Abstract
Background
Haemoperitoneum secondary to non-traumatic liver rupture is a rare but potentially fatal condition. It may result from several neoplastic and non-neoplastic diseases such as primary benign or malignant tumours, peliosis hepatis, polyarteritis nodosa, systemic lupus erythematosus, pre-eclampsia and metastatic carcinoma.
Case outlines
Three cases of spontaneous haemoperitoneum caused by rupture of hepatocellular carcinoma are described. All three patients (two men, one woman) had cirrhotic livers, and all were submitted to an urgent operation.One patient re-bled on a second occasion. Emergency operation was undertaken four times in three patients and was successful on all but one occasion.
Discussion
The prognosis for patients with haemoperitoneum is generally poor. Although this condition is relatively frequent in some regions of Asia and Africa, it has rarely been reported in Western countries.The present experience shows that emergency laparotomy can be life-saving.
Keywords: haemoperitoneum, liver neoplasm, spontaneous liver rupture
Introduction
Haemoperitoneum secondary to non-traumatic liver rupture is a rare but potentially fatal condition. It can be caused by a number of different neoplastic and non-neoplastic diseases, including primary benign or malignant tumours of the liver 1,2,3,4,5, peliosis hepatis 6,7, polyarteritis nodosa 8, systemic lupus erythematosus 9, pre-eclampsia 10,11 and metastatic carcinoma. We report three patients with this catastrophic complication of hepatocellular carcinoma (HCC), one of whom had a second bleed.
Case Outlines
Case 1
A 69-year-old white man with a history of alcohol abuse was admitted in October 1993 with acute right upper quadrant abdominal pain and signs of hypovolaemia. On examination, he was pale, dehydrated, with a tense and distended abdomen but no signs of external bleeding; blood pressure was 110/60 mmHg and heart rate 96 bpm. Routine laboratory tests were as follows: haematocrit (Ht) 28%, haemoglobin (Hb) 9.3 g/dl, prothrombin time (PT) 80%. There was no history of trauma. He was admitted to the intensive care unit (ICU) and submitted to abdominal ultrasonography, which revealed free peritoneal fluid. Diagnostic paracentesis revealed blood in the right paracolic gutter. After transfusion of four units of red cell concentrate and haemodynamic stabilisation, a laparotomy was performed. It revealed a 3-litre haemoperitoneum and a 5 cm diameter liver tumour which was ulcerated and haemorrhagic. The tumour occupied segments VII and VIII and adhered to the diaphragm. Two similar expansive lesions were observed on the left side of the liver. The liver was cirrhotic and enlarged. The tumour was partially resected after being detached from the diaphragm (bisegmentectomy of segments VII and VIII). The parenchyma was then sutured with 3–0 silk sutures. On the 8th postoperative day, the patient developed high fever (39°C) and diffuse abdominal pain. Antibiotics were immediately started (ampicillin + gentamicin), and he improved within 24 hours. He was discharged 25 days postoperatively in fair general health. Histology revealed HCC and cirrhosis.
Case 2
A 66-year-old black man with a history of alcoholism and liver cirrhosis presented as an emergency in October 1994 with abdominal distension and hypotension. There was no history of trauma. The haematocrit was 22%, and he had signs of hypovolaemia. Resuscitation was started with blood volume replacement. After haemodynamic stabilisation, the patient was submitted to abdominal ultrasonography and CT scan, which showed a tumour on the right side of the liver and free peritoneal fluid (Figure 1). Diagnostic paracentesis revealed blood in the right paracolic gutter. On the next day, he was submitted to elective right trisegmentectomy. Histopathological examination confirmed the presence of HCC and cirrhosis (Figure 2). On postoperative day 23, a subphrenic abscess was drained. The patient was discharged on day 36 in good general health.
Figure 1. .
Case 1. CT scan showing large mass in the right liver with free fluid in the right subphrenic space.
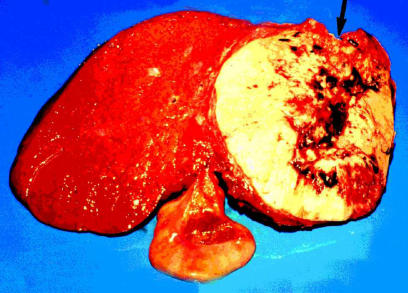
Figure 2. .
Case 2. Section of right hemiliver plus segment IV showing an ulcerated tumour with haemorrhagic areas. The arrow shows the point of rupture in the tumour.
