. Nearly 25% of choledochal cysts are detected in the first year of life and 60% in the first decade, but 20% are diagnosed after the age of 20 years 1,7.
Adults with cysts are especially predisposed to the development of cholangiocarcinoma, with the cancer incidence increasing from 0.7% in the first decade of life to >14% after the age of 20 years 8,9,10. Several reports have documented long-term complications following the paediatric management of choledochal cysts using cystenterostomy without total cyst excision 8,11,12. Many centres now see an increasing number of adult patients who have either had previous operative procedures (without cyst excision) or experience ongoing complications related to a cyst in situ 7,13,14,15,16; up to 80% experience recurrent cholangitis and pancreatitis.
Because of the risk of malignant change in choledochal cysts, the ideal treatment is excision of the entire dilated biliary tree with reconstruction using a Roux-en-Y hepaticojejunostomy 3,9,10,17. We present a contemporary cohort of adult patients with choledochal cysts, which emphasises the complexity and diversity of this disorder in adults.
Methods
In a retrospective review of all adults presenting with choledochal cysts to the Royal Infirmary of Edinburgh, Scotland, between 1992 and 2000, patients were identified by means of the Lothian Surgical Audit and their medical and operative records were reviewed. Detailed analyses were made of the clinical presentation, radiological and biochemical findings, anatomical anomalies, management, complications and outcomes.
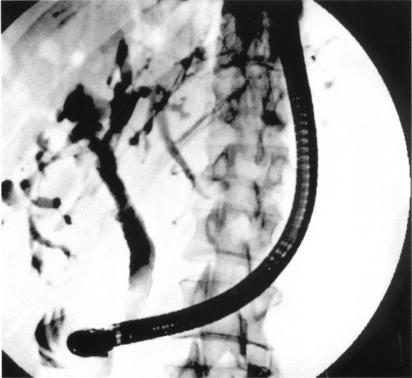
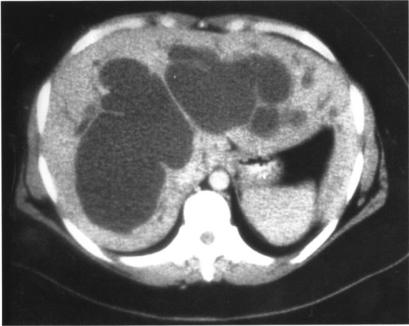
Investigation of the patients was dictated by their presentation, but generally involved assessment of the biliary tree by endoscopic retrograde cholangio-pancreatography (ERCP) (Figure 1) and computed tomography (CT) scanning (Figure 2).
Figure 1. .
ERCP demonstrating extrahepatic and intrahepatic biliary duct dilatation in a type IV choledochal cyst.
Figure 2. .
CT scan demonstrating intrahepatic biliary duct dilatation in a type IV choledochal cyst.
Patients with choledochal cysts in situ underwent total cyst excision with reconstruction of the biliary tract by means of a Roux-en-Y hepaticojejunostomy. Patients with Caroli's disease were excluded from the series.
Results
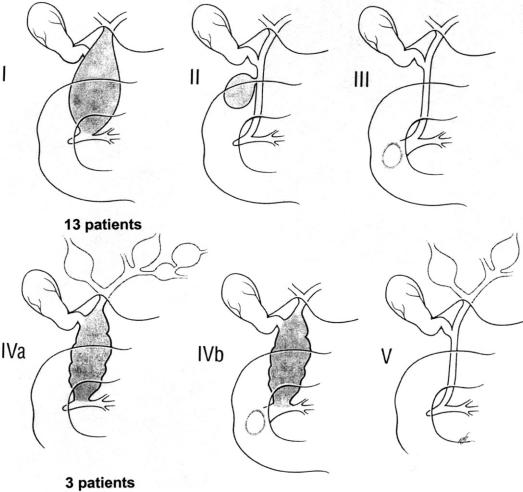
Sixteen patients (12 women and 4 men) were identified, with a median age of 23 years (range 18–49 years). According to the modified Todani classification, 13 patients had type I cysts and 3 had type IVa cysts (Figure 3).
Figure 3. .
