Abstract
Background
Hepatocellular carcinoma (HCC) is rare in pregnancy but can enlarge rapidly under these circumstances.
Case outline
A 25-year-old woman was diagnosed with HCC of fibrolamellar type immediately post-partum. One year after liver resection the patient remains well.
Discussion
This is only the second report of fibrolamellar carcinoma occurring in pregnancy. Other types of hepatocellular carcinoma in pregnancy have generally demonstrated a poor outcome, probably secondary to hormonal changes and increased liver vascularity.
Keywords: Hepatocellular carcinoma, fibrolamellar variant, pregnancy, treatment
Introduction
Hepatocellular carcinoma (HCC) is rare in females of reproductive age, accounting for only 2.3% of cases in Hong Kong 1. HCC during pregnancy is even rarer with only 32 reports in the medical literature 1,2,3,4,5. Fibrolamellar HCC (FLHCC), a distinct histopathological subtype associated with a better prognosis, has only been described once during pregnancy 6. Here we report the second such case, which resulted in a favourable maternal and fetal outcome.
Case report
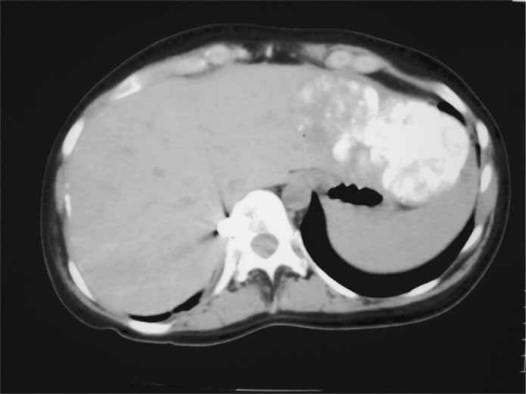
A 25-year-old Caucasian woman (gravida 1, para 1) presented with a painful epigastric mass 1 day after normal vaginal delivery of a 3.8-kg term infant. She had experienced abdominal discomfort for about 2 weeks before delivery. Four days post-partum, she underwent operation for the epigastric mass, which was thought to be a hernia. A transverse incision was made in the epigastrium, and a large tumour measuring 10 cm in diameter was found arising from the left lobe of the liver. There was no evidence of cirrhosis. An incision biopsy of the tumour was taken, the histology of which later showed HCC of fibrolamellar type. The patient was then transferred to this unit. Subsequent blood tests revealed a mildly elevated alpha-fetoprotein (AFP) of 40.5 IU/ml (consistent with 1 week post-partum) and other tumour markers (CEA, Ca 125, Ca 19.9) were within the normal range. Serology for hepatitis B and C was also negative. No metastases were detected on a bone scan or computed tomography (CT) of the chest, and unifocal disease was established with a Lipiodol-enhanced CT (Figure 1).
Figure 1. .
Upiodol-enhanced CT scan showing a solitary tumour in the left lateral segment of the liver (arrow).
Two weeks post-partum, a left lateral segmentectomy (segments II and III) was performed (with excision of the old wound site). Intraoperative ultrasound scan and palpation revealed no other lesions in the liver. Omentum attached to the previous biopsy site in the liver was also excised, with subsequent histology showing no evidence of malignancy. The postoperative course was uneventful, and the patient was discharged after 4 days. Serum AFP normalised within 5 weeks (4.0 IU/ml). A repeat abdominal CT scan 12 months after liver resection showed no recurrence of malignancy, and both mother and infant remain well.
Discussion
HCC is a common malignancy in the Far East but is uncommon in Western countries. It is often extremely aggressive in nature, with a median survival of only 8 weeks for inoperable symptomatic patients 7. The serum AFP is usually markedly elevated, white hepatitis B carrier status is variable, with up to 90% positive serology in some series 8. Cirrhosis is also a common finding in HCC patients.
Documented cases of HCC in pregnancy have been associated with poor maternal and fetal outcome. In Lau et al.'s analysis of 28 patients, only two survived up to 1 year from diagnosis and live infants were delivered in just over half the cases 1. The median survival of this patient group was considerably shorter than that observed in non-pregnant patients with inoperable HCC.
Increased levels of oestrogen and increased liver vascularity have been implicated in the abrupt progression of HCC during pregnancy 1,3,4. Jeng and co-workers have suggested monthly maternal serum AFP measurements once a hepatitis- B carrier is known to be pregnant instead of routine screening at 16 weeks gestation 3. Such a high index of suspicion may allow earlier detection and treatment of HCC.