After 16 months, he returned to the emergency room with diffuse abdominal pain but again no history of trauma and no external bleeding. Physical examination revealed signs of anaemia and hypovolaemia, with signs of chronic liver disease and a tense abdomen. Laboratory tests were as follows: Hb 8.9 g/dl, Ht 26.3%, PT 48%. Abdominal ultrasonography suggested the presence of an encapsulated haematoma in the right subphrenic space. CT showed signs of previous liver resection; the left side of the liver was enlarged and contained a heterogeneous lesion which was neoplastic. There was free fluid around the spleen and probably around the left hepatic lobe. The patient was submitted to laparotomy, which revealed a haematoma in the remaining left liver with a metastatic lesion in segment II; the bleeding site had been sealed off by the omentum. Ultrasound-guided liver biopsy revealed diffuse hepatocarcinoma metastases on the left side of the liver. The patient recovered well and was discharged 13 days postoperatively. Eighteen months later, he died of liver failure secondary to extensive carcinoma.
Case 3
A 48-year-old white woman with a previous history of viral hepatitis C and cirrhosis presented in June 1995 with pain, abdominal distension and hypovolaemic shock. There was no history of injury. After resuscitation in the ICU, she was submitted to diagnostic ultrasonography, which revealed a large amount of intra-abdominal fluid and a lesion in the right hepatic lobe. Diagnostic paracentesis showed blood in the peritoneal cavity. Because of haemodynamic instability in spite of generous blood and fluid resuscitation, emergency laparotomy was performed. There was an ulcerated bleeding lesion about 10 cm in diameter in the right hepatic lobe. Right hepatectomy was performed with partial vascular exclusion of the liver. In the immediate postoperative period, she developed hypovolaemic shock with external bleeding through the abdominal drain and died as a consequence.
Discussion
In some parts of Asia and Africa, over 10% of HCC patients present as acute abdominal catastrophes due to rupture of the tumour 3,12. However, in Western countries, haemoperitoneum due to spontaneous rupture of HCC is a rare event 5,6. Physicians should always consider trauma as a possible cause of haemoperitoneum, regardless of the absence of any sign of external damage 13.
Massive abdominal bleeding has also been associated with other abdominal sites besides the liver 13,14, including the spleen, intestine (secondary to the rupture of a metastatic tumour or leiomyosarcoma) and ovary. In HCC cases, the clinical findings often include a history of malignancy and/or chronic liver disease. The patients usually present with severe abdominal pain and massive haemoperitoneum 4,15. Hepatic enzymes may be elevated 15. Although red cell Tc-99m scintigraphy 16 and CT can help to identify the source of intra-abdominal bleeding 5,17,18, these occult malignancies are usually diagnosed during operation 13 or at autopsy 15,19,20.
The mechanism of hepatic rupture and bleeding may be attributed to several factors. Both primary and metastatic tumours can be highly vascular and necrotic 13,15,19 and therefore prone to intraperitoneal rupture. Factors that contribute to bleeding may include increased intravascular pressure secondary to tumour embolus 20, causing intra-hepatic venous obstruction with shunting of blood 19,21, and a hyperaemic liver circulation 22 caused by proximity of vessels to metastatic nodules or primary tumours. However, direct pressure of the tumour against the capsular surface of the liver seems the most plausible explanation 13. Extensive replacement of liver tissue by tumour 15,19 together with poor nutrition may reduce coagulation factors and promote haemorrhage 19.
Systemic chemotherapy can lead to considerable tumour necrosis as well as thrombocytopenia 19. A sudden increase in intra-abdominal pressure resulting from sneezing, coughing or vomiting may cause rupture of tumours that are necrotic or hyper-vascular 19,21. Minor trauma or iatrogenic damage by needle biopsy or liver palpation should be ruled out before the rupture and haemoperitoneum are classified as spontaneous 13.
There is some controversy regarding the treatment of choice in this situation. Bleeding is often difficult to control, and the mortality rate is high 5. The available treatment options are merely palliative 13 unless resection is possible. Surgical treatment includes hepatic wedge resection or lobectomy, ligation of the bleeding source and hepatic artery ligation 5,23,24. Several authors advocate an aggressive surgical intervention 2,3,24,25 with resection of the affected liver lobe whenever possible 25. Unfortunately, only a few patients are suited for this procedure, owing to the presence of cirrhosis or extensive replacement of liver tissue by tumour 4,26. Hepatic ligation may stop the bleeding, but it is associated with a high risk of death from liver failure 24.