The modified Todani classification, and distribution of choledochal cysts in this series.
Eight of the 16 patients had undergone operations before referral to this institution (Table 1). One of these patients had presented previously to a local hospital as an adult with severe abdominal pain and underwent laparotomy without notable findings. In retrospect, he probably had cholangitis and an infected choledochal cyst. A second patient had presented with a history of recurrent idiopathic pancreatitis and had undergone transduodenal sphincteroplasty and cholecystectomy, but the relevance of her choledochal cyst was not appreciated at that time. One patient underwent cholecystectomy for recurrent upper abdominal pain, again without diagnosis or recognition of the choledochal cyst. The remaining five patients underwent cystduodenostomy for known choledochal cysts in childhood. The cyst (or part of the cyst) remained in situ in all patients who had undergone previous operation.
Table 1. Patient characteristics, previous operations, follow-up and complications.
| Age (years) | Sex | Todani classification | Previous operation | Length of follow-up (months) | Complications | Cholangitis | Re-operation |
|---|---|---|---|---|---|---|---|
| 30 | M | Type I | 111 | + | |||
| 49 | F | Type I | Partial cyst excision and cystduodenostomy | 101 | |||
| 20 | M | Type I | 51 | Subphrenic abscess | |||
| 19 | F | Typel | Partial cyst excision and cystduodenostomy | 51 | + | + | |
| 23 | F | Type I | 44 | ||||
| 36 | F | Type I | Cholecystectomy | 40 | |||
| 32 | F | Type I | Cystduodenostomy and cholecystectomy | 37 | Mild pancreatitis | ||
| 18 | F | Type I | 35 | Bile leak | |||
| 23 | F | Type I | Cystduodenostomy and cholecystectomy | 33 | + | + | |
| 31 | M | Type I | Negative exploratory laparotomy for right upper quadrant pain | 29 | Bile leak | ||
| 19 | F | Type I | 27 | ||||
| 31 | F | Type I | Transduodenal sphincteroplasty and cholecystectomy | 23 | |||
| 21 | F | Type I | 21 | ||||
| 18 | M | Type IVa | Cystduodenostomy | 105 | + | ||
| 31 | F | Type IVa | 90 | ||||
| 31 | F | Type IVa | 51 | + | |||
All patients presented with symptoms of recurrent abdominal pain. Other symptoms included recurrent nausea in 13, vomiting in 8, dyspepsia in 4 and weight loss in 3. At referral, 10 patients had a history of at least one episode of cholangitis and 5 had previous pancreatitis. Median duration of symptoms before referral was 10 months (range 1 week to 6 years). Abnormal liver function tests were recorded in 69% of patients at the time of diagnosis. These levels did not remain consistently abnormal, and all patients had normal laboratory tests at the time of operation.
All patients underwent elective definitive surgery in this unit, comprising complete cyst excision and Roux-en-Y hepaticojejunostomy. In all but one case, the biliary-enteric anastomosis was fashioned at the biliary confluence using interrupted 4/0 PDS sutures. One patient, who had had dense adhesions and scarring following a previous procedure, underwent a single anastomosis to include the left hepatic duct. No patient required separate anastomoses to the right and left hepatic ducts, and no internal stents or access loops were employed in any of the patients. The 12 patients with intact gallbladders also underwent cholecystectomy.
A number of anomalies were identified during investigation or at operation (Table 2), including the presence of an anomalous pancreatobiliary junction (APBJ) (10 patients), an aberrant hepatic artery (4 patients), primary ductal stricture (2 patients), a prominent accessory papilla (1 patient) and an accessory gallbladder (1 patient). In addition, seven patients had cholelithiasis, six patients had stones within the choledochal cyst and two patients had intrahepatic stones. Histological assessment confirmed choledochal cyst in all cases with no evidence of malignancy.
