Abstract
Background
In 1995 the concept of a ‘critical view of safety’ (CVS) in Calot's triangle was introduced to prevent bile duct injury in laparoscopic cholecystectomy. The aim of this study was to determine the most reliable method for recording CVS.
Methods
Operation notes, video images and photo prints from 50 consecutive elective non-converted laparoscopic cholecystectomies were analysed.
Results
Operation notes alone did not suffice to record CVS. As an adjunct, video proved superior to photo print with regard to quality. Nevertheless, photo prints were practically and logistically much easier to produce than video. Moreover, when good quality images were achieved, photo print recorded CVS more conclusively than video.
Discussion
Operation notes,video and photo print are complementary, and the combination records CVS conclusively in nearly every case.
Keywords: laparoscopic cholecystectomy, operation notes, documentation, bile duct injury, quality control
Introduction
It was recently calculated that every fifth lawsuit against Dutch general surgeons concerns laparoscopic cholecystectomy (LC) 1. Although everyone agrees on the advantages of LC, its maj or drawback remains the increased risk of bile duct injury (BDI). The reported incidence of BDI varies from 0.20% to 3.40%, with a mean of 0.85% 2. When simple bile leaks and bilomas are excluded, the risk remains at least 0.50%, which is calculated to be 2.5–4-fold greater than that in open cholecystectomy 2. In fact, the true incidence may be much higher, considering that these injuries are subject to under-reporting 2: while an incidence of BDI of 0.86% was found in a national survey, the incidence of bile duct repair was 1.09% over the same period 3. Moreover, late complications such as stenosis due to ischaemia are often not reported 3.
To prevent BDI, Strasberg and colleagues introduced the concept of the ‘critical view of safety’ (CVS). In this technique, the neck of the gallbladder must be dissected off the liver bed (i.e. unfolding Calot's triangle) to achieve conclusive identification of the two structures to be divided: the cystic duct and cystic artery 2. In 1996 we implemented this concept in our department. For quality control purposes, we subsequently videotaped the CVS for each LC. More recently, we purchased a printing device and started photo printing CVS as well (Figure 1). The aim of this study was to determine which technique is superior in documenting CVS. We also investigated the quality of the operation notes and correlated these results with the data from the two imaging techniques.
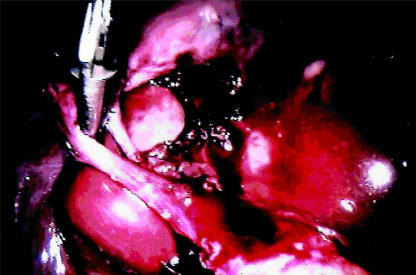
Figure 1. .
Critical view of safety in laparoscopic cholecystectomy as documented on photo print.
Patients and methods
The documentation of CVS was investigated in 50 consecutive elective non-converted LCs. For this purpose non-protocolised operation notes, videotapes (JVC HR-J220E) and photo prints (Sony UP2300P) were studied. Photo prints were taken at three stages during the dissection of Calot's triangle: after creating CVS, after clipping the cystic duct and artery and after dividing these structures. This entire procedure was documented on videotape.
Patient characteristics and indications for LC are depicted in Table 1. The quality of the documenting modality was determined on a semi-quantitative scale (good/moderate/poor). Achieving CVS was judged as being established as follows: conclusively, probably, inconclusively or not at all.
Table 1. Patient characteristics and indications in 50 consecutive laparoscopic cholecystectomies.
| Patient characteristics | |
| Sex | 15 men/35 women |
| Age | 48.7 years (range: 24–77) |
| Mean hospital stay | 2.6 days (range: 1–9) |
| Indications | |
| Biliary colic | 41 |
| Acute cholecystitis | 4 |
| After gallstone pancreatitis | 2 |
| After acute cholecystitis | 1 |
| After obstructive jaundice | 1 |
| Asymptomatic (pre-renal transplantation) | 1 |
Results
Operation notes were available for all 50 patients and adequate establishment of CVS was described in 39 cases (78%). On the videotapes, images were missing for five cases; in each case photo prints were available. The number of prints produced was one each for 19 patients, two each for five patients, three each for 25 and four for one patient; there was a mean of 2.2 photo prints per LC. The quality of the documenting modality and the extent to which CVS was established are depicted in Table 2. When imaging techniques were combined with the operation notes, the fact that CVS had been established could be proved in all but one case. Among the 11 patients in whom the operation notes were not interpretable in this regard, the other information confirmed CVS in eight.
