Abstract
Background
Split liver transplantation offers an attractive way to increase the number of cadaveric grafts. In the past 10 years, it has enabled clinicians to minimise paediatric waiting list mortality. Two major concepts are applied in liver splitting. The more widely accepted approach provides a left lateral and a right extended liver graft to be transplanted into one child and one adult, respectively. To date the results from this technique are comparable to whole organ techniques for both the paediatric and the adult recipient. The second principle of splitting the liver provides two ‘full’ hemi-grafts-the left side for a small adult or big child and the right for a medium-sized adult patient. Full right/full left splitting is an important means of expanding the adult liver graft pool; however, it is a complex variant of liver transplantation that requires a high level of technical skill and a comprehensive knowledge of possible anatomic variations. Splitting for two adults should be performed in centres with a significant annual volume of liver transplantations, experience with left lateral splitting and an active program of hepatobiliary surgery. This brief review discusses anatomical and technical aspects and summarises the experience of both approaches to split liver transplantation to date.
Keywords: split liver transplantation, in situ, ex situ, review
Introduction
Orthotopic liver transplantation (OUT) has evolved from an experimental procedure to the treatment of choice for end-stage liver disease. New immunosuppressive regimens, refinements of surgical techniques, advances in tissue preservation and improvement of postoperative management account for the remarkable progress that has been made. Because of an increasing discrepancy between liver graft supply and demand, the death rate on the waiting list is currently estimated at an unacceptable level of 15–20% for Europe 1. In future years an epidemic increase of patients with hepatitis C cirrhosis (more than 1 million in the USA 2) is expected to dramatically worsen the imbalance of available organs and need 3.
To maximise cadaveric donor organ use for children and adults, split liver transplantation has been established. The basic difference between this approach and reduced-size liver transplantation is that both parts of the liver are suitable for transplantation. In 1989, Pichlmayr and colleagues were the first to report a case of transplanting one donor liver into two recipients 4. This technique and its variations serve the fundamental principle of dividing the whole liver into portions, each with a suitable vascular pedicle, bile duct and venous outflow, along with sufficient functional hepatic mass.
Two main types of split liver transplantation have to be distinguished. First there is the'classical' split, to achieve a right extended graft (segments I, IV–VIII) and a left lateral graft (segments II and III), for one adult and one small paediatric recipient. Secondly liver splitting along the line of Cantilie resulting in one right (segments V–VIII) and one left (segments I–IV) hemi-liver to supply two adult recipients can be performed. As experience, anatomical hurdles and purpose differ widely between these two main variations of split liver transplantation, they will be discussed separately in the following.
Which donors are suitable for liver splitting?
Only haemodynamically stable cadaveric donors are eligible for split liver transplantation. Donors for left lateral splitting should additionally meet the following criteria: age <55 years; fatty degeneration of the liver <30%; intensive care stay <5 days; Na <160mmol/L; serum glutamic pyruvic transaminase <60 U/L; gamma-glutamyl transpeptidase <50U/L. Organs from donors >70 kg of BW may be suitable for a full right/full left split, resulting in grafts for two adult recipients. Requirements of organ quality are more pronounced if a full right/full left split is intended (age <40 years, fatty degeneration <10%, ICU stay <3 days). Toso et al. determined that around 15% of donors fulfil such conditions for a split liver procedure, and about 9% could be eligible as donors for two adults 5. More optimistic calculations estimate up to 13% of donors being eligible for splitting for two adults 6. The final decision on whether the graft quality is sufficient for splitting is made on macroscopic criteria and ideally on the result of a liver biopsy. Performing the latter routinely would give centres the ability to undertake an external split graft with more confidence in organ quality.