Transcatheter arterial embolisation is a therapeutic alternative to operation that has been used to control the bleeding resulting from hepatic metastases 27 or rupture of an HCC 4. After superselective catheterisation of the feeding artery to the tumour, a mixture of gelfoam and mitomycin C is injected. Steel coils are used in patients with a shunt between the hepatic artery and the portal vein 4. The advocates of this method state that the advantage of embolisation over operation (especially in high risk patients) is that it allows later treatment of the neoplastic disease. Operation should only be carried out when hepatic resection is feasible or when embolisation fails to control the bleeding. In addition, therapeutic embolisation decreases mortality rate and hospitalisation time 4. However, a radiologist with the necessary expertise may not always be available 26. Intratumoural injection of absolute alcohol has also been used to treat haemoperitoneum secondary to non-traumatic liver rupture 26, based on the ability of this substance to destroy HCC under ultrasonographic control 28 and to stop the bleeding in oesophageal varices and peptic ulcers 29. Bleeding stops owing to a process of tissue dehydration and fixation, followed by thrombosis of the vessel 26. This procedure is inexpensive and may be performed in any operating theatre. It may be useful when resection or hepatic ligation are either not possible or ineffective, and when transcatheter embolisation is not available 26.
The documented survival of patients with non-traumatic haemoperitoneum is low 23, and the prognosis of patients with spontaneous rupture of hepatomas is extremely poor 5,13,15. The outcome is determined by the stage of both the neoplastic and the underlying liver disease, the rapidity of diagnosis, the degree of haemorrhage and the type of therapy 4.
References
- 1.Bird D, Vowles K, Anthony PP. Spontaneous rupture of a liver cell adenoma after long term methyltestosterone: Report of a case successfully treated by emergency right hepatic lobectomy. Br J Surg. 1979;66:212–3. doi: 10.1002/bjs.1800660324. [DOI] [PubMed] [Google Scholar]
- 2.Mokka R, Seppala A, Huttunen R, et al. Spontaneous rupture of liver tumors. Br J Surg. 1976;63:715–7. doi: 10.1002/bjs.1800630911. [DOI] [PubMed] [Google Scholar]
- 3.Nagasue N, Inokushi K. Spontaneous and traumatic rupture of hepatoma. Br J Surg. 1979;66:248–50. doi: 10.1002/bjs.1800660409. [DOI] [PubMed] [Google Scholar]
- 4.Hsieh JS, Huang CJ, Huang YS, et al. Intraperitoneal hemorrhage due to spontaneous rupture of hepatocellular carcinoma: treatment by hepatic artery embolization. AJR Am J Roentgenol. 1987;149:715–7. doi: 10.2214/ajr.149.4.715. [DOI] [PubMed] [Google Scholar]
- 5.Pombo F, Arrojo L, Perez-Fontan J. Haemoperitoneum secondary to spontaneous rupture of hepatocellular carcinoma: CT diagnosis. Clin Radiol. 1991;43:321–2. doi: 10.1016/s0009-9260(05)80539-2. [DOI] [PubMed] [Google Scholar]
- 6.Baer PA, Meagher T, Pal JM, Viloria J. Severe weight loss and fatal intra-abdominal hemorrhage in an elderly man. Can Med Assoc J. 1984;131:319–24. [PMC free article] [PubMed] [Google Scholar]
- 7.Smathers RL, Heiken JP, Lee JKT, et al. Computed tomography of fatal hepatic rupture due to peliosis hepatis. J Comput Assist Tomogr. 1984;8:768–9. doi: 10.1097/00004728-198408000-00035. [DOI] [PubMed] [Google Scholar]
- 8.Li AKC, Rhodes JM, Valentino AR. Spontaneous liver rupture in polyarteritis nodosa. Br J Surg. 1979;66:251–2. doi: 10.1002/bjs.1800660410. [DOI] [PubMed] [Google Scholar]
- 9.Levitin PM, Sweet D, Brunner CM, et al. Spontaneous rupture of the liver. Arthritis Rheum. 1977;20:748–50. doi: 10.1002/art.1780200217. [DOI] [PubMed] [Google Scholar]
- 10.Aziz S, Merrel RC, Collins JA. Spontaneous hepatic hemorrhage during pregnancy. Am J Surg. 1983;146:680–2. doi: 10.1016/0002-9610(83)90311-2. [DOI] [PubMed] [Google Scholar]
