Abstract
Background
Hepatic resection is indicated for a variety of benign conditions because of persistent symptoms, uncertainty regarding the diagnosis or the risk of malignant transformation. The aim of this study was to assess the indications for and outcome of hepatic resection for benign non-cystic liver lesions in a specialist hepatobiliary unit.
Patients and methods
All patients who had undergone hepatic resection for benign non-cystic hepatic lesions between 1989 and 2001 were identified from a prospective database for analysis.
Results
A total of 49 patients (40 women, 9 men) with a mean age of 43 years (range 21–75 years) underwent resection of non-cystic benign lesions. Indications for operation included suspected liver cell adenoma (n=11), suspicion of malignancy (11), persistent symptoms attributable to the lesion (20) or chronic sepsis (7). The final diagnosis was focal nodular hyperplasia (n=12), haemangioma (12), adenoma (8), sclerosing cholangitis (5), inflammatory pseudotumour (4), intrahepatic cholelithiasis (3), chronic hepatic abscess (3), benign biliary fibrosis (I) and leiomyoma (I). Major anatomical hepatic resections were performed in 44 patients, and 5 patients underwent a segmentectomy or minor atypical resection. Median operating time was 215 min (range 45–450 min) and median blood loss was 875 ml (range 200–4000 ml). Ten patients (20%) required a median blood transfusion of 2 units (range 2–8 units). The median postoperative stay was 10 days (range 4–33 days). There were no deaths, but complications occurred in 15 patients (27%).
Conclusions
Hepatic resection can be safely recommended for selected patients with a variety of benign non-cystic hepatic lesions. A small group of patients undergo resection as a result of inability to rule out a malignant process, but the large majority will be operated on because of either their malignant potential or related symptoms.
Keywords: liver cell adenoma, haemangioma, focal nodular hyperplasia, liver resection, liver abscess, pseudotumours, cholangiocarcinoma
Introduction
Benign non-cystic liver lesions include liver cell adenomas, focal nodular hyperplasia (FNH), haemangiomas, chronic abscesses and inflammatory pseudotumours. They may be discovered incidentally or may present with abdominal symptoms. Very rarely a benign liver lesion presents acutely with a complication secondary to haemorrhage or necrosis. These tumours are of interest to clinicians because they can present a diagnostic dilemma in patients referred for operation because of persisting symptoms or a concern about malignancy. Liver resection is a major procedure, so if it is to be undertaken in patients with benign disease it must be associated with low morbidity and mortality rates. The aim of this review was to assess the indications for and outcome of hepatic resection for benign non-cystic liver lesions over a 12-year period in a specialist hepatobiliary unit.
Patients and methods
A prospective database for all liver resections has been maintained in our tertiary referral unit since 1989. Details of all patients undergoing hepatic resection for pathologically proven benign disease between September 1989 and January 2001 were identified from the database for further assessment. Where relevant, inpatient notes were retrieved for review.
Preoperative assessment included a routine abdominal ultrasound and CT scan. CT angio-portography, laparoscopic ultrasound and mesenteric angiography were used selectively. Magnetic resonance imaging (MRI) was not available in our unit during the period of this study. Liver function tests and clotting profiles were checked in all patients, while in selected patients alpha-fetoprotein (AFP) and carcinoembryonic antigen (CEA) levels were also measured.
If a confident diagnosis of FNH or haemangioma was made and the patient was asymptomatic, observation was recommended. Operation was offered for giant haemangiomas (>4 cm diameter) if the lesion increased in size or was symptomatic. If a diagnosis of adenoma was ascertained or could not be excluded, hepatic resection was advocated because of the concern about malignant transformation. Patients with inflammatory lesions underwent resection if a residual mass was identified following percutaneous drainage of infected fluid. The other major indication for operation was persistent suspicion of malignancy.