FLHCC, a less aggressive variant of HCC, has certain distinct clinicopathological features which pose diagnostic dilemmas in pregnancy. Most cases occur in patients under the age of 25 years and are associated with a normal or modestly raised serum AFP level, negative hepatitis serology and normal liver parenchyma. FLHCC may also mimic benign neoplasms of the liver such as adenoma or focal nodular hyperplasia, which are not infrequently seen during pregnancy 9. However, pregnancy may not affect the fibrolamellar variant in the same deleterious manner as it does other types of HCC. The only previously reported case was of a 22-year-old woman who was diagnosed with FLHCC on fine-needle aspiration 2 months before conception. The patient refused intervention, delivered a term infant and was still well 6 months post-partum 6, although abdominal CT scan did show a marked increase in the size of the tumour.
In the case of successful resection of FLHCC occurring during pregnancy, the question of future pregnancies may arise. The possible adverse effects should lead to careful consideration of the risks involved, although Gemer et al., report a case of successful term delivery in a 22-year-old woman in whom a FLHCC had been resected 3 years earlier 10. Successful confinement and delivery have also been reported after resection of non-fibrolamellar HCC 4. On the basis of these anecdotal reports, patients are probably not compromised by further pregnancies if there is no evidence of recurrent disease.
In our patient, erroneous diagnosis of an epigastric hernia at the referring hospital led to an unexpected intraoperative finding of a hepatic tumour, and incision biopsy may have adversely affected the patient's prognosis. In this situation we would advise adequate radiological imaging and referral to a specialist liver unit rather than biopsy or attempted resection by an inexperienced operator. This case also highlights some of the diagnostic difficulties surrounding a focal hepatic mass in pregnancy. Correct diagnosis of FLHCC and appropriate surgical intervention in a specialised centre can lead to a favourable outcome.
References
- 1.Lau WY, Leung WT, Ho S, et al. Hepatocellular carcinoma during pregnancy and its comparison with other pregnancy-associated malignancies. Cancer. 1995;75:2669–76. doi: 10.1002/1097-0142(19950601)75:11<2669::aid-cncr2820751105>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- 2.Brucker C, Weiss M, Schweiberer L, Genz T, Maasen V, Debus-Thiede G. Hepatocellular carcinoma in pregnancy.] [German] Geburtshilfe Frauenheilkd. 1994;54:305–7. doi: 10.1055/s-2007-1022845. [DOI] [PubMed] [Google Scholar]
- 3.Jeny LB, Lee W, Wang C, Chen M, Hsieh T. Hepatocellular carcinoma in a pregnant woman detected by routine screening of maternal a-fetoprotein. Am J Obstet Gynecol. 1995;172:219–20. doi: 10.1016/0002-9378(95)90121-3. [DOI] [PubMed] [Google Scholar]
- 4.Hsieh T, Hou H, Hsu J, Hsieh C, Jeng LB. Term delivery after hepatocellular carcinoma resection in previous pregnancy. Acta Obstet Gynecol Scand. 1996;75:77–8. doi: 10.3109/00016349609033290. [DOI] [PubMed] [Google Scholar]
- 5.Entezami M, Becker R, Ebert A, Pritze W, Weitzel H. Hepatocellular carcinoma as a rare cause of an excessive increase in alpha-fetoprotein during pregnancy. Gynecol Oncol. 1996;62:405–7. doi: 10.1006/gyno.1996.0257. [DOI] [PubMed] [Google Scholar]
- 6.Kroll D, Mazor M, Zirkin H, Schulman H, Glezerman M. Fibrolamellar carcinoma of the liver in pregnancy: a case report. J Reprod Med. 1991;36:823–7. [PubMed] [Google Scholar]
- 7.Shiu W, Dewar G, Leung N, et al. Hepatocellular carcinoma in Hong Kong: clinical study on 340 cases. Oncology. 1990;476:241–5. doi: 10.1159/000226823. [DOI] [PubMed] [Google Scholar]
- 8.Johnson PJ, Krasner N, Portmann B, Eddleston ALWF, Williams R. Hepatocellular carcinoma in Great Britain: influence of age, sex HbsAg status and aetiology of underlying cirrhosis. Gut. 1978;19:1022–6. doi: 10.1136/gut.19.11.1022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Scott LD, Katz AR, Duke JH, Cowan DF, Maklad NF. Oral contraceptives, pregnancy, and focal nodular hyperplasia of the liver. JAMA. 1984;251:1461–3. [PubMed] [Google Scholar]
- 10.Germer O, Segal S, Zohav E. Pregnancy in a patient with fibrolamellar hepatocellular carcinoma. Arch Gynecol Obstet. 1994;225:211–12. doi: 10.1007/BF02335087. [DOI] [PubMed] [Google Scholar]