- 11.Winer-Muran HT, Muran D, Salagan J, Massie JD. Hepatic rupture in preeclampsia: The role of diagnostic imagery. J Can Assoc Radiol. 1985;36:34–6. [PubMed] [Google Scholar]
- 12.Kew MC, Geddes EW. Hepatocellular carcinoma in rural Southern African blacks. Medicine (Baltimore) 1982;61:98–108. doi: 10.1097/00005792-198203000-00004. [DOI] [PubMed] [Google Scholar]
- 13.Mittleman RE. Hepatic rupture due to metastatic lung carcinoma. Am J Clin Pathol. 1987;88:506–9. doi: 10.1093/ajcp/88.4.506. [DOI] [PubMed] [Google Scholar]
- 14.Margolin KA, Park HY, Esensten ML, Doroshow JH. Hepatic metastases in granulosa cell tumor of the ovary. Cancer. 1985;56:691–5. doi: 10.1002/1097-0142(19850801)56:3<691::aid-cncr2820560342>3.0.co;2-q. [DOI] [PubMed] [Google Scholar]
- 15.Schoedel KE, Dekker A. Hemoperitoneum in the setting of metastatic cancer to the liver. Dig Dis Sci. 1992;37:153–4. doi: 10.1007/BF01308360. [DOI] [PubMed] [Google Scholar]
- 16.Czarnecki DJ. Intraperitoneal hemorrhage diagnosed by technetium-99m labeled RBC imaging. Clin Nucl Med. 1986;11:617–8. doi: 10.1097/00003072-198609000-00003. [DOI] [PubMed] [Google Scholar]
- 17.Cates JD, Thorsen MK, Foley WD, Lawson TL. CT diagnosis of massive hemorrhage from hepatocellular carcinoma. J Comput Assist Tomogr. 1987;11:81–2. doi: 10.1097/00004728-198701000-00015. [DOI] [PubMed] [Google Scholar]
- 18.Siskind BN, Malat J, Hammers L. CT features of hemorrhagic malignant liver tumors. J Comput Assist Tomogr. 1987;11:766–70. doi: 10.1097/00004728-198709000-00004. [DOI] [PubMed] [Google Scholar]
- 19.Fidas-Kamini A, Busuttil A. Fatal haemoperitoneum from ruptured hepatic metastases from testicular teratomas. Br J Urol. 1987;60:80–1. doi: 10.1111/j.1464-410x.1987.tb09143.x. [DOI] [PubMed] [Google Scholar]
- 20.Alavi AH. Massive haemoperitoneum following rupture of hepatoma: Report of three autopsy cases. East Afr Med J. 1985;62:415–9. [PubMed] [Google Scholar]
- 21.Cooperman AM, Weiland LH, Welch JS. Massive bleeding from a ruptured metastatic hepatic melanoma treated by hepatic lobectomy. Mayo Clin Proc. 1976;51:167–70. [PubMed] [Google Scholar]
- 22.Watson CR, Baltaxe HA. The angiographic appearances of primary and secondary tumors of the liver. Radiology. 1971;101:539–48. doi: 10.1148/101.3.539. [DOI] [PubMed] [Google Scholar]
- 23.Urdaneta LF, Nielson JV. Massive hemoperitoneum secondary to spontaneous rupture of hepatic metastases: Report of two cases and review of the literature. J Surg Oncol. 1986;31:104–7. doi: 10.1002/jso.2930310206. [DOI] [PubMed] [Google Scholar]
- 24.Chearanai O, Plengvanit U, Asavanish C, et al. Spontaneous rupture of primary hepatoma: Report of 63 cases with particular reference to the pathogenesis and rationale treatment by hepatic artery ligation. Cancer. 1983;52:1532–6. doi: 10.1002/1097-0142(19830415)51:8<1532::aid-cncr2820510829>3.0.co;2-3. [DOI] [PubMed] [Google Scholar]
- 25.Ong GB, Taw HL. Spontaneous rupture of hepatocellular carcinoma. Br Med J. 1972;4:146–9. doi: 10.1136/bmj.4.5833.146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chung SCS, Lee TW, Kwok SPY, Li AKC. Injection of alcohol to control bleeding from ruptured hepatomas. Br Med J. 1990;301:421. doi: 10.1136/bmj.301.6749.421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hirai K, Kawazoe Y, Yamashita K, et al. Transcatheter arterial embolization for spontaneous rupture of hepatocellular carcinoma. Am J Gastroenterol. 1986;81:275–9. [PubMed] [Google Scholar]
- 28.Di Stasi M, Buscarini L, Livralgi T, et al. Percutaneous ethanol injection in the treatment of hepatocellular carcinoma. A multicenter survey of evaluation practices and complication rates. Scand J Gastroenterol. 1997;32:1168–73. doi: 10.3109/00365529709002998. [DOI] [PubMed] [Google Scholar]
- 29.Sugawa C, Fujita Y, Ikeda T, Walt AJ. Endoscopic hemostasis of bleeding of the upper gastrointestinal tract by local injection of ninety-eight per cent dehydrated ethanol. Surg Gynecol Obstet. 1986;162:159–63. [PubMed] [Google Scholar]