Table 2. Hepatobiliary pathology associated with the choledochal cysts in this series.
| Pathology | Number | Percentage |
|---|---|---|
| Anomalous pancreato-biliary junction | 10 | 63 |
| Primary ductal stricture | 2 | 13 |
| Secondary ductal stricture | 5 | 31 |
| Aberrant hepatic artery | 4 | 25 |
| Prominent accessory papilla | 1 | 6 |
| Accessory gallbladder | 1 | 6 |
| Cholelithiasis | 7 | 44 |
| Cystolithiasis | 6 | 38 |
| Intrahepatic stones | 2 | 13 |
There were no operative deaths, while 4 of the 16 patients (25%) had minor postoperative complications (Table 1). Two patients developed bile leaks and one patient had an episode of mild pancreatitis. These three complications settled spontaneously without the need for further intervention. One patient developed a subphrenic collection, which was drained percutaneously. The median postoperative length of hospital stay was 8 days (range 6–12 days).
During a median postoperative follow-up of 44 months (range 21–111 months), five patients had at least one further episode of cholangitis (Table 1). Three of these patients had type I cysts (two with previous cystduodenostomy) and two had type IVa cysts (one with previous cystduodenostomy). Two of the symptomatic patients have required revisional surgery. The first patient had a type I cyst treated previously with partial cyst excision and cystduodenostomy 12 years before definitive surgery in this unit. She subsequently developed intrahepatic ductal calculi and required anastomotic revision and stone extraction from the left duct system. The second patient also had a type I cyst and had undergone previous cystduodenostomy as a child. She developed an anastomotic stricture and required revisional surgery. Both patients remain symptom-free at 33 and 51 months after re-operation.
Discussion
We present the management of a series of adult patients with choledochal cysts and symptoms related to the presence of the cyst in situ. Their presentations did not follow any classical patterns. Many had episodic and non-specific symptoms, but all experienced abdominal pain and most had episodes of cholangitis. Although 69% had abnormal liver function tests, none of these were consistently abnormal. This fact may explain why the diagnosis was often delayed, and inappropriate upper gastrointestinal surgery (with incorrect diagnoses) was performed in three of the eight patients who had been operated elsewhere. Five patients had previously undergone inadequate procedures for their choledochal cysts in the form of cystduodenostomy and had recurrent symptoms related to the cyst remnant. The literature reports that up to 80% of such patients will have recurrent symptoms 15,16 and that up to 69% will subsequently require revisional surgery 18,19,20.
Although early postoperative morbidity was low, five patients (31%) developed recurrent cholangitis and two (13%) have required additional revisional procedures at our institution. This finding emphasises the difficulty in managing adult patients with this condition and the dangers of exposing the patient to the risks of secondary sclerosing cholangitis following an inappropriate operation.
Yamataka and co-workers 21 reported a 23% incidence of postoperative cholangitis after primary definitive cyst excision of type I cysts, while other authors have reported the incidence to range up to 40% in adults 4,15,22. This figure is even higher for type IVa cysts, ranging from 31% to 44% 3,22,23. Specific causes of recurrent cholangitis after definitive cyst excision have been postulated by Todani and colleagues 22. In this series, only one of the eight patients with type I cysts who had undergone a primary definitive procedure developed recurrent cholangitis, whereas two further patients with type I cysts suffered recurrent cholangitis after cystduodenostomy. Of the two patients with type IVa cysts experiencing ongoing problems, one had undergone previous surgery. These overall results compare favourably to the literature, giving a rate of 18% for recurrent cholangitis if the primary definitive procedure is undertaken in a specialist unit.
There are limited data in the literature with regard to recurrent symptomatology following revisional surgery in those who have previously had cyst drainage procedures. The fact that three of the six revision patients had recurrent cholangitis following a definitive procedure suggests that an inadequate previous operation may compromise long-term results.
In this series, 40% of postoperative cholangitis was caused by the development of an anastomotic stricture, despite this being fashioned at the biliary confluence in accordance with previous recommendations 22,24. These complications appear more frequently in patients who have undergone previous cyst drainage procedures, especially those patients with type IVa cysts 21,25,26. The two patients who required re-operation and anastomotic revision in this series had both had cystduodenostomies performed in childhood. The extensive fibrosis and shortening of the hepatoduodenal ligament noted in both cases has been suggested by other authors to be an independent risk factor for postoperative stenosis and cholangitis 21,22. Two further patients with recurrent cholangitis had type IVa cysts, which are known to promote biliary stasis and stone formation due to intra-hepatic cyst disease, which may not be adequately drained by hepaticojejunostomy 21,25,26,27. Intra-hepatic calculi were identified in both these patients.