The left lateral split
Alternative techniques to improve the graft supply for small children were pushed by an unacceptable mortality rate on the waiting list for paediatric patients suffering from end-stage liver disease, reaching up to 40% in the 1980s. Backed by growing confidence with transplantation of segmental grafts resulting either from size reduction of a whole adult cadaveric liver or adult-to-child living donation, left lateral splitting evolved like adult-to-paediatric living donation as an alternative to paediatric whole organ transplantation, thus reducing the need for living donation. Also, importantly, left lateral splitting does not compromise the adult graft pool, as the remaining extended right graft is suitable even for large adults without risking a small-for-size situation 7. Depending on its relatively highly variable weight, the left lateral segment can be utilised for recipients up to 40 kg of body weight. Since the first split liver transplantation by Pichlmayr et al.4 the ex situ and more recently the in situ splitting techniques 8 have been established and should be performed according to the logistical possibilities, as both may lead to comparably good results as long as optimal technique and choice of donors and recipients are ensured.
Technical Aspects
First the left side of the hepatoduodenal ligament is dissected to identify the left hepatic artery. The artery to segment IV can either stay in continuity with the main arterial trunk of the right graft depending on individual anatomy or has to be anastomosed with the stump of the left hepatic or gastroduodenal artery to minimise the risk of necrosis of segment IV 9. Then the left portal vein is dissected down to the main bifurcation. Portal branches to segments I and IV arising from the left main portal vein have to be transected. Dissection of the parenchyma is performed just to the right of the falciform ligament. In the ex situ technique the parenchyma can be cut sharply in a single even plane, leaving a flat surface, so that haemostasis may be achieved most efficiently. In the in situ technique any of the established techniques for liver resection, combined with vessel clipping and suture ligation of vessels, is suitable for transection of the parenchyma. This technique utilises the donor's coagulation system to achieve optimal haemostasis. A vessel loop placed around the left hepatic vein can guide the surgeon through the plane of transection between the middle and left hepatic vein during in situ splitting 10. Any dissection and isolation of the main left bile duct has to be avoided to save the parabiliary vascular plexus and the bile ducts of segments I and IV. The hilar plate, including the bile duct(s) to segments II and III, is sharply divided at the level of the longitudinal part of the left portal vein (Rex Recessus) (Figure 1). The left hepatic vein is divided adjacent to the vena cava. The right and middle hepatic veins stay in continuity with the vena cava with the right graft. To minimise the risk of bile leakage on the right graft every effort should be made, including intra-operative cholangiography if needed, to save the bile ducts draining segments I and IV.
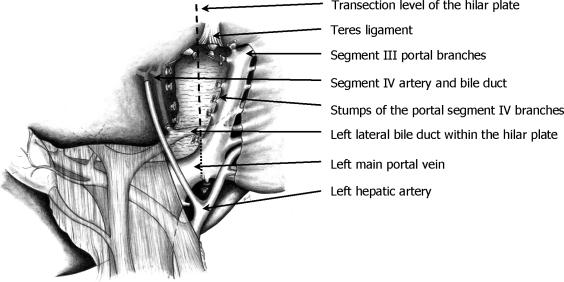
Figure 1. .
Anatomic situation after dissection of the portal branches to segment IV in the course of left lateral splitting. The left hilar plate behind the left portal vein is exposed. In most cases the bile duct(s) within the hilar plate can be seen. Sharp transection of the hilar plate (dashed line) should yield a short stump of the bile duct(s) from segments II and III (see text).
Results
Both left lateral living-related and split liver transplantation have reduced the mortality on the paediatric waiting list to <5% to date in our programme. Despite the fact that, from a surgical point of view, the whole graft seems to be the safest graft, split liver transplantations in children have yielded comparable results 3,11,12,13,14,15,16. Transplantation of a left lateral graft resulting from splitting of a cadaveric donor liver can also achieve comparable results with that of transplanting left lateral grafts from living donors 16,17. Therefore to avoid the risk to a living donor the first choice for a paediatric recipient should be a split liver graft in countries in which cadaveric livers are available.
It has been shown that transplantation of the right extended graft is not followed by a higher rate of surgical complications or an inferior level of patient and graft survival. Therefore the right extended graft can be considered as safe as the transplantation of a whole organ 11,18,19. Results as published by us and others are summarised in Table 1 [3, 13–15, 18, 20–33, Hamburg, unpublished data].