Results
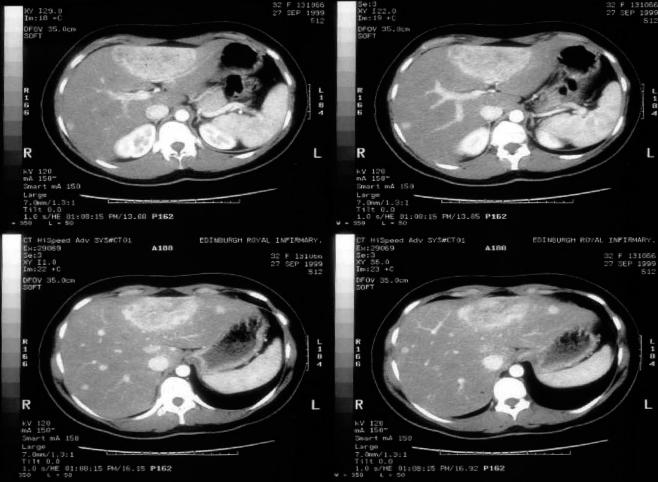
A total of 49 patients (40 women, 9 men) underwent resection of solid benign lesions of the liver between September 1989 and January 2001. The mean age was 43 years (range 21–75 years). Of the 20 patients in whom tumour markers were sought (AFP levels, 9 patients; CEA levels, 11 patients), only one patient with an adenoma had an elevated CEA (156iu/ml: normal <60iu/ml). Most patients had normal liver function tests, but abnormalities were noted in six patients (adenoma 3, FNH 2, inflammatory pseudotumour 1). All patients underwent ultrasonography and abdominal CT scanning (Figure 1). Other imaging techniques were used on a selective basis and included CT angio-portography (n = 22), laparoscopy (23), laparoscopic ultrasound (22) and mesenteric angiography (6). Mesenteric angiography was reserved for patients with a suspected cholangiocarcinoma.
Figure 1. .
CT scan showing the typical appearance of focal nodular hyperplasia (FNH) in the left lobe of the liver.
The principal indications for operation were suspected liver cell adenoma (n = 11), suspicion of malignancy (11), persistent symptoms (20) and chronic sepsis (7). The final diagnosis was FNH (n = 12), haemangioma (12), adenoma (8), sclerosing cholangitis (5), inflammatory pseudotumour (4), intrahepatic cholelithiasis (3), hepatic abscess (3), benign biliary fibrosis (1) and leiomyoma (1).
All but one of the patients with adenoma were symptomatic, the commonest presenting symptom being abdominal pain; one patient presented with a mass. In only one case was the presumed preoperative diagnosis of an adenoma found to be incorrect – the lesion actually being FNH–although in another two cases the preoperative investigations had been unable clearly to distinguish FNH from adenoma. All other patients with FNH had been offered operation because of persistent symptoms. Although all patients with haemangiomas were symptomatic, none presented with acute rupture. In one patient the haemangioma was incorrectly assumed to be a colorectal liver metastasis, and operation was recommended on this basis. Another 10 patients underwent operation because of a concern about malignancy: six patients with hilar masses and biliary strictures suspicious of cholangiocarcinoma, three patients with inflammatory pseudotumours and one patient with a very large intrahepatic mass. This last patient had suffered from progressive abdominal distension and pain for 5 years. A 500-g tumour measuring 20 cm in diameter was resected by right trisectionectomy. Histology demonstrated a leiomyoma with extensive hyalinisation and myxoid degeneration. Seven patients required operation for chronic sepsis, which was precipitated by complicated cholelithiasis in three patients. All were initially treated by percutaneous drainage, biliary decompression and appropriate antibiotic therapy. Non-resolution of hepatic sepsis was the indication for operation in each case.
Resections included right hepatectomy (23), right trisegmentectomy (4), left hepatectomy (15), left trisegmentectomy (2) and segmentectomy/minor atypical resection (5). The median operating time was 215 min (range 45–450 min) and median blood loss was 875 ml (range 200–4000 ml). Ten patients required a median of 2 units blood transfusion (range 2–8 units). The median postoperative stay was 10 days (range 4–33 days). There were no deaths, but complications occurred in 15 patients (27%) as follows: bile leak (n = 3), intra-abdominal collection (3), chest infection (3), haemorrhage (2), portal vein thrombosis (1), duodenal fistula (1), deep venous thrombosis (1), renal failure (1) and urinary tract infection (1). Two patients with bile leaks required endoscopic stenting, while the third leak resolved spontaneously. The duodenal fistula resolved after 2 weeks of total parenteral nutrition.