The aetiology of choledochal cysts remains somewhat elusive. One aetiological factor may be the reflux of pancreatic juice into the common bile duct (CBD), possibly due to the presence of an anomalous pancreatobiliary junction (APBJ), which is frequently associated with choledochal cysts 28,29,30. It is hypothesised that this anomaly leads to weakening of the duct wall and causes inflammatory changes within the endothelium 31, although an experimental model failed to confirm this finding 32. This theory also seems to be refuted by the case report of a choledochal cyst diagnosed at 15 weeks in utero, i.e. before the exocrine function of the pancreas had even begun 33. However, the strong association of an APBJ with choledochal cysts cannot be ignored 34; 63% of our patients had APBJ either diagnosed by preoperative cholangiography or intra-operatively. Reports of the observed incidence of this abnormality vary from as low as 44% in adult patients 35 to nearly 100% in some paediatric populations 36. The high association with APBJ in children emphasises the potential association, but the lesser frequency with which it is observed in adults suggests other aetiological factors in this patient group. The other anomalies identified at operation or during investigation were also strongly associated with choledochal cyst 14.
We observed no malignancy in this group of patients, yet the incidence in the Asian literature ranges from 8% to 19% 11,12,24, with similar figures in some Western series 3,7. The median age of our patients was 23 years (mean 27 years), which is lower than the mean age of approximately 45 years in other reports 11,37 and may explain why cholangiocarcinoma was not encountered.
There are many reports of malignancy in patients previously treated by cyst drainage procedures 9,11,17, and there is growing evidence that these patients may be at an increased risk of developing malignancy 3,12,20,28, presenting 15 years earlier than those who have had no procedure 37. This phenomenon may be due to reflux of gut bacteria and enzymes into the bile ducts via the enteric anastomosis. These reports emphasise the importance of avoiding cyst drainage procedures and of undertaking complete choledochal cyst excision. Revisional surgery should include definitive cyst excision with a Roux-en-Y hepaticojejunostomy to reduce the likelihood of malignancy. Interestingly, the risk of malignancy in those patients with type IVa cysts is negligible following complete extrahepatic ductal excision with Roux-en-Y hepaticojejunostomy, even though the intrahepatic disease remains in situ, while this figure approaches 45% in patients if no treatment is undertaken 38.
The management of choledochal cysts in adult surgical units is being increasingly reported. The high rate of cholangitis and need for revisional surgery that we and others have reported emphasises that these cases are best managed in specialised tertiary surgical units 22,23,39.
References
- 1.Lipsett PA, Pitt HA, Colombani PM, Boitnott JK, Cameron JL. Choledochal cyst disease. A changing pattern of presentation. Ann Surg. 1994;220:644–52. doi: 10.1097/00000658-199411000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Suita S, Shono K, Kinugasa Y, Kubota M, Matsuo S. Influence of age on the presentation and outcome of choledochal cyst. J Pediatr Surg. 1999;34:1765–8. doi: 10.1016/s0022-3468(99)90308-1. [DOI] [PubMed] [Google Scholar]