Table 2. Quality and results of the three documenting modalities (%): the results describe the ability of the documenting modality to establish an ad equate’ critical view of safety’.
| Parameter | Operation notes | Videotape | Photo Print |
|---|---|---|---|
| (n = 50) |
(n = 45) |
(n = 50) |
|
| Quality | |||
| good | 50 (100) | 38 (84) | 25 (50) |
| moderate | 0(0) | 6(13) | 22 (44) |
| poor | 0(0) | 1 (2) | 3(6) |
| Results | |||
| conclusive | 39 (78) | 20 (44) | 3 1 (62) |
| probable | 6(12) | 18 (40) | 8(16) |
| inconclusive | 0(0) | 5(12) | 8(16) |
| CVS not established | 0(0) | 2(4) | 3(6) |
Discussion
BDI is a severe complication of biliary surgery because it causes serious morbidity and is potentially lethal 5. Furthermore, BDI has enormous economic consequences; it has been estimated that in the USA alone laparoscopic litigation costs $40–100 million per annum 6. The commonest cause of BDI in LC is misinterpretation of Calot's triangle, i.e. confusing the common bile duct with the cystic duct 3,4. This confusion may be attributed to anatomical risk factors, factors inherent in the laparoscopic technique and inadequate training. Anatomical risk factors may include inflammation, obesity and congenital anomalies. Factors inherent in the laparoscopic technique include lack of depth perception and tactile sensation, two-dimensional sight, the difficulty in performing antegrade cholecystectomy, the use of electrocautery or laser in a limited field that can easily be obscured by blood or bile, and sometimes inadequate instrumentation 7,8,9,10. The report by Strasberg and associates on BDI must be regarded as a milestone 2. Not only did they review 124 433 cases of LC, but they also proposed a simple yet important concept to prevent BDI in LC, i.e. the principle of CVS.
To date, no study has been performed to investigate which technique or combination of techniques is superior in documenting CVS. We compared operation notes with two imaging modalities (i.e. videotape and photo print) to try to resolve this question. Although the operation notes were generally of good quality, they did not describe CVS adequately in all cases, even though all laparoscopic surgeons in our clinic have complied with the principle of CVS since its introduction. Operation notes alone, therefore, do not suffice to document CVS adequately. Second, video imaging proved superior to photo print as an adjunct to the operation notes with regard to quality. However, photo printing was much easier to perform than videotaping, probably because fewer actions are needed and direct results can be achieved. Moreover, photo prints give a better opportunity to correct potential mistakes immediately, which is not the case with videotaping, and storage is much easier. Lastly, documenting CVS conclusively was better with photo printing than with video, given the fact that good quality imaging had been achieved.
We conclude that operation notes and imaging techniques are complementary. In its present form photo printing has some advantages over videotaping, and the prints are kept in the patients’ records. These results have led to the implementation of printing CVS for medicolegal and tutorial purposes in several teaching hospitals in our region.
References
- 1.van den Wildenberg FAJM, Andriesse R, Hamersma AM. Lawsuits against general surgeons [translated title] Ned Tijdschr Heelkd. 2000;9:44–6. [Google Scholar]
- 2.Strasberg SM, Hertl M, Soper NJ. An analysis of the problem of biliary injury during laparoscopic cholecystectomy. J Am Coll Surg. 1995;180:101–25. [PubMed] [Google Scholar]
- 3.de Wit LT, Rauws EAJ, Gouma DJ. Surgical management of iatrogenic bile duct injury. Scand J Gastroenterol. 1999;34(suppl 230):89–94. doi: 10.1080/003655299750025606. [DOI] [PubMed] [Google Scholar]
- 4.Habib E, Elhadad A. A technique for laparoscopic Cholecystectomy: wide opening of Calot's triangle as the first step. HPB Surg. 2000;2:313–15. [Google Scholar]
- 5.Targarona EM, Marco C, Balagué C, et al. How, when, and why bile duct injury occurs: a comparison between open and laparoscopic cholecystectomy. Surg Endosc. 1998;12:322–6. doi: 10.1007/s004649900662. [DOI] [PubMed] [Google Scholar]
- 6.Kern KA. Malpractice litigation involving laparoscopic cholecystectomy: cost, cause and consequences. Arch Surg. 1997;132:392–8. doi: 10.1001/archsurg.1997.01430280066009. [DOI] [PubMed] [Google Scholar]
- 7.Moossa AR, Easter DW, van Sonnenberg E, Casola G, D'Agostino H. Laparoscopic injuries to the bile duct: a cause for concern. Ann Surg. 1992;215:203–8. doi: 10.1097/00000658-199203000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Asbun HJ, Rossi RL, Lowell JA, Munson JL. Bile duct injury during laparoscopic cholecystectomy. World J Surg. 1993;17:547–52. doi: 10.1007/BF01655122. [DOI] [PubMed] [Google Scholar]
- 9.MacFadyen BV, Vecchio R, Ricardo AE, Mathis CR. Bile duct injury after laparoscopic cholecystectomy: the United States experience. Surg Endosc. 1998;12:315–21. doi: 10.1007/s004649900661. [DOI] [PubMed] [Google Scholar]
- 10.Sekimoto M, Tomita N, Tamura S, Ohsato H, Monden M. New retraction technique to allow better visualiztion of Calot's triangle during laparoscopic cholecystectomy. Surg Endosc. 1998;12:1439–41. doi: 10.1007/s004649900877. [DOI] [PubMed] [Google Scholar]