Discussion
Benign non-cystic hepatic lesions include a variety of conditions. The widespread availability of abdominal ultrasonography means that an increasing number of these lesions are detected and may be referred for surgical assessment. Bismuth urged a degree of caution when he stated that ‘extreme care must be taken to understand the natural history of benign tumours of the liver and to avoid unnecessary surgery’ 1. The safety of resection for benign liver lesions in specialist hepatobiliary units is well established. Iwatsuki et al. reported no deaths from hepatic resections undertaken for a variety of benign hepatic lesions (giant haemangioma 114, liver cell adenoma 25, FNH 23, congenital cysts 23) 2. In the series of Belghiti and colleagues (51 patients), there were no deaths and minor complications in 6 patients 3. Weimann and associates performed liver resection for benign lesions in 173 patients (haemangioma, 69; FNH, 61; liver cell adenoma, 39; mixed tumours, 4) and reported one death due to a consumptive coagulopathy 4. Nagorney and co-workers performed resection for FNH (14) and liver cell adenomas (19) with no mortality 5. Their morbidity included a bile leak and a superficial wound infection. There were no deaths in the present series, but 15 patients (27%) developed a complication.
Liver cell adenomas have a potential for malignant change, and hence resection is indicated. Eleven percent of resected liver cell adenomas may contain foci of hepatocellular carcinoma (HCC) 6. Similarly Belghiti's cohort included three suspected adenomas which contained foci of malignancy (well differentiated HCC, 2; fibrolamellar carcinoma, 1) 3. It is for this reason that operation is advocated for all patients with suspected liver cell adenomas.
Patients with asymptomatic FNH can be observed, as there is no malignant potential. However, the difficulty lies in distinguishing between adenoma and FNH, as both conditions predominantly affect women of reproductive age and they share common radiological features. In our series, FNH was labelled incorrectly as liver cell adenoma preoperatively in one case, and in another two preoperative imaging was unable to distinguish FNH from adenoma. As percutaneous biopsy may result in haemorrhage or pathological misdiagnosis due to the small sample of tissue 2,4, we do not advocate this procedure.
Haemangiomas are benign liver lesions of mesenchymal origin. Cavernous haemangiomas may be large and cause symptoms due to stretching of Glisson's capsule. Most authors reserve operation for symptomatic lesions. Born-man and colleagues resected four symptomatic giant haemangiomas with minimal morbidity and no mortality 7, while Lise and associates operated on 29 of 51 patients with haemangiomas 8. Farges and associates intervened in 14 of 87 patients with haemangioma (resection, 8; embolisation, 5; hepatic artery ligation, 1) 9. In another series of 78 giant haemangiomas 10, 16 symptomatic lesions were resected and 36 participated in a protocol-directed ultrasonography follow-up study. None of the above operative series had any surgical mortality, and none of the observed haemangiomas became symptomatic or developed complications. However, Brouwers and co-workers reported spontaneous rupture in two patients with giant haemangiomas (>4 cm in diameter) 11; this is a rare complication but associated with a high mortality rate. They advocated resection of giant haemangiomas in atypical locations or in the setting of anticoagulant use. We believe that spontaneous rupture is rare and maintain an observational policy for patients with asymptomatic haemangiomas. Operation is reserved for symptomatic haemangiomas or where there is diagnostic doubt.
Attributing symptoms to radiologically detected liver lesions remains problematic. Bismuth described benign liver lesions as the ‘bad side effect’ of diagnostic ultrasound 1. Once a patient has been told of the presence of a lesion, personal anxiety may precipitate or exacerbate underlying symptoms, although these may not always be due to the liver lesion. A small minority of patients can have persistent vague abdominal symptoms such as dull aches up to 15 years after their initial operation 2. In Farges’ series of 87 patients with cavernous haemangiomas who presented with abdominal pain, 47 had a concomitant pathology which could explain their pain 9. Symptoms persisted in seven patients who underwent resection in this group, implying that the haemangioma was not the cause of the symptoms. When assessing these patients, it is imperative that concomitant upper gastrointestinal pathology that could account for the symptoms is excluded.
Pyogenic liver abscess can complicate biliary obstruction and cholangitis or portal pyaemia secondary to diverticular disease 12,13,14. Most of these abscesses are adequately treated by percutaneous drainage, biliary decompression and antibiotic therapy. Hepatic resection is required for a subset of patients with complicated hepatic abscesses. In one series of 23 patients, one patient developed recurrent abscesses despite repeated percutaneous catheter drainage requiring hepatic resection 12. In another series no patients required formal resection, but in the invited commentary, Dr Schwartz stated that his group had experience of five patients with abscesses that required formal hepatectomy after failed percutaneous drainage 13. The factors that make it unlikely that simple drainage will be sufficient include chronicity, multi-loculated cavities, central areas of necrosis, inadequate biliary drainage, intrahepatic stone disease, liver atrophy and location of the abscess in segments II and III.