- 3.Lenriot JP, Gigot JF, Segol P, Fagniez PL, Fingerhut A, Adloff M. Bile duct cysts in adults: a multi-institutional retrospective study. French Associations for Surgical Research. Ann Surg. 1998;228:159–66. doi: 10.1097/00000658-199808000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chen HM, Jan YY, Chen MF, et al. Surgical treatment of choledochal cyst in adults: results and long-term follow-up. Hepatogastroenterology. 1996;43:1492–9. [PubMed] [Google Scholar]
- 5.Powell CS, Sawyers JL, Reynolds VH. Management of adult choledochal cysts. Ann Surg. 1981;193:666–76. doi: 10.1097/00000658-198105000-00018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kasai M, Asakura Y, Taira Y. Surgical treatment of choledochal cyst. Ann Surg. 1970;172:844–51. doi: 10.1097/00000658-197011000-00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hewitt PM, Krige JE, Bornman PC, Terblanche J. Choledochal cysts in adults. Br J Surg. 1995;82:382–5. doi: 10.1002/bjs.1800820333. [DOI] [PubMed] [Google Scholar]
- 8.Voyles CR, Smadja C, Shands WC, Blumgart LH. Carcinoma in choledochal cysts. Age-related incidence. Arch Surg. 1983;118:986–8. doi: 10.1001/archsurg.1983.01390080088022. [DOI] [PubMed] [Google Scholar]
- 9.Jan YY, Chen HM, Chen MF. Malignancy in choledochal cysts. Hepatogastroenterology. 2000;47:337–40. [PubMed] [Google Scholar]
- 10.Bismuth H, Krissat J. Choledochal cystic malignancies. Ann Oncol. 1999;10(Suppl 4):94–8. [PubMed] [Google Scholar]
- 11.Komi N, Tamura T, Miyoshi Y, Kunitomo K, Udaka H, Takehara H. Nationwide survey of cases of choledochal cyst. Analysis of coexistent anomalies, complications and surgical treatment in 645 cases. Surgery and Gastroenterology. 1984;3:69–73. [PubMed] [Google Scholar]
- 12.Todani T, Watanabe Y, Toki A, Urushihara N. Carcinoma related to choledochal cysts with internal drainage operations. Surg Gynecol Obstet. 1987;164:61–4. [PubMed] [Google Scholar]
- 13.Chijiiwa K, Tanaka M. Late complications after excisional operation in patients with choledochal cyst. J Am Coll Surg. 1994;179:139–44. [PubMed] [Google Scholar]
- 14.Schier F, Clausen M, Kouki M, Gdanietz K, Waldschmidt J. Late results in the management of choledochal cysts. Eur J Pediatr Surg. 1994;4:141–4. doi: 10.1055/s-2008-1066088. [DOI] [PubMed] [Google Scholar]
- 15.Chaudhary A, Dhar P, Sachdev A. Reoperative surgery for choledochal cysts. Br J Surg. 1997;84:781–4. [PubMed] [Google Scholar]
- 16.Swisher SG, Cates JA, Hunt KK, et al. Pancreatitis associated with adult choledochal cysts. Pancreas. 1994;9:633–7. [PubMed] [Google Scholar]
- 17.Yoshikane H, Hashimoto S, Hidano H, et al. Multiple early bile duct carcinoma associated with congenital choledochal cyst. J Gastroenterol. 1998;33:454–7. doi: 10.1007/s005350050113. [DOI] [PubMed] [Google Scholar]
- 18.Flanigan DP. Biliary cysts. Ann Surg. 1975;182:635–43. doi: 10.1097/00000658-197511000-00017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nagorney DM, McIlrath DC, Adson MA. Choledochalcysts in adults: clinical management. Surgery. 1984;96:656–63. [PubMed] [Google Scholar]
- 20.Yamaguchi M. Congenital choledochal cyst. Analysis of 1433 patients in the Japanese literature. Am J Surg. 1980;140:653–7. doi: 10.1016/0002-9610(80)90051-3. [DOI] [PubMed] [Google Scholar]
- 21.Yamataka A, Ohshiro K, Okada Y, et al. Complications after cyst excision with hepaticoenterostomy for choledochal cysts and their surgical management in children versus adults. J Pediatr Surg. 1997;32:1097–102. doi: 10.1016/s0022-3468(97)90407-3. [DOI] [PubMed] [Google Scholar]
- 22.Todani T, Watanabe Y, Urushihara N, Noda T, Morotomi Y. Biliary complications after excisional procedure for choledochal cyst. J Pediatr Surg. 1995;30:478–81. doi: 10.1016/0022-3468(95)90060-8. [DOI] [PubMed] [Google Scholar]