Table 1. Review of left lateral/extended right split liver series.
| Lead author | Year | Total no. | Graft survival (%) | Patient survival (%) |
|---|---|---|---|---|
| Edmond 20 | 1990 | 18 | 52 | 67 |
| Shaw 21 | 1990 | 10 | 50 | 50 |
| Broelsch 22 | 1990 | 30 | – | 60 |
| Langnas 23 | 1992 | 10 | – | 50 |
| Houssin 24 | 1993 | 16 | 69 | 75 |
| Sloof 25 | 1995 | 15 | 67 | 73 |
| Otte 26 | 1995 | 29 | 67 | 71 |
| De Ville de Goyet 27 (European analysis) | 1995 | 98 | – | 68 |
| Azoulay 28 | 1996 | 27 | 78.4 | 79.5 |
| Rogiers 29(exlin situ) | 1996 | 19/14 | 58/86 | 63/93 |
| Kalayoglu 30 | 1996 | 12 | 75 | 91.6 |
| Goss 31(in situ) | 1997 | 28 | 86 | 92 |
| Rela[l8] | 1998 | 41 | 88 | 90 |
| Mirza 13 | 1998 | 24 | 68 | 78 |
| Chardot 32 (incl. two segments II–IV) | 1999 | 16 | 62 | 66.7 |
| Sindhi 33 (UNOS analysis) | 1999 | 89 | 60.3 | 82 |
| Ghobrial 3(in situ; right/left) | 2000 | 110 | – | 80/76 |
| Spada 15 (right/left) | 2000 | 42/42 | 79/ | 84/85 |
| Reyes 14(exlin situ) | 2000 | 25/29 | 61/81 | 74/96 |
| Hamburg (unpublished data) | 2002 | 171 | 78.4 | 85.6 |
Full right/full left splitting
In contrast to organ shortage in small paediatric patients, which has been dramatically reduced with'routine' application of living donation and left lateral splitting, the organ shortage for older children and adult patients is rather getting worse. Bismuth et al. were the first to report the use of one donor liver for two adult patients in 1989 34. Although the concept of living-related adult-to-adult liver transplantation has been followed in depth over the past 5 years, full right/full left splitting is still an important means of expanding the adult liver graft pool, thus reducing the need for a living donor, with the inherent risks of that approach. The former technique provides two grafts from one liver for a small adult or large child (segments (I), II–IV) and for a medium-sized adult patient (segments V–VIII).
Full right/full left split liver transplantation is a complex variant of liver transplantation that requires high levels of technical skill and a comprehensive knowledge of possible anatomic variations that may present a contraindication to the procedure. The latter may necessitate a switch to a left lateral split procedure. Splitting for two adults should be performed in centres that carry out a significant number of liver transplantations each year, with experience of left lateral splitting and that incorporate an active programme of hepatobiliary surgery.
Technical Aspects
The technical difficulties in split liver transplantation for two adults are focused mainly on two questions: how to share the blood vessels, especially the hepatic veins and vena cava, and how to achieve safe biliary drainage of all segments transplanted. Major differences to left lateral splitting are the absence of an anatomic structure indicating the line of resection (like the falciform ligament), a larger transection plane, and a substantially higher chance of disturbing vascularisation and bile drainage of the transplanted segments.
In this scenario, in situ splitting has the advantage of identification of the optimal dissection plane by performing a short inflow occlusion of one hemi-liver. After parenchymal transection, sufficient portal and arterial inflow as well as venous outflow (especially of segments V and VIII), can be assured before perfusion. At the end of this procedure perfect haemostasis and biliostasis of the cut section can be obtained with the help of the donor's coagulation system.
Intraoperative cholangiography helps to identify anatomical bile duct variations, which may either indicate a switch to a left lateral splitting procedure or may totally prohibit liver splitting 9. The decision whether to leave the common bile duct to the left or right hemi-liver depends on the individual anatomy. In most instances the common bile duct should stay with the right graft, as the right main bile duct is shorter than the left and anatomical variations of the bile ducts are more frequent within the right lobe. The bile ducts should be shortened as much as possible to ensure sufficient perfusion.
Some authors recommend an arteriography 35, but in most cases arterial anatomy can be safely identified by hilar dissection. Sharing of the arterial trunk depends on the individual anatomy of the donor, especially the origin of the segment IV artery. In most cases the main arterial trunks stays with the left graft.
In conventional techniques, usually the middle hepatic vein is retained with the left graft and the vena cava with the right graft. The indispensable division of the caudate lobe veins lead to uncertain viability of liver segment I, and resection might be necessary. To provide optimal venous drainage of both hemi-liver grafts, we developed the split cava technique 36, which involves the division of the vena cava, maintaining venous drainage of segment I and the dorsal parts of the right lobe via retrohepatic veins. However, the split cava technique does not prevent venous congestion of segments V and VIII if the middle hepatic vein stays with the left graft. Additional venous reconstruction of these veins on the cut surface is necessary (Figure 2).
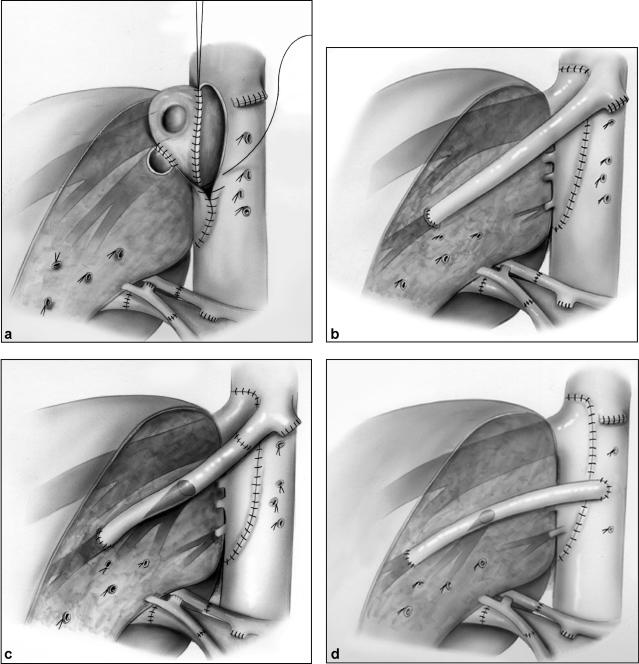
Figure 2. .
Different strategies to optimise venous drainage of segments V and VIII subsequent to full right/full left splitting. Beyond right and segment VIII vein from cut surface re-anastomoses, outflow via short retrohepatic veins is assured by utilising the right cava patch subsequent to the cava split technique (a). Venous branches that lead in the parenchymal transection plane should, if >5 mm in diameter, be reconstructed via the recipients own middle hepatic vein without (b) or with (c) interpositioning graft Alternatively, a graft can be interposed between the stump of segments V and VIII veins and the recipient's cava (d).
Results
In contrast to splitting a liver for a child and an adult, only small series of full right/full left splitting are published. Increased morbidity and poor initial results, especially after grafting of the left hemi-liver, have prevented a wider acceptance of this technique (Table 2) [35,37–40, Hamburg, unpublished data]. The main hurdles for expanding this technique seem to be the high technical and logistical requirements, as well as the worry of a small-for-size situation evolving subsequent to full right/full left splitting for two adult recipients. The key aspects to obtaining results for full right/full left split liver transplantation that are as good as those following whole organ transplantation are: adequate technical skills, a reliable judgement on graft quality and an optimal graft-recipient size match.
Table 2. Review of reports on full right/full left split liver experience.
| Lead author | Year | Total no. | Graft survival (%) | Patient survival (%) |
|---|---|---|---|---|
| Colledan 37 | 2000 | 6 | 66.6 | 83.3 |
| Sommacale 38 | 2000 | 2 | 100 | 100 |
| Kilic 39 | 2001 | 2 | 100 | 100 |
| Humar 40(in situ) | 2001 | 12 | 83.3 | 83.3 |
| Azoulay 35 (right/left) (24 grafts shared segment. IV) | 2001 | 34 | 74/75 | 74/88 |
| Hamburg (7 right/9 left) (unpublished data) | 2002 | 16 | 80 | 86 |
Graft quality has to be evaluated by an experienced split liver transplantation surgeon, supported by a liver biopsy, if available. The donor requirements are higher compared with left lateral splitting (see above).
The choice of the recipient should respect the relationship of absolute transplantable functional liver mass and the needs of the individual recipient. In general the recipient should receive a split liver mass exceeding 1.2% of body weight. With worsening general condition of the recipient functional liver mass needs to be increased even further. Only in elective cases without portal hypertension this limit may be surpassed on individual decisions. Therefore donor and recipient selection are vital and do not tolerate any compromise.
Conclusion
Splitting one liver in a left lateral and a right extended graft for one paediatric and adult recipient has been shown to yield comparable results to whole organ transplantation and is therefore widely accepted as an alternative to a whole graft. Split liver transplantation for two adult recipients is still a challenging procedure; however, it has the potential to reduce mortality on the adult waiting list. The latest results with this technique are encouraging. Administrative accommodations in the current methods of organ allocation to ensure optimal combinations of graft and recipient will be needed if split liver transplantation in adults is to succeed. A nationwide view of organ allocation requires that the total number of lives saved by the procedure be the priority outcome. If liver transplantation is viewed from this perspective, split liver transplantation for adults is a high priority, and incentives should be set to encourage it. Despite the fact that in situ splitting seems to have certain advantages concerning graft quality and subsequent recipient operation and course, logistical circumstances may favour ex situ splitting in selected cases.
Experience with split liver transplantation is growing and it may be foreseen that, one day, splitting for two adult recipients will become established routine. Grafting two patients with one cadaveric donor is the ultimate way of meeting the liver organ shortage, without the risks associated with using a living donor and therefore must be further followed and established.
References
- 1.Stellingwerff GC, et al. The liver transplant waiting list. A competing risk (cr) analysis of mortality and transplant probabilities. In: Program and Abstracts of the 18th Annual Scientific Meeting of the American Society of Transplantation (AST)1999;A346 [Google Scholar]
- 2.Liang TJ, Rehermann B, Seef LB, Hoofnagle JH. Pathogenesis, natural history, treatment, and prevention of hepatitis C. Ann Intern Med. 2000;132:296–305. doi: 10.7326/0003-4819-132-4-200002150-00008. [DOI] [PubMed] [Google Scholar]
- 3.Ghobrial RM, Yersiz H, Farmer DG, et al. Predictors of survival after in vivo split liver transplantation: analysis of 110 consecutive patients. Ann Surg. 2000;232:312–23. doi: 10.1097/00000658-200009000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pichlmayr R, Ringe B, Gubernatis G, Hauss J, Bunzendahl H. Transplantation of a donor liver to 2 recipients (splitting transplantation)-a new method in the further development of segmental liver transplantation. Langenbecks Arch Chir. 1988;373:127–30. [PubMed] [Google Scholar]
- 5.Toso C, Ris F, Mentha G, Oberholzer J, Morel P, Majno P. Potential impact of in situ liver splitting on the number of available grafts. Transplantation. 2002;74:222–6. doi: 10.1097/00007890-200207270-00013. [DOI] [PubMed] [Google Scholar]
- 6.Poncet G, Dumortier J, Choucair A, et al. Split-liver transplantation in two adult recipients: evaluation of feasibility in 100 consecutive cadaver liver grafts. Gastroenterol Clin Biol. 2002;26:578–83. [PubMed] [Google Scholar]
- 7.Gridelli B, Perico N, Remuzzi G. Strategies for a greater supply of organs for transplantation. Recent Prog Med. 2001;92:9–15. [PubMed] [Google Scholar]
- 8.Rogiers X, Malago M, Habib N, et al. In situ splitting of the liver in the heart-beating cadaveric organ donor for trans plantation in two recipients. Transplantation. 1995;59:1081–3. [PubMed] [Google Scholar]
- 9.Broering DC, Schulte am Esch J, Rogiers X. Rogiers X, Bismuth H, Busuttil RW, Broering DC, Azoulay D. Steinkopff Verlag; Darmstadt: 2002. Consequences of anatomy on split-liver transplantation, Split liver Transplantation-Theoretical and Practical Aspects; pp. 46–62. [Google Scholar]
- 10.Broering DC, Rogiers X, Malago M, Bassas A, Broelsch CE. Vessel loop-guided technique for parenchymal transection in living donor or in situ split-liver procurement. liver Transpl Surg. 1998;4:241. doi: 10.1002/lt.500040304. [DOI] [PubMed] [Google Scholar]
- 11.Busuttil RW, Goss JA. Split liver transplantation. Ann Surg. 1999;229:313–21. doi: 10.1097/00000658-199903000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Reding R, Gennari F, Janssen M, et al. The pediatric liver transplant program at the Universite Catholique de Louvain, Cliniques Saint-Luc, Brussels: overall results in 444 children 1984–1997. Acta Gastroenterol Belg. 1999;62:285–9. [PubMed] [Google Scholar]
- 13.Mirza DF, Achilleos O, Pirenne J, Buckels JA, McMaster P, Payer AD. Encouraging results of split-liver transplantation. Br J Surg. 1998;85:494–7. doi: 10.1046/j.1365-2168.1998.00605.x. [DOI] [PubMed] [Google Scholar]
- 14.Reyes J, Gerber D, Mazariegos GV, et al. Split-liver transplantation: a comparison of ex vivo and in situ techniques. J Pediatr Surg 2000;35:283–9; discussion 289–90. [DOI] [PubMed] [Google Scholar]
- 15.Spada M, Gridelli B, Colledan M, et al. Extensive use of split liver for pediatric liver transplantation: a single-center experience. liver Transpl. 2000;6:415–28. doi: 10.1053/jlts.2000.7570. [DOI] [PubMed] [Google Scholar]
- 16.Broering DC, Mueller L, Ganschow R, et al. Is there still a need for living-related liver transplantation in children? Ann Surg 2001;234:713–21; discussion 721–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Farmer DG, Yersiz H, Ghobrial RM, et al. Early graft function after pediatric liver transplantation: comparison between in situ split liver grafts and living-related liver grafts. Transplantation. 2001;72:1795–802. doi: 10.1097/00007890-200112150-00015. [DOI] [PubMed] [Google Scholar]
- 18.Rela M, Vougas V, Muiesan P, et al. Split liver transplantation: King's College Hospital experience. Ann Surg. 1998;227:282–8. doi: 10.1097/00000658-199802000-00019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Broering DC, Topp S, Schaefer U, et al. Split liver transplantation and risk to the adult recipient: analysis using matched pairs. J Am Coll Surg. 2002;195:648–57. doi: 10.1016/s1072-7515(02)01339-x. [DOI] [PubMed] [Google Scholar]
- 20.Emond JC, Whitington PF, Thistlethwaite JR, et al. Transplantation of two patients with one liver. Analysis of a preliminary experience with'split-liver' grafting. Arm Surg. 1990;212:14–22. doi: 10.1097/00000658-199007000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shaw BW, Jr, Wood RP, Stratta RJ, et al. Management of arterial anomalies encountered in split-liver transplantation. Transplant Proc. 1990;22:420–2. [PubMed] [Google Scholar]
- 22.Broelsch CE, Emond JC, Whitington PF, Thistlethwaite JR, Baker A, Lichtor JL. Application of reduced-size liver transplants as split grafts, auxiliary orthotopic grafts, and living related segmental transplants. Arm Surg 1990;212: 368–75; discussion 375–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Langnas AN, Marujo WC, Inagaki M, Stratta RJ, Wood RP, Shaw BW., Jr The results of reduced-size liver trans plantation, including split livers, in patients with end-stage liver disease. Transplantation. 1992;53:387–91. doi: 10.1097/00007890-199202010-00023. [DOI] [PubMed] [Google Scholar]
- 24.Houssin D, Boillot O, Soubrane O, et al. Controlled liver splitting for transplantation in two recipients: technique, results and perspectives. Br J Surg. 1993;80:75–80. doi: 10.1002/bjs.1800800126. [DOI] [PubMed] [Google Scholar]
- 25.Slooff MJ. Reduced size liver transplantation, split liver transplantation, and living related liver transplantation in relation to the donor organ shortage. Transpl lnt. 1995;8:65–8. doi: 10.1007/BF00366715. [DOI] [PubMed] [Google Scholar]
- 26.Otte JB. Is it right to develop living related liver trans plantation? Do reduced and split livers not suffice to cover the needs? Transpl lnt. 1995;8:69–73. doi: 10.1007/BF00366716. [DOI] [PubMed] [Google Scholar]
- 27.de Ville de Goyet J. Split liver transplantation in Europe – 1988 to 1993. Transplantation ; 1995;59:1371–6. doi: 10.1097/00007890-199505270-00002. [DOI] [PubMed] [Google Scholar]
- 28.Azoulay D, Astarcioglu I, Bismuth H, et al. Split-liver transplantation. The Paul Brousse policy. Arm Surg 1996; 224:737–46; discussion 746–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rogiers X, Malago M, Gawad K, et al. In situ splitting of cadaveric livers. The ultimate expansion of a limited donor pool. Ann Surg 1996;224:331–9; discussion 339–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kalayoglu M, d'Alessandro AM, Knechtle SJ, et al. Preliminary experience with split liver transplantation. J Am Coll Surg. 1996;182:381–7. [PubMed] [Google Scholar]
- 31.Goss JA, Yersiz H, Shackleton CR, et al. In situ splitting of the cadaveric liver for transplantation. Transplantation. 1997;64:871–7. doi: 10.1097/00007890-199709270-00014. [DOI] [PubMed] [Google Scholar]
- 32.Chardot C, Branchereau S, de Dreuzy O, et al. Paediatric liver transplantation with a split graft: experience at Bicetre. Eur J Pediatr Surg. 1999;9:146–52. doi: 10.1055/s-2008-1072231. [DOI] [PubMed] [Google Scholar]
- 33.Sindhi R, Rosendale J, Mundy D, et al. Impact of segmental grafts on pediatric liver transplantation-a review of the United Network for Organ Sharing Scientific Registry data (1990–1996). J Pediatr Surg 1999;34:107–10; discussion 110–11. [DOI] [PubMed] [Google Scholar]
- 34.Bismuth H, Morino M, Castaing D, et al. Emergency orthotopic liver transplantation in two patients using one donor liver. Br J Surg. 1989;76:722–4. doi: 10.1002/bjs.1800760723. [DOI] [PubMed] [Google Scholar]
- 35.Azoulay D, Casating D, Adam R, et al. Split-liver trans plantation for two adult recipients: feasibility and long-term outcomes. Ann Surg. 2001;233:565–74. doi: 10.1097/00000658-200104000-00013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gundlach M, Broering D, Topp S, Sterneck M, Rogiers X. Split-cava technique: liver splitting for two adult recipients. liver Transpl. 2000;6:703–6. doi: 10.1053/jlts.2000.18503. [DOI] [PubMed] [Google Scholar]
- 37.Colledan M, Segalin A, Andorno E, et al. Modified splitting technique for liver transplantation in adult-sized recipients. Technique and preliminary results. Ada Chir Belg. 2000;100:289–91. [PubMed] [Google Scholar]
- 38.Sommacale D, Farges O, Ettorre GM, et al. In situ split liver transplantation for two adult recipients. Transplantation. 2000;69:1005–7. doi: 10.1097/00007890-200003150-00060. [DOI] [PubMed] [Google Scholar]
- 39.Kilic M, Seu P, Stribling RJ, Ghalib R, Goss JA. In situ splitting of the cadaveric liver for two adult recipients. Transplantation. 2001;72:1853–8. doi: 10.1097/00007890-200112150-00028. [DOI] [PubMed] [Google Scholar]
- 40.Humar A, Ramcharan T, Sielaff TD, et al. Split liver transplantation for two adult recipients: an initial experience. Am J Transplant. 2001;1:366–72. doi: 10.1034/j.1600-6143.2001.10413.x. [DOI] [PubMed] [Google Scholar]