Inflammatory pseudotumours consist of a central core of necrotic tissue surrounded by overlying chronic inflammatory tissue; they appear as hyperdense lesions on CT scan and hyper- or hypo-echoic lesions on ultrasound 15,16,17. Pyrexia, pain and weight loss are the commonest presenting features, and malignancy is usually considered to be the cause 15. In this report of 53 cases from Schmid and colleagues, less than a quarter (22%) were treated conservatively. Operation included major liver resections (30), wedge resections (5) and liver transplantation (1). In the present series seven patients with either a chronic pyogenic liver abscess or an inflammatory pseudotumour required hepatic resection. Of these, four had not responded to simple drainage and three had suspected malignancy.
A number of benign conditions can present with biliary obstruction and radiological imaging suggestive of cholangiocarcinoma. Confirming a preoperative diagnosis of malignancy remains difficult and may be dangerous as both bleeding and needle tract seeding of malignant cells have been reported following needle aspiration 2,18. Consequently, in a subset of patients resection will be undertaken for what turns out to be benign disease. Observing these patients exposes the patient to the risk of not treating a malignancy. Gerhards and associates reviewed their ability to distinguish benign and malignant biliary strictures at the hepatic hilum on the basis of radiology 19. They undertook hepatic resection in 132 patients for a suspicious lesion at the hepatic hilum. Of these, 20 patients (15%) had benign disease, the diagnosis being chronic fibrosis, erosive inflammation, sclerosing cholangitis or a granular cell tumour. All these patients had clinical and radiological features highly suggestive of cholangiocarcinoma. They concluded that erroneous preoperative diagnosis is to be expected in patients undergoing hepatic resection for suspected cholangiocarcinoma, and this concurs with our own experience in whom six patients were erroneously thought to have cholangiocarcinoma despite extensive investigation. Provided that hepatic resection can be undertaken safely and the patient is counselled appropriately, hepatic resection should still be offered to this group of patients 20.
This report has demonstrated the applicability of hepatic resection in a spectrum of benign liver and proximal biliary conditions. Liver cell adenomas should be resected, as they have a definite malignant potential. Patients with FNH and haemangiomas can be safely observed; however, resection should be considered if there is diagnostic doubt or if the lesion produces significant symptoms. Asymptomatic giant haemangiomas should be observed, as the risk of spontaneous rupture seems to be remote. Most pyogenic liver abscesses will respond to simple drainage, but a subset may require surgery – especially if the collection is multi-loculated, there is a central core of necrotic debris or there remains a suspicion of malignancy. Patients presenting with obstructing biliary strictures may be candidates for resection if malignancy cannot be excluded. A group of patients who pose particular difficulty are those who are known to suffer from primary sclerosing cholangitis. Any exacerbation of their condition could be due to the development of a cholangiocarcinoma and resection at that time may be the most appropriate management strategy. All these patients should be thoroughly investigated in specialist hepatobiliary units and should be considered for liver resection, as surgery can be undertaken with minimal morbidity and mortality.
References
- 1.Bismuth H. World progress in surgery. Benign and malignant tumours of the liver – Introduction. World J Surg. 1995;19:11–12. doi: 10.1007/BF00316972. [DOI] [PubMed] [Google Scholar]
- 2.Iwatsuki S, Todo S, Starzl TE. Excisional therapy for benign hepatic lesions. Surg Gynecol Obstet. 1990;171:240–6. [PMC free article] [PubMed] [Google Scholar]
- 3.Belghiti J, Pateron D, Panis Y, et al. Resection of presumed benign liver tumours. Br J Surg. 1993;80:380–93. doi: 10.1002/bjs.1800800340. [DOI] [PubMed] [Google Scholar]
- 4.Weimann A, Ringe B, Klempnauer J, et al. Benign liver tumours: differential diagnosis and indications for surgery. World J Surg. 1997;21:983–91. doi: 10.1007/s002689900337. [DOI] [PubMed] [Google Scholar]
- 5.Nagorney DM. Benign hepatic tumours: focal nodular hyperplasia and hepatocellular adenoma. World J Surg. 1995;19:13–18. doi: 10.1007/BF00316973. [DOI] [PubMed] [Google Scholar]
- 6.Kerlin P, Davis GL, McGill DB, Weiland LH, Adson MA, Sheedy PF. Hepatic adenoma and focal nodular hyperplasia: clinical, pathologic, and radiologic features. Gastroenterobgy. 1983;84:994–1002. [PubMed] [Google Scholar]
- 7.Bornman PC, Terblanche J, Blumgart RL, Harries Jones EP, Kalvaria I. Giant hepatic haemangiomas: diagnostic and therapeutic dilemmas. Surgery. 1987;101:445–8. [PubMed] [Google Scholar]
- 8.Lise M, Feltrin G, Da Pian PP, et al. Giant cavernous haemangiomas: diagnosis and surgical strategies. World J Surg. 1992;16:516–20. doi: 10.1007/BF02104457. [DOI] [PubMed] [Google Scholar]
- 9.Farges O, Daradkeh S, Bismth H. Cavernous haemangiomas of the liver: are there any indications for resection? World J Surg. 1995;19:19–24. doi: 10.1007/BF00316974. [DOI] [PubMed] [Google Scholar]
- 10.Pietrabiss A, Giullianotti P, Campatelli A, et al. Management and follow-up of 78 giant haemangiomas of the liver. Br J Surg. 1996;83:915–18. doi: 10.1002/bjs.1800830710. [DOI] [PubMed] [Google Scholar]
- 11.Brouwers MAM, Peeters PMJG, de Jong KP, et al. Surgical treatment of giant haemangioma of the liver. Br J Surg. 1997;84:314–16. [PubMed] [Google Scholar]
- 12.Rintoul R, O'Riordian MG, Laurenson IF, Crosbie JL, Allan PL, Garden OJ. Changing management of pyogenic liver abscess. Br J Surg. 1996;83:1215–18. [PubMed] [Google Scholar]
- 13.Huang CJ, Pitt H, Lipsett P, et al. Pyogenic hepatic abscess: changing trends over 42 years. Arm Surg. 1996;223:600–9. doi: 10.1097/00000658-199605000-00016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chou F, Sheen-Chen SM, Chen YS, Chen MC. Single and multiple pyogenic liver abscesses: clinical course, etiology and results of treatment. World J Surg. 1997;21:384–9. doi: 10.1007/pl00012258. [DOI] [PubMed] [Google Scholar]
- 15.Schmid A, Janig D, Bohuszlavizki A, Henne-Bruns D. Inflammatory pseudotumour of the liver presenting as incidentaloma: report of a case and review of the literature. Hepatogastroenterology. 1996;43:1009–14. [PubMed] [Google Scholar]
- 16.Zamir D, Jarchowsky J, Singer C, et al. Inflammatory pseudotumour of the liver – a rare entity and a diagnostic challenge. Am J Gastroenterol. 1998;93:1538–40. doi: 10.1111/j.1572-0241.1998.00476.x. [DOI] [PubMed] [Google Scholar]
- 17.Zavaglia C, Barberis M, Gelosa F, et al. Inflammatory pseudotumour of the liver with malignant transformation. Report of two cases. Ital J Gastroenterol. 1996;28:152–9. [PubMed] [Google Scholar]
- 18.John TG, Garden OJ. Needle track seeding of primary and secondary liver carcinoma after percutaneous liver biopsy. HPB Surg. 1993;6:199. doi: 10.1155/1993/39539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gerhards MF, Vos P, Van Gulik TM, Rauws EAJ, Gouma DJ. Incidence of benign lesions in patients resected for suspicious hilar obstruction. Br J Surg. 2001;88:48–51. doi: 10.1046/j.1365-2168.2001.01607.x. [DOI] [PubMed] [Google Scholar]
- 20.Clayton RAE, Clarke DL, Currie EJ, Madhavan KK, Parks RW, Garden OJ. Incidence of benign pathology in patients undergoing hepatic resection for suspected malignancy. J R Coll Surg Edin Ire. 2003;1:32–8. doi: 10.1016/s1479-666x(03)80006-9. [DOI] [PubMed] [Google Scholar]