- 23.Saing H, Han H, Chan KL, et al. Early and late results of excision of choledochal cysts. J Pediatr Surg. 1997;32:1563–6. doi: 10.1016/s0022-3468(97)90453-x. [DOI] [PubMed] [Google Scholar]
- 24.Ishibashi T, Kasahara K, Yasuda Y, Nagai H, Makino S, Kanazawa K. Malignant change in the biliary tract after excision of choledochal cyst. Br J Surg. 1997;84:1687–91. [PubMed] [Google Scholar]
- 25.Uno K, Tsuchida Y, Kawarasaki H, Ohmiya H, Honna T. Development of intrahepatic cholelithiasis long after primary excision of choledochal cysts. J Am Coll Surg. 1996;183:583–8. [PubMed] [Google Scholar]
- 26.Cetta F, Montalto G, Nuzzo G. Recurrent hepatolithiasis after primary excision of choledochal cysts. J Am Coll Surg. 1997;185:198–200. doi: 10.1016/s1072-7515(01)00784-0. [DOI] [PubMed] [Google Scholar]
- 27.Chijiiwa K, Komura M, Kameoka N. Postoperative follow-up of patients with type IVA choledochal cysts after excision of extrahepatic cyst. J Am Coll Surg. 1994;179:641–5. [PubMed] [Google Scholar]
- 28.Akkiz H, Colakoglu SO, Ergun Y, et al. Endoscopic retro grade cholangiopancreatography in the diagnosis and management of choledochal cysts. HPB Surgery 1997;10:211–18; discussion 218–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wiedmeyer DA, Stewart ET, Dodds WJ, Geenen JE, Vennes JA, Taylor AJ. Choledochal cyst: findings on cholangiopancreatography with emphasis on ectasia of the common channel. Am J Roentgenol. 1989;153:969–72. doi: 10.2214/ajr.153.5.969. [DOI] [PubMed] [Google Scholar]
- 30.Rattner DW, Schapiro RH, Warshaw AL. Abnormalities of the pancreatic and biliary ducts in adult patients with choledochal cysts. Arch Surg. 1983;118:1068–73. doi: 10.1001/archsurg.1983.01390090052012. [DOI] [PubMed] [Google Scholar]
- 31.Watanatittan S NR. Choledochal cyst: review of 74 paediatric cases. J Med Assoc Thai. 1998;81:856–95. [PubMed] [Google Scholar]
- 32.Benhidjeb T, Said S, Rudolph B, Siegmund E. Anomalous pancreatico-biliary junction – report of a new experimental model and review of the literature. J Pediatr Surg. 1996;31:1670–4. doi: 10.1016/s0022-3468(96)90045-7. [DOI] [PubMed] [Google Scholar]
- 33.Schroeder D, Smith L, Prain C. Antenatal diagnosis of choledochal cyst at 15 weeks gestation: etiologic implications and management. J Pediatr Surg. 1989;24:936–8. doi: 10.1016/s0022-3468(89)80600-1. [DOI] [PubMed] [Google Scholar]
- 34.Sugiyama M, Atomi Y, Kuroda A. Pancreatic disorders associated with anomalous pancreaticobiliary junction. Surgery. 1999;126:492–7. [PubMed] [Google Scholar]
- 35.Chaudhary A, Dhar P, Sachdev A, et al. Choledochal cysts – differences in children and adults. Br J Surg. 1996;83:186–8. [PubMed] [Google Scholar]
- 36.Todani T, Watanabe Y, Narusue M, Tabuchi K, Okajima K. Congenital bile duct cysts: classification, operative procedures, and review of thirty-seven cases including cancer arising from choledochal cyst. Am J Surg. 1977;134:263–9. doi: 10.1016/0002-9610(77)90359-2. [DOI] [PubMed] [Google Scholar]
- 37.Miyoshi Y, Hino M, Takusyoku S. Biliary carcinoma with pancreatobiliary ductal malunion. Proceedings of the Japanese Biliary Disease Association. 1984;20:312–13. [Google Scholar]
- 38.Kagawa Y, Kashihara S, Kuramoto S, Maetani S. Carcinoma arising in a congenitally dilated biliary tract. Report of a case and review of the literature. Gastroenterology. 1978;74:1286–94. [PubMed] [Google Scholar]
- 39.Watanabe Y, Toki A, Todani T. Bile duct cancer developed after cyst excision for choledochal cyst. Journal of Hepatobiliary and Pancreatic Surgery. 1999;6:207–12. doi: 10.1007/s005340050108. [DOI] [PubMed] [Google